Abstract
Background
Access to safe surgery is critical to health, welfare, and economic development. In 2015, the Lancet Commission on Global Surgery recommended that all countries collect surgical indicators to lend insight into improving surgical care. No nationwide high-quality data exist for these metrics in Uganda.
Methods
A standardized quantitative hospital assessment and a semi-structured interview were administered to key stakeholders at 17 randomly selected public hospitals. Hospital walk-throughs and retrospective reviews of operative logbooks were completed.
Results
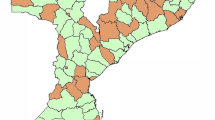
This study captured information for public hospitals serving 64.0% of Uganda’s population. On average, <25% of the population had 2 h access to a surgically capable facility. Hospitals averaged 257 beds/facilities and there were 0.2 operating rooms per 100,000 people. Annual surgical volume was 144.5 cases per 100,000 people per year. Surgical, anesthetic, and obstetrician physician workforce density was 0.3 per 100,000 people. Most hospitals reported having electricity, oxygen, and blood available more than half the time and running water available at least three quarters of the time. In total, 93.8% of facilities never had access to a CT scan. Sterile gloves, nasogastric tubes, and Foley catheters were frequently unavailable. Uniform outcome reporting does not exist, and the WHO safe surgery checklist is not utilized.
Conclusion
The Ugandan public hospital system does not meet LCoGS targets for surgical access, workforce, or surgical volume. Critical policy and programmatic developments are essential to build surgical capacity and facilitate provision of safe, timely, and affordable surgical care. Surgery must become a public health priority in Uganda and other low resource settings.





Similar content being viewed by others
References
Meara JG, Leather AJM, Hagander L et al (2015) Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet 386:569–624
Alkire BC, Raykar NP, Shrime MG et al (2015) Global access to surgical care: a modelling study. Lancet Glob Health 3:316–323
Raykar NP, Ng-kamstra JS, Bickler S et al (2017) New global surgical and anaesthesia indicators in the World Development Indicators dataset. BMJ Glob Health 2(2):e000265. https://doi.org/10.1136/bmjgh-2016-000265
Ministry of Health (2016) Annual Health Sector Performance Report 2015/2016
Ministry of Health (2012) Health facilities inventory. Kampala, Uganda. http://library.health.go.ug/publications/health-infrastructure-physical-infrastructure/health-facility-inventory. Accessed 1 Aug 2016
Dare AJ, Bleicher J, Lee KC et al (2015) Generation of national political priority for surgery: a qualitative case study of three low-income and middle-income countries. Lancet 385(Suppl):S54
Linden AF, Sekidde FS, Galukande M et al (2012) Challenges of surgery in developing countries: a survey of surgical and anesthesia capacity in Uganda’s public hospitals. World J Surg 36:1056–1065. https://doi.org/10.1007/s00268-012-1482-7
Luboga S, Galukande M, Mabweijano J (2010) Key aspects of health policy development to improve surgical services in Uganda. World J Surg 34:2511–2517. https://doi.org/10.1007/s00268-010-0585-2
Butler EK, Tran TM, Fuller AT, Brammell A (2016) Quantifying the pediatric surgical need in Uganda: results of a nationwide cross-sectional, household survey. Pediatr Surg Int 32:1075–1085
Farber SH, Ricardo J, Vissoci N et al (2017) Geospatial analysis of unmet surgical need in Uganda: an analysis of SOSAS survey data. World J Surg 41:353–363. https://doi.org/10.1007/s00268-016-3689-5
Tran TM, Fuller AT, Butler EK et al (2017) Burden of surgical conditions in Uganda. Ann Surg 266:389–399
Anderson GA, Ilcisin L, Abesiga L et al (2017) Surgical volume and postoperative mortality rate at a referral hospital in Western Uganda: measuring the Lancet commission on global surgery indicators in low-resource settings. Surgery (United States) 161:1710–1719
Harvard Humanitarian Initiative KoboToolbox. http://www.kobotoolbox.org/. Accessed 1 Aug 2016
Albutt K, Namanya D, Anderson G, Kayima P (2017) Uganda. In: Johnson W, Lin Y, Mukhopadhyay S, Meara J (eds) Surgical care systems strengthening: developing national surgical, obstetric and anaesthesia plans. World Health Organization, Geneva
