Abstract
Purpose
Individual factors of low rates of return to sport after anterior cruciate ligament (ACL) reconstruction were unclear. We evaluated the impact of various individual factors after ACL reconstruction for return to sport in athletes.
Methods
A prospective study was performed in 1274 athletes, who had undergone ACL autograft reconstruction. Individual factors survey about return to sport was performed during the second year after surgery. Athlete responses were analyzed with a multivariate logistic model adjusted for baseline patient characteristics and an adjusted Cox model.
Results
Younger age and involvement in higher-level sporting activities were associated with a significantly higher frequency and a significantly shorter time to return to sport (running, training, competition; p = 0.001 to 0.028). Men returned to sport more rapidly than women, for both training (p = 0.007) and competition (p = 0.042). Although there was no difference to return to sport between hamstring (HT) and patellar tendon (PT) autograft. We note that MacFL surgery (Mac Intosh modified with intra- and extra-articular autografts used the tensor fasciae latae muscle) was associated with a higher frequency (p = 0.03) and rapidity (p = 0.025) of return to training than HT. Sports people practicing no weight-bearing sports returned to training (p < 0.001) and competition (p < 0.001) more rapidly than other sports people. By contrast, the practicing pivoting sports with contact started running again sooner (p < 0.001).
Conclusion
Younger age, male sex, higher level of sports, sportspeople practicing no weight-bearing sports, and MacFL surgery reduce time to return to sport after ACL reconstruction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the USA, the reported annual incidence of ACL reconstruction is 36.9 per 100,000 people [1]. Currently, two main reconstruction techniques are used: patellar tendon and hamstring autografts. Nowadays, using hamstring autografts was the gold standard for ACL reconstruction [2, 3]. As reported in Denmark, the proportion of hamstring autografts increased from 68% in 2005 to 85% in 2011 [4]. However, very few differences [5,6,7] have been clearly demonstrated between these two reconstruction procedures [8, 9]. Patellar tendon autografts are more frequently associated with anterior knee pain [8, 10], whereas hamstring autografts tend to progress toward greater residual laxity [8, 11]. Alternative graft options exist, but very few comparative studies have been performed on it. These alternatives include, in particular, hamstring autografts using only the semitendinosus (ST) with two tunnels (a femoral and a tibial tunnel) [12,13,14], hamstring autografts with an anterolateral graft tensor (HT + AL) with two tunnels (a femoral and a tibial tunnel) [15, 16], muscle hamstring autografts with double bundle and four anatomic tunnels (2HT) [17], and intra- and extra-articular autografts with the tensor fasciae latae muscle (MacFL) [18, 19]. Furthermore, increasing numbers of studies are focusing on the return to sport [20,21,22], but these studies do not sufficiently take into account morphotype data that may also have an impact on the return to sport [23,24,25,26,27,28]. No study specifies the frequencies and times to each chronological stage of the return to sport, in the same series, for a population of sportspeople practicing at different levels with multivariate analyses and adjustment for baseline patient characteristics. We therefore tested the hypothesis that baseline factors (age, sex, type and level of sport, and type of surgery) could influence return to sport.
With this prospective study, we proposed to investigate the influence of these factors on the frequency and time to return to sport after initial ligament reconstruction in a population of athletes.
Material and methods
This was a prospective study that included athletes who had undergone a first ACL autograft reconstruction between 01/06/2017 and 31/12/2018. The study was approved by a scientific ethics committee (Groupement de Cooperation Sanitaire Ramsay Générale de Santé pour l’Enseignement et la Recherche, Paris, IRB N. COS-RGDS-2015–09-018), and all patients signed an informed consent form for participation.
