Abstract
Background
The Lancet Commission on Global Surgery (LCoGS) described the lack of access to safe, affordable, timely surgical, and anesthesia care. It proposed a series of 6 indicators to measure surgery, accompanied by time-bound targets and a template for national surgical planning. To date, no sub-Saharan African country has completed and published a nationwide evaluation of its surgical system within this framework.
Method
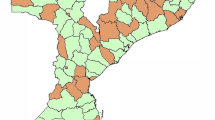
Mercy Ships, in partnership with Harvard Medical School and the Madagascar Ministry of Health, collected data on the 6 indicators from 22 referral hospitals in 16 out of 22 regions of Madagascar. Data collection was by semi-structured interviews with ministerial, medical, laboratory, pharmacy, and administrative representatives in each region. Microsimulation modeling was used to calculate values for financial indicators.
Results
In Madagascar, 29% of the population can access a surgical facility within 2 h. Surgical workforce density is 0.78 providers per 100,000 and annual surgical volume is 135–191 procedures per 100,000 with a perioperative mortality rate of 2.5–3.3%. Patients requiring surgery have a 77.4–86.3 and 78.8–95.1% risk of incurring impoverishing and catastrophic expenditure, respectively. Of the six LCoGS indicator targets, Madagascar meets one, the reporting of perioperative mortality rate.
Conclusion
Compared to the LCoGS targets, Madagascar has deficits in surgical access, workforce, volume, and the ability to offer financial risk protection to surgical patients. Its perioperative mortality rate, however, appears better than in comparable countries. The government is committed to improvement, and key stakeholder meetings to create a national surgical plan have begun.
Similar content being viewed by others
References
Bickler SN, Weiser TG, Kassebaum N et al (2015) Global burden of surgical conditions. In: Debas HT, Donkor P, Gawande A, Jamison DT, Kruk ME, Mock CN (eds) Essential surgery: disease control priorities, vol 1, 3rd edn. The International Bank for Reconstruction and Development/The World Bank, Washington DC
Farmer PE, Kim JY (2008) Surgery and global health: a view from beyond the OR. World J Surg 32(4):533–536. doi:10.1007/s00268-008-9525-9
Alkire BC, Raykar NP, Shrime MG et al (2015) Global access to surgical care: a modelling study. Lancet Glob health 3(6):e316–e323
Rose J, Weiser TG, Hider P et al (2015) Estimated need for surgery worldwide based on prevalence of diseases: a modelling strategy for the WHO Global Health Estimate. Lancet Glob Health 3:S13–S20
Shrime MG, Dare AJ, Alkire BC et al (2015) Catastrophic expenditure to pay for surgery worldwide: a modelling study. Lancet Glob health 3(Suppl. 2):S38–S44
Alkire BC, Shrime MG, Dare AJ et al (2015) Global economic consequences of selected surgical diseases: a modelling study. Lancet Glob Health 3(Suppl. 2):S21–S27
Meara JG, Leather AJ, Hagander L et al (2015) Global surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet 386(9993):569–624
World Bank. Subnational Population database World Bank 2014. http://databank.worldbank.org/data/reports.aspx?source=subnational-population
Xu K, Evans DB, Carrin G et al (2007) Protecting households from catastrophic health spending. Health Aff (Millwood) 26(4):972–983
Uribe-Leitz T, Jaramillo J, Maurer L et al (2016) Variability in mortality following caesarean delivery, appendectomy, and groin hernia repair in low-income and middle-income countries: a systematic review and analysis of published data. Lancet Glob health 4(3):e165–e174
The Global Surgery Collaborative (2016) Mortality of emergency abdominal surgery in high-, middle- and low-income countries. Br J Surg 103(8):971–988
Dubowitz G, Detlefs S, McQueen KA (2010) Global anesthesia workforce crisis: a preliminary survey revealing shortages contributing to undesirable outcomes and unsafe practices. World J Surg 34(3):438–444. doi:10.1007/s00268-009-0229-6
