Abstract
Efforts have been made to strengthen national health systems for safe, affordable, and timely surgical, obstetric, trauma, and anesthesia (SOTA) care since 2015 when the Lancet Commission on Global Surgery (LCoGS) identified critical needs in improving access to essential surgical care for five billion people worldwide. Several governments have developed National Surgical, Obstetric, and Anesthesia Plans (NSOAPs) as a commitment to ensuring safe and accessible surgical care for all of their population. The Ministry of Public Health (MoPH) of Madagascar launched its NSOAP in May 2019, named Le Plan National de Développement de la Chirurgie a Madagascar (PNDCHM). This policy established Madagascar as the first African francophone country to define concrete objectives for the Malagasy health system to meet the targets set by the LCoGS by 2030. The PNDCHM outlined the following priorities and specific action points to be implemented from 2019 to 2023: improving technical capacity, training human resources, developing a health information system, ensuring adequate governance and leadership, offering quality care, creating specific surgical services, and financing and mobilizing resources for implementation. Challenges encountered in the process included complex coordination between different stakeholders, allocating a sufficient budget for its implementation, frequent turnover within the MoPH, and the COVID-19 pandemic. The PNDCHM is a first of its kind in francophone Africa and the many lessons learned can serve as guidance for countries aspiring to build NSOAPs of their own.
Résumé
Des efforts ont été déployés pour renforcer les systèmes de santé nationaux pour des soins chirurgicaux, obstétricaux, traumatologiques et anesthésiques sécuritaires, abordables et lorsque nécessaires depuis 2015, lorsque la Commission Lancet sur la chirurgie mondiale (LCoGS) a identifié des besoins critiques pour améliorer l’accès aux soins chirurgicaux essentiels pour cinq milliards de personnes dans le monde. Plusieurs gouvernements ont élaboré des Plans nationaux pour des soins en chirurgie, d’obstétrique et anesthésie (PNCOA) dans le but d’assurer des soins chirurgicaux sécuritaires et accessibles à l’ensemble de leur population. En mai 2019, le ministère de la Santé publique de Madagascar a lancé son propre PNCOA, baptisé Le Plan National de Développement de la Chirurgie à Madagascar (PNDChM). Cette politique a fait de Madagascar le premier pays africain francophone à définir des objectifs concrets pour que le système de santé malgache atteigne les cibles fixées par la Commission Lancet d’ici 2030. Le PNDChM a défini les priorités et points d’action spécifiques suivants à mettre en œuvre de 2019 à 2023 : amélioration des plateaux techniques, formation des ressources humaines, développement d’un système d’information sanitaire, bonne gouvernance et leadership, offre de soins de qualité, création de services chirurgicaux spécialisés, et financement et mobilisation des ressources pour la mise en œuvre. Les défis rencontrés dans le processus comprenaient une coordination complexe entre les différentes parties prenantes, l’allocation d’un budget suffisant pour sa mise en œuvre, un roulement fréquent au sein du ministère de la Santé publique et la pandémie de COVID-19. Le PNDChM est une première en son genre en Afrique francophone et les nombreuses leçons apprises pourront être utiles aux pays qui aspirent à élaborer leurs propres PNCOA.

Similar content being viewed by others
Notes
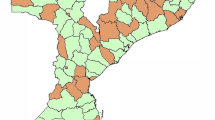
CHRD = centre hospitalier de référence du district; régionale; CHU = centre hospitalier universitaire
CHRD = centre hospitalier de référence du district; régionale; CHU = centre hospitalier universitaire
References
Meara JG, Leather AJ, Hagander L, et al. Global surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet 2015; 386: 569–624. https://doi.org/10.1016/s0140-6736(15)60160-x
World Health Organization. Strengthening emergency and essential surgical care and anaesthesia as a component of universal health coverage, 2015. Available from URL: https://apps.who.int/gb/ebwha/pdf_files/WHA68/A68_R15-en.pdf (accessed November 2022).