Patients with osteotomy, bone fracture or chondroplasty, an associated medial/lateral ligament surgery, and iso or contralateral rupture were not included. When athletes were included, all their data were input into a computerized database that included complete surgical, medical, and sports-related data. All surgical information were completely determined. Patients were considered eligible for this study if they had undergone one of six different types of surgery [29] for a first reconstruction and aged more than 16 years. All the surgeries were performed by French LCA specialist surgeons. The use of arthroscopy was referred to in all the surgeries. The first surgery used the patellar tendon autografts (PT), involving transplantation of the patellar tendon (bone-patellar tendon-bone) with a single bundle, and two tunnels (a femoral and a tibial tunnel) [8]. The type of femoral and tibial fixations were interference screws. The second surgery was hamstring autografts (HT) requiring two hamstring muscles (semitendinosus and gracilis), folded over, with a single bundle and two tunnels (a femoral and a tibial tunnel) [8]. The single bundle was composed of four strands. The type of femoral and tibial fixations were endobuttons or screws. The third surgery was hamstring autografts using only the semitendinosus (ST) with a single bundle and two tunnels (a femoral and a tibial tunnel) [12,13,14]. The single bundle was composed of three strands. The type of femoral and tibial fixations were endobuttons or screws. The fourth was hamstring autografts with an anterolateral graft (HT + AL) with two tunnels (a femoral and a tibial tunnel) [15, 16]. It is a graft combined with anterolateral ligament reconstruction. The type of femoral and tibial fixations were endobuttons or screws. The fifth was hamstring muscle autografts with a double bundle and four anatomic tunnels (2HT) [17]. The anterior cruciate ligament consists of at least two distinct functional bundles: the anteromedial bundle and the posterolateral bundle. An anatomic double-bundle ACL reconstruction was therefore close to the native anatomy to increase the rotational stability. The sixth was the Mac Intosh modified with intra- and extra-articular autografts used the tensor fasciae latae muscle (MacFL) [18, 19]. The graft was realized with a combined internal and external anterior cruciate ligament reconstruction with the iliotibial band autograft.
Rehabilitation [25] was based on post-operative recovery for articular extension at 0° and articular flexion at more than 120°, quadriceps contraction against gravity, and techniques for walking without assistance from three to six weeks after surgery. A brace was worn for three to six weeks, as decided by the surgeon. Cardiovascular activity on a bicycle, step machine, or rowing machine was introduced progressively, and swimming (crawl) was also introduced during this period. A return to running was introduced around the third or fourth month, at the decision of the surgeon. Return to the original activity was subject to the surgeon’s approval.
Patients were contacted by telephone during the second year after surgery. Data regarding return to sport (running, training, competitive sport, same level of competition) and the time to each of these events were collected. Sports were analyzed according to discipline and were grouped according to the Arpège classification [30]. For patients playing competitively, sport level was classified as regional, national, or international, whereas patients playing non-competitively were classified as recreational athletes, such as as sports teacher, coach, or monitor.
Statistical analyses
Multivariate logistic regression analyses were performed to evaluate the effects of the various factors on the frequency of return to sport outcome (primary endpoint), with adjustment for baseline patient characteristics. A Cox multivariate model accounting for the same factors was performed on the time to return to sport, to establish the robustness of the results in terms of the primary endpoint. The alpha risk was fixed at 5%. Statistical analyses were performed with SAS® for Windows (Version 9.4, SAS Institute Inc., Cary, NC, USA).
Results
In total, we screened 2450 athletes undergoing ACL autograft reconstruction. Of the initial population, 897 did not meet the inclusion criteria (Fig. 1). Responses (82%) from 1274 athletes were thus analyzed. The mean time between initial surgery and questionnaire completion was 19.5 months (± 4.2).
Population were analyzed for the six types of surgery (Table 1): 56% (N = 712) for the hamstring group (HT), 19% (N = 243) for the patellar tendon autograft group (PT), 10.7% (N = 137) for hamstring autografts using only the semitendinosus (ST), 4.1% (N = 52) for hamstring autografts with an anterolateral graft tensor fasciae latae (HT + AL), 6% (N = 76) for hamstring muscle autografts with a double bundle and four anatomic tunnels (2HT), and 4.2% (N = 54) for autografts with the tensor fasciae latae muscle (MacFL). Mean age was 26.2 years. The most common sport practiced was rugby (33.7%), followed by soccer, handball, and skiing.
Influence of baseline factors on the return to sport outcome
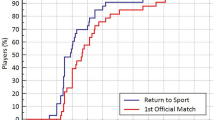
A return to running was reported for 94.2% of patients, a return to training for 84.8%, a return to competition for 74.3%, and a return to the same level of competition for 63.4%. The mean times for the return to sport were 4.8 months for the return to running, 7.9 months for the return to training, 9.5 months for the return to competition, and 10.5 months for the return to the same level of competition (Table 2).