Hoyler M, Finlayson SR, McClain CD et al (2014) Shortage of doctors, shortage of data: a review of the global surgery, obstetrics, and anesthesia workforce literature. World J Surg 38(2):269–280. doi:10.1007/s00268-013-2324-y
McQueen K, Coonan T, Ottaway A et al (2015) The bare minimum: the reality of global anaesthesia and patient safety. World J Surg 39(9):2153–2160. doi:10.1007/s00268-015-3101-x
Madagascar awards medals to Chinese doctors. Peoples Daily Online 2010
Baird R, Poenaru D, Ganey M et al (2016) Partnership in fellowship: comparative analysis of pediatric surgical training and evaluation of a fellow exchange between Canada and Kenya. J Pediatr Surg. doi:10.1016/j.jpedsurg.2016.06.002
Chao TE, Riesel JN, Anderson GA et al (2015) Building a global surgery initiative through evaluation, collaboration, and training: the Massachusetts General Hospital experience. J Surg Educ 72(4):e21–e28
Monroe-Wise A, Kibore M, Kiarie J et al (2014) The clinical education partnership initiative: an innovative approach to global health education. BMC Med Educ 14:1043
Ndenga E, Uwizeye G, Thomson DR et al (2016) Assessing the twinning model in the Rwandan human resources for health program: goal setting, satisfaction and perceived skill transfer. Glob Health 12:4
Ulisubisya M, Jornvall H, Irestedt L et al (2016) Establishing an anaesthesia and intensive care partnership and aiming for national impact in Tanzania. Glob Health 12:7
Jones A (2016) Envisioning a global health partnership movement. Glob Health 12(1):1
Edwards S, Ritman D, Burn E et al (2015) Towards a simple typology of international health partnerships. Glob Health 11:49
Kelly E, Doyle V, Weakliam D et al (2015) A rapid evidence review on the effectiveness of institutional health partnerships. Glob Health 11:48
Kannan VC, Andriamalala CN, Reynolds TA (2015) The burden of acute disease in Mahajanga, Madagascar—a 21 month study. PLoS ONE 10(3):e0119029
Honda A, Randaoharison PG, Matsui M (2011) Affordability of emergency obstetric and neonatal care at public hospitals in Madagascar. Reprod Health Matters 19(37):10–20
Chirdan LB, Ameh EA, Abantanga FA et al (2010) Challenges of training and delivery of pediatric surgical services in Africa. J Pediatr Surg 45(3):610–618
World-Bank. Madagascar Country Profile. 2016. http://www.worldbank.org/en/country/madagascar
Lin BM, White M, Glover A, et al (2016) Barriers to surgical care and health outcomes: a prospective study on the relation between wealth, sex, and postoperative complications in the Republic of Congo. World J Surg. doi:10.1007/s00268-016-3676-x
Ng-Kamstra JS, Greenberg SL, Kotagal M et al (2015) Use and definitions of perioperative mortality rates in low-income and middle-income countries: a systematic review. Lancet 385(Suppl. 2):S29
Acknowledgements
E. Bruno received funding for International travel by Boston Children’s Hospital, Boston, MA, USA, and from the Mark Allen McConkey, M.D., Medical Student Public Service Fund. L. S. Baxter received a travel and education Grant from the National Institute for Academic Anaesthesia, UK. M. G. Shrime receives funding from the GE foundation for its Safe Surgery 2020 initiative.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
M. C. White, V. A. Ravelojaona, H. N. Rakotoarison, H. H. Andriamanjato, K. L. Close, A. Herbert, N. Raykar and S. Saluja have no conflicts of interest to declare.
Additional information
Emily Bruno and Michelle C. White serve as the lead authors of this article.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Bruno, E., White, M.C., Baxter, L.S. et al. An Evaluation of Preparedness, Delivery and Impact of Surgical and Anesthesia Care in Madagascar: A Framework for a National Surgical Plan. World J Surg 41, 1218–1224 (2017). https://doi.org/10.1007/s00268-016-3847-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-016-3847-9