Citron I, Sonderman K, Subi L, Meara JG. Making a case for national surgery, obstetric, and anesthesia plans. Can J Anesth 2019; 66: 263–71. https://doi.org/10.1007/s12630-018-01269-5
Fatima I, Shoman H, Peters AW, Samad L, Nishtar S. Pakistan’s National Surgical, Obstetric, and Anesthesia Plan: an adapted model for a devolved federal-provincial health system. Can J Anesth 2020; 67: 1212–6. https://doi.org/10.1007/s12630-020-01708-2
Truché P, Shoman H, Redy CL, et al. Globalization of national surgical, obstetric and anesthesia plans: the critical link between health policy and action in global surgery. Global Health 2020; 16: 1. https://doi.org/10.1186/s12992-019-0531-5
Citron I, Jumbam D, Dahm J, et al. Towards equitable surgical systems: development and outcomes of a national surgical, obstetric and anaesthesia plan in Tanzania. BMJ Glob Health 2019; 4: e001282. https://doi.org/10.1136/bmjgh-2018-001282
Sonderman KA, Citron I, Mukhopadhyay S, et al. Framework for developing a national surgical, obstetric and anaesthesia plan. BJS Open 2019; 3: 722–32. https://doi.org/10.1002/bjs5.50190
United Nations Institute for Training and Research. National surgical obstetric anesthesia planning (NSOAP) manual. Available from URL: https://unitar.org/sustainable-development-goals/people/our-portfolio/programme-health-and-development/global-surgery/national-surgical-obstetric-anesthesia-planning-nsoap-manual (accessed November 2022).
UNICEF Data. Madagascar: key demographic indicators. Available from URL: https://data.worldbank.org/indicator/NY.GDP.PCAP.CD?locations=MG (accessed November 2022).
The World Bank. GDP per capita (current US$) – Madagascar. Available from URL: https://data.worldbank.org/indicator/NY.GDP.PCAP.CD?locations=MG (accessed November 2022).
Barmania S. Madagascar’s health challenges. Lancet 2015; 386: 729–30. https://doi.org/10.1016/s0140-6736(15)61526-4
World Health Organization. Plague – Madagascar. Available from URL: https://www.who.int/emergencies/disease-outbreak-news/item/plague---madagascar (accessed November 2022).
The World Bank. Maternal mortality ratio (modeled estimate, per 100,000 live births) – Madagascar. Available from URL: https://data.worldbank.org/indicator/SH.STA.MMRT?locations=MG (accessed November 2022).
Marks F, Rabehanta N, Baker S, et al. A way forward for healthcare in Madagascar? Clin Infect Dis 2016l 62: S76–9. https://doi.org/10.1093/cid/civ758
Bruno E, White MC, Baxter LS, et al. An evaluation of preparedness, delivery and impact of surgical and anesthesia care in Madagascar: a framework for a national surgical plan. World J Surg 2017; 41: 1218–24. https://doi.org/10.1007/s00268-016-3847-9
World Federation of Societies of Anaesthesiologists. World anaesthesiology workforce map. Available from URL: https://wfsahq.org/resources/workforce-map/ (accessed November 2022).
Baxter LS, Ravelojaona VA, Rakotoarison HN, et al. An observational assessment of anesthesia capacity in Madagascar as a prerequisite to the development of a national surgical plan. Anesth Analg 2017; 124: 2001–7. https://doi.org/10.1213/ane.0000000000002049
Yaya S, Uthman OA, Amouzou A, Bishwajit G. Disparities in caesarean section prevalence and determinants across sub-Saharan Africa countries. Glob Health Res Policu 2018; 3: 19. https://doi.org/10.1186/s41256-018-0074-y
Honda A, Randaoharison PG, Matsui M. Affordability of emergency obstetric and neonatal care at public hospitals in Madagascar. Reprod Health Matters 2011; 19: 10–20. https://doi.org/10.1016/s0968-8080(11)37559-3
Shrime MG, Hamer M, Mukhopadhyay S, et al. Effect of removing the barrier of transportation costs on surgical utilisation in Guinea, Madagascar and the Republic of Congo. BMJ Glob Health 2017; 2: e000434. https://doi.org/10.1136/bmjgh-2017-000434
Kingdon JW. Agendas, Alternatives, and Public Policies. Boston: Little, Brown & Co.: 1984.
Milton K, Grix J. Public health policy and walking in England—analysis of the 2008 ‘policy window’. BMC Public Health 2015; 15: 614. https://doi.org/10.1186/s12889-015-1915-y
Albutt K, Sonderman K, Citron I, et al. Healthcare leaders develop strategies for expanding national surgical, obstetric, and anaesthesia plans in WHO AFRO and EMRO regions. World J Surg 2019; 43: 360–7. https://doi.org/10.1007/s00268-018-4819-z
World Health Organization. Surgical care systems strengthening: developing national surgical, obstetric and anaesthesia plans, 2017. Available from URL: https://apps.who.int/iris/handle/10665/255566 (accessed November 2022).