Various factors (age, sex, type of sport and type of surgery) affected return to sport, but in different ways, depending on the chronology of the steps in the return to sport.
Age
A younger age (< 25 years versus > 25 years) was associated with a significantly higher frequency of return to sport (Table 3): for running (p = 0.006), training (p = 0.026), competition (p = 0.008), and return to the same level of competition (p = 0.005). Being younger was also associated with a shorter time to return to sport (Table 4): for running (p = 0.002), training (p = 0.076), competition (p = 0.028), and return to the same level of competition (p = 0.015).
Sex
Women returned to sport significantly less rapidly than men, for training (p = 0.007) and competition (p = 0.042) (Table 4).
Sport level
Higher sport levels (Table 3) were associated with a significantly higher frequency of return to sport: for running (p = 0.01), training (p = 0.007), competition (p < 0.001), and return to the same level of sport (p = 0.001). Being higher sport level was associated with more rapidly return to sport (Table 4): for running (p = 0.018), training (p < 0.001), competition (p < 0.001), and return to the same level of competition (p < 0.001).
Type of sport
Sportspeople practicing sports involving pivoting with contact, who are used to running, starting running again sooner than those practicing other types of sport (Tables 4; p < 0.001). Sportspeople practicing no weight-bearing sports, which make less demands on the knee, returned to sport more rapidly (Table 4) for training (p < 0.001) and competition (p < 0.001).
Type of surgery
MacFL surgery (Table 3) was associated with a higher frequency of (p = 0.03) and a faster (p = 0.025) return to training than HT (Table 4).
Discussion
The most important finding of the study was that baseline factors (age, sex, level, sport, and surgery) can influence return to sport. And we have precise the frequency and the time of the steps in the return to sport which was unknown before.
We found that the frequency of return to sport was 94.2% for running, 84.8% for training, 74.3% for competition, and 63.4% for return to the same level of competition. Our results were important to have a better comprehension of return-to-sport decision. Ardern [20] precise that return to sport is a continuum with different steps: return to participation, return to sport, and return to performance. But, in general, most studies give only a part of results like competition but not the different steps of the continuum. Dingenen [31] proposed an optimized criterion-based multifactorial return-to-sport approach based on shared decision making with a layered approach within a smooth continuum with repeated athletic evaluations throughout rehabilitation followed by a gradual periodized reintegration into sport with adequate follow-up could help to guide an individual athlete toward a successful return to sport [32, 33]. Our results were a little better than the other publications [21, 34]. Ardern reported [21] a low frequency of 55% for return to the same level of competition, and Czuppon [34] found a frequency of return to sport of 50.7% in a meta-analysis. Our study is of interest because it specifies the frequencies and times to each chronological stage of the return to sport, in the same series, for a population of sportspeople practicing at different levels. The mean times recorded were 4.8 months for the return to running, 7.9 months for the return to training, 9.5 months for the return to competition, and 10.5 months for the return to competition at the same level. These times are consistent with published results for a return to the same level of competition but more detailed: 10.7 months for basketball players in the NBA [35], 10.2 months for the soccer players of the MLS [36], and 9.8 months for ice hockey players [37].
We showed here that age influences the frequency and time to return to sport, for all the chronological stages considered (running, training or competition). No study found these results in different steps of return to play. Just Arden also reported a small effect of being younger, favoring a return to preinjury level sport (effect size, 0.3) [21]. Those over the age of 25 years are 50% less likely to return to playing at their preinjury level of sport than their younger counterparts (OR, 0.5; 95% CI, 0.3–0.8) [22], and two-thirds of athletes over the age of 32 years do not return to their preinjury level [20]. NHL players injured after the age of 30 years were found to be less likely to return to play at least one full season [37], and younger French alpine skiers at the time of injury were found to be more likely to improve their performance after returning to sport [38].
In this study, we found that sex influenced the time to return to training and competition, with men returning more rapidly than women. We confirmed results of literature like Arden who found that men were about 1.5 times more likely than women to return to the preinjury level of sport (OR, 1.4; 95% CI, 1.2–1.7) and to competitive sport (OR, 1.7; 95% CI, 1.2–2.3) [21], but we proved that it was the case for training too.