Bruno E, White MC, Baxter LS et al (2017) An evaluation of preparedness, delivery and impact of surgical and anesthesia care in madagascar: a framework for a national surgical plan. World J Surg 41:1218–1224. https://doi.org/10.1007/s00268-016-3847-9
Raykar NP, Bowder AN, Liu C et al (2015) Geospatial mapping to estimate timely access to surgical care in nine low-income and middle-income countries. Lancet 385:S16
Ozgediz D, Kijjambu S, Galukande M et al (2008) Africa’s neglected surgical workforce crisis. Lancet 371:627–628
Petroze RT, Nzayisenga A, Rusanganwa V et al (2012) Comprehensive national analysis of emergency and essential surgical capacity in Rwanda. Br J Surg 99:436–443
Ozgediz D, Galukande M, Mabweijano J et al (2008) The neglect of the global surgical workforce: experience and evidence from Uganda. World J Surg 32:1208–1215. https://doi.org/10.1007/s00268-008-9473-4
Galukande M, Kaggwa S, Sekimpi P et al (2013) Use of surgical task shifting to scale up essential surgical services: a feasibility analysis at facility level in Uganda. BMC Health Serv Res 13:292
Knowlton LM, Chackungal S, Dahn B et al (2013) Liberian surgical and anesthesia infrastructure: a survey of county hospitals. World J Surg 37:721–729. https://doi.org/10.1007/s00268-013-1903-2
Carlson LC, Lin JA, Ameh EA et al (2015) Moving from data collection to application: a systematic literature review of surgical capacity assessments and their applications. World J Surg 39(4):813–821. https://doi.org/10.1007/s00268-014-2938-8
LeBrun DG, Chackungal S, Chao TE et al (2014) Prioritizing essential surgery and safe anesthesia for the post-2015 development agenda: operative capacities of 78 district hospitals in 7 low- and middle-income countries. Surgery 155:365–373
Raykar NP, Yorlets RR, Liu C et al (2016) The how project: understanding contextual challenges to global surgical care provision in low-resource settings. BMJ Glob Health 1:e000075
Nwanna-Nzewunwa OC, Ajiko M-M, Kirya F et al (2016) Barriers and facilitators of surgical care in rural Uganda: a mixed methods study. J Surg Res 204(1):242–250. https://doi.org/10.1016/j.jss.2016.04.051
Henry JA, Windapo O, Nwomeh BC (2012) A survey of surgical capacity in rural southern Nigeria: opportunities for change. World J Surg 36(12):2811–2818. https://doi.org/10.1007/s00268-012-1764-0
Acknowledgments
We are grateful to our collaborating partners and the hospitals and staff that participated in this assessment. Many thanks in particular to our colleagues at MOH whose partnership ensured a comprehensive evaluation, access to facilities, and applicability and accessibility of results at the country level. Funding was provided by the MGH Global Surgery Fund, MGH Center for Global Health, and Program in Global Surgery and Social Change.
Funding
Funding for this research was provided by the MGH Global Surgery Fund, MGH Center for Global Health, and Program in Global Surgery and Social Change.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest
Appendix: statistics
Appendix: statistics
Relationship between access to bellwether facility and region
-
Ho = no relationship between access to bellwether facility and region
-
Ha = relationship between access to bellwether facility and region
-
Test = Fisher’s exact test
Relationship between hospital type and medications (composite score)
-
Ho = no relationship between hospital type and medications (composite score)
-
Ha = relationship between hospital type and medications (composite score)
-
Test = Fisher’s exact test
-
Relationship between hospital type and blood
-
Ho = no relationship between hospital type and blood
-
Ha = relationship between hospital type and blood
-
Test = Fisher’s exact test
Relationship between operative volume (absolute and relative) and the type of hospital
-
Ho = no relationship between hospital type and operative volume
-
Ha = relationship between hospital type and operative volume
-
Test = two-sample t test
Rights and permissions
About this article
Cite this article
Albutt, K., Punchak, M., Kayima, P. et al. Access to Safe, Timely, and Affordable Surgical Care in Uganda: A Stratified Randomized Evaluation of Nationwide Public Sector Surgical Capacity and Core Surgical Indicators. World J Surg 42, 2303–2313 (2018). https://doi.org/10.1007/s00268-018-4485-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-018-4485-1