Jumbam DT, Reddy CL, Roa L, Meara JG. How much does it cost to scale up surgical systems in low-income and middle-income countries? BMJ Glob Health 2019; 4: e001779. https://doi.org/10.1136/bmjgh-2019-001779
OAU/SPS/ABUJA. Abuja declaration on HIV/AIDS, tuberculosis and other related infectious diseases. Available from URL: https://au.int/sites/default/files/pages/32894-file-2001-abuja-declaration.pdf (accessed November 2022).
Reddy CL, Peters AW, Jumbam DT, et al. Innovative financing to fund surgical systems and expand surgical care in low-income and middle-income countries. BMJ Glob Health 2020; 5: e002375. https://doi.org/10.1136/bmjgh-2020-002375
World Health Organization. Pratique chirurgicale de base dans les structures à moyens limités, 2011. Available from URL: https://apps.who.int/iris/handle/10665/44608 (accessed November 2022).
Kanamori S, Shibanuma A, Jimba M. Applicability of the 5S management method for quality improvement in health-care facilities: a review. Trop Med Health 2016; 44: 21. https://doi.org/10.1186/s41182-016-0022-9
Micah AE, Chen CS, Zlavog BS, Hashimi G, Chapin A, Dieleman JL. Trends and drivers of government health spending in sub-Saharan Africa, 1995–2015. BMJ Glob Health 2019; 4: e001159. https://doi.org/10.1136/bmjgh-2018-001159
Johns Hopkins Coronavirus Resource Center. COVID-19 dashboard. https://coronavirus.jhu.edu/map.html (accessed November 2022).
Mazingi D, Navarro S, Bobel MC, Dube A, Mbanje C, Lavy C. Exploring the impact of COVID-19 on progress towards achieving global surgery goals. World J Surg 2020; 44: 2451–7. https://doi.org/10.1007/s00268-020-05627-7
Villavisanis DF, Kiani SN, Taub PJ, Marin ML. Impact of COVID-19 on global surgery: challenges and opportunities. Ann Surg 2021; 2: e046. https://doi.org/10.1097/AS9.0000000000000046
Park K. To prepare for pandemics, invest in surgical care, 2020. Available from URL: https://globalhealthnow.org/2020-09/prepare-pandemics-invest-surgical-care (accessed November 2022).
Author contributions
Vaonandianina Ravelojaona, Xiya Ma, Desmond T. Jumbam, and Lalatiana M. Andriamanarivo contributed to all aspects of this manuscript, including study conception and design; acquisition, analysis, and interpretation of data; and drafting the article. Marie-Fidèle Samison, Dominique Rabemalala, Ruben Ayala, Anjaramamy Ramamonjisoa, Hery H. Andriamanjato, and Voahangiseheno Ravoniaritsoa contributed to data acquisition, data interpretation, and critical feedback of the manuscript including subsequent revisions.
Disclosures
None.
Funding statement
None.
Editorial responsibility
This submission was handled by Dr. Adrian Gelb, Guest Editor (Global Health and Sustainability), Canadian Journal of Anesthesia/Journal canadien d’anesthésie.
Contributions des auteurs
Vaonandianina Ravelojaona, Xiya Ma, Desmond T. Jumbam et Lalatiana M. Andriamanarivo ont contribué à tous les aspects de ce manuscrit, y compris la création et la conception de l’étude, l’acquisition, l’analyse et l’interprétation des données, et la rédaction de l’article. Marie-Fidèle Samison, Dominique Rabemalala, Ruben Ayala, Anjaramamy Ramamonjisoa, Hery H. Andriamanjato et Voahangiseheno Ravoniaritsoa ont contribué à l’acquisition et à l’interprétation des données et à la rétroaction critique du manuscrit, y compris des révisions ultérieures.
Déclaration
Aucune.
Déclaration de financement
Aucune.
Responsabilité éditoriale
Cet article a été traité par Dr Adrian Gelb, rédacteur invité (Santé mondiale et durabilité), Journal canadien d’anesthésie.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is accompanied by an Editorial. Please see Can J Anesth 2023; https://doi.org/10.1007/s12630-023-02497-0.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ravelojaona, V., Ma, X., Samison, MF. et al. Incorporating surgical and anesthesia care into universal health care: a national plan for the development of surgery in Madagascar. Can J Anesth/J Can Anesth 70, 1131–1154 (2023). https://doi.org/10.1007/s12630-023-02500-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-023-02500-8