We have shown that sport level influences the possibilities for returning and the time to return to sport (running, training, competition, same level), with better results for higher levels. This completed published results, as Ardern showed that elite athletes were 2.5 times more likely to return to their preinjury level (OR, 2.5; 95% CI, 2.0–3.1) and six times more likely to return to competitive sport (OR, 5.9; 95% CI, 4.6–7.5) than nonelite athletes [21]. In our study, the frequency of return to competition was 89.5% at the international level, and the frequency of return to the same level of competition was 80.5%, a value similar to that reported by Lai [27], who found, in a meta-analysis, that 83% of elite sportspeople returned to the same level of competition. And in our study, athletes returned to the same level for 70.8% for the national level, 59.4% for the regional level, and 51.8% for others.
Our results show that the type of sport influences the frequency of return to running, but also the time to the return to running, training, and competition. Participants in no weight-bearing sports returned to running less rapidly than those involved in pivoting sports. By contrast, they returned to training and competition more rapidly. Those involved in contact sports returned to training less rapidly than those participating in pivoting sports without contact. We were unable to identify any similar published studies with which to compare our results.
We found no significant difference in the rates of return to competition between HT (70.9%) and PT surgery (77.9%) (adjusted OR = 0.718; 95% CI (0.50;1.02)), consistent with most published findings [24, 39]. By contrast, the frequency and time to return to training were significantly higher for MacFL (92.3% and 7.3 months, respectively) in our study after adjustment for the various factors in the multivariate analysis, but we were unable to identify any similar published studies. It would be interesting to confirm these results in larger population and would be important information for high-level sports people.
Limitations of the study
We found several biases of inclusion as in all prospective studies. The different surgeons operating on the patients are a potential source of bias worthy of inclusion in analyses. Nonetheless, any associated bias was limited, given that the inclusion of patients was nationwide and there was a large number of participating surgeons, all of whom are specialists in knee reconstruction. Randomization was not performed at inclusion, but the large population, similar baseline characteristics, and adjusted analyses would have reduced potential bias. As the adjusted comparisons take into account confounding factors, they are thus interpretable with good quality.
For this study, a telephone questionnaire was performed a mean of 19.5 months after the autografting procedure. This is a short post-operative time, but our methodology was otherwise very similar to others [40,41,42], and the aim of this study was to analyze the initial chronological stage of the return to sport. Furthermore, our population included a large series of athletes, most practicing competitively, whereas most of the other reports have tended to focus on sports as leisure activities. The impact of the different sports practiced, along with their relationship to the level of sport practiced, was evaluated.
Conclusion
The factors considered (age, sex, type and level of sport, and type of surgery) influence the outcome of anterior cruciate ligament reconstruction. For the return to sport, younger athletes were more likely to return to sport but did so more rapidly. Higher sport levels were associated with a higher frequency of return to sport and a faster return. Men also returned to sport more rapidly than women. Although there is no difference in the principal surgery (HT and PT), it is interessant to observe that MacFL led to a higher frequency of and a faster return to training than HT. Sportspeople practicing non-weight-bearing sports returned to training and competition more rapidly than those practicing weight-bearing sports. However, those practicing pivoting contact sports returned more rapidly to running. Finally, a young man practicing weight-bearing sports with MacFL autograft surgery is the patient with the most important frequency and faster return to sport.
References
Gianotti SM, Marshall SW, Hume PA, Bunt L (2009) Incidence of anterior cruciate ligament injury and other knee ligament injuries: a national population-based study. J Sci Med Sport 12(6):622–627. https://doi.org/10.1016/j.jsams.2008.07.005
Chambat P, Guier C, Sonnery-Cottet B, Fayard JM, Thaunat M (2013) The evolution of ACL reconstruction over the last fifty years. Int Orthop 37(2):181–186. https://doi.org/10.1007/s00264-012-1759-3
Chechik O, Amar E, Khashan M, Lador R, Eyal G, Gold A (2013) An international survey on anterior cruciate ligament reconstruction practices. Int Orthop 37(2):201–206. https://doi.org/10.1007/s00264-012-1611-9
Rahr-Wagner L, Thillemann TM, Pedersen AB, Lind M (2014) Comparison of hamstring tendon and patellar tendon grafts in anterior cruciate ligament reconstruction in a nationwide population-based cohort study: results from the Danish registry of knee ligament reconstruction. Am J Sports Med 42(2):278–284. https://doi.org/10.1177/0363546513509220
Gabler CM, Jacobs CA, Howard JS, Mattacola CG, Johnson DL (2016) Comparison of graft failure rate between autografts placed via an anatomic anterior cruciate ligament reconstruction technique: a systematic review, meta-analysis, and meta-regression. Am J Sports Med 44(4):1069–1079. https://doi.org/10.1177/0363546515584043
Gifstad T, Foss OA, Engebretsen L, Lind M, Forssblad M, Albrektsen G, Drogset JO (2014) Lower risk of revision with patellar tendon autografts compared with hamstring autografts: a registry study based on 45,998 primary ACL reconstructions in Scandinavia. Am J Sports Med 42(10):2319–2328. https://doi.org/10.1177/0363546514548164
Xie X, Liu X, Chen Z, Yu Y, Peng S, Li Q (2015) A meta-analysis of bone-patellar tendon-bone autograft versus four-strand hamstring tendon autograft for anterior cruciate ligament reconstruction. Knee 22(2):100–110. https://doi.org/10.1016/j.knee.2014.11.014
Biau DJ, Tournoux C, Katsahian S, Schranz PJ, Nizard RS (2006) Bone-patellar tendon-bone autografts versus hamstring autografts for reconstruction of anterior cruciate ligament: meta-analysis. BMJ (Clinical research ed) 332(7548):995–1001. https://doi.org/10.1136/bmj.38784.384109.2F
Salmon L, Russell V, Musgrove T, Pinczewski L, Refshauge K (2005) Incidence and risk factors for graft rupture and contralateral rupture after anterior cruciate ligament reconstruction. Arthrosc J Arthrosc Relat Surg 21(8):948–957. https://doi.org/10.1016/j.arthro.2005.04.110
Runer A, Keeling L, Wagala N, Nugraha H, Özbek EA, Hughes JD, Musahl V (2023) Current trends in graft choice for primary anterior cruciate ligament reconstruction - part II: in-vivo kinematics, patient reported outcomes, re-rupture rates, strength recovery, return to sports and complications. J Exp Orthop 10(1):40. https://doi.org/10.1186/s40634-023-00601-3
Wagner M, Kääb MJ, Schallock J, Haas NP, Weiler A (2005) Hamstring tendon versus patellar tendon anterior cruciate ligament reconstruction using biodegradable interference fit fixation: a prospective matched-group analysis. Am J Sports Med 33(9):1327–1336. https://doi.org/10.1177/0363546504273488
Islam MZ, Rahman M, Ali ME, Alam MK, Ahmed W, Alam MT, Saha MK (2017) Arthroscopic anterior cruciate ligament reconstruction with triplet autograft of semitendinosus tendon. Mymensingh Med J : MMJ 26(3):545–550
Madaíl CA, Vaz MF, Amaral PM, Consciência JG, Silva AL (2018) Quadruple semitendinosus graft construct with double cortical suspensory fixation for anterior cruciate ligament reconstruction: a biomechanical study. Sci Rep 8(1):12835. https://doi.org/10.1038/s41598-018-30931-7
Orfeuvre B, Pailhé R, Sigwalt L, Rubens Duval B, Lateur G, Plaweski S, Saragaglia D (2018) Anterior cruciate ligament reconstruction with the Tape Locking Screw (TLS) and a short hamstring graft: clinical evaluation of 61 cases with a minimum 12 months’ follow-up. Orthop Traumatol Surg Res : OTSR 104(5):701–705. https://doi.org/10.1016/j.otsr.2018.03.016
Saragaglia D, Pison A, Refaie R (2013) Lateral tenodesis combined with anterior cruciate ligament reconstruction using a unique semitendinosus and gracilis transplant. Int Orthop 37(8):1575–1581. https://doi.org/10.1007/s00264-013-1957-7
Sonnery-Cottet B, Saithna A, Cavalier M, Kajetanek C, Temponi EF, Daggett M, Helito CP, Thaunat M (2017) Anterolateral ligament reconstruction is associated with significantly reduced ACL graft rupture rates at a minimum follow-up of 2 years: a prospective comparative study of 502 patients from the SANTI Study Group. Am J Sports Med 45(7):1547–1557. https://doi.org/10.1177/0363546516686057
Svantesson E, Sundemo D, Hamrin Senorski E, Alentorn-Geli E, Musahl V, Fu FH, Desai N, Stålman A, Samuelsson K (2017) Double-bundle anterior cruciate ligament reconstruction is superior to single-bundle reconstruction in terms of revision frequency: a study of 22,460 patients from the Swedish National Knee Ligament Register. Knee Surg Sports Traumatol Arthrosc 25(12):3884–3891. https://doi.org/10.1007/s00167-016-4387-4
Jørgensen U, Bak K, Ekstrand J, Scavenius M (2001) Reconstruction of the anterior cruciate ligament with the iliotibial band autograft in patients with chronic knee instability. Knee Surg Sports Traumatol Arthrosc 9(3):137–145. https://doi.org/10.1007/s001670000163
Stensbirk F, Thorborg K, Konradsen L, Jørgensen U, Hölmich P (2014) Iliotibial band autograft versus bone-patella-tendon-bone autograft, a possible alternative for ACL reconstruction: a 15-year prospective randomized controlled trial. Knee Surg Sports Traumatol Arthrosc 22(9):2094–2101. https://doi.org/10.1007/s00167-013-2630-9
Ardern CL, Taylor NF, Feller JA, Webster KE (2012) Return-to-sport outcomes at 2 to 7 years after anterior cruciate ligament reconstruction surgery. Am J Sports Med 40(1):41–48. https://doi.org/10.1177/0363546511422999
Ardern CL, Taylor NF, Feller JA, Webster KE (2014) Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med 48(21):1543–1552. https://doi.org/10.1136/bjsports-2013-093398
Ardern CL (2015) Anterior cruciate ligament reconstruction-not exactly a one-way ticket back to the preinjury level: a review of contextual factors affecting return to sport after surgery. Sports health 7(3):224–230. https://doi.org/10.1177/1941738115578131
Bjordal JM, Arnły F, Hannestad B, Strand T (1997) Epidemiology of anterior cruciate ligament injuries in soccer. Am J Sports Med 25(3):341–345. https://doi.org/10.1177/036354659702500312
Laboute E, James-Belin E, Puig PL, Trouve P, Verhaeghe E (2018) Graft failure is more frequent after hamstring than patellar tendon autograft. Knee Surg Sports Traumatol Arthrosc 26(12):3537–3546. https://doi.org/10.1007/s00167-018-4982-7
Laboute E, Savalli L, Lefesvre T, Puig P, Trouve P (2008) Intérêt d’une rééducation spécialisée à distance d’une chirurgie du ligament croisé antérieur chez le sportif de haut niveau [Interest of an iterative specialized rehabilitation after an anterior cruciate ligament reconstruction in high level sport athletes]. Rev Chir Orthop Reparatrice Appar Mot 94(6):533–540. https://doi.org/10.1016/j.rco.2008.01.008
Laboute E, Verhaeghe E, Ucay O, Minden A (2019) Evaluation kinaesthetic proprioceptive deficit after knee anterior cruciate ligament (ACL) reconstruction in athletes. J Exp Orthop 6(1):6. https://doi.org/10.1186/s40634-019-0174-8
Lai CCH, Ardern CL, Feller JA, Webster KE (2018) Eighty-three per cent of elite athletes return to preinjury sport after anterior cruciate ligament reconstruction: a systematic review with meta-analysis of return to sport rates, graft rupture rates and performance outcomes. Br J Sports Med 52(2):128–138. https://doi.org/10.1136/bjsports-2016-096836
Rochcongar P, Laboute E, Jan J, Carling C (2009) Ruptures of the anterior cruciate ligament in soccer. Int J Sports Med 30(5):372–378. https://doi.org/10.1055/s-0028-1105947
Yang XG, Wang F, He X, Feng JT, Hu YC, Zhang H, Yang L, Hua K (2020) Network meta-analysis of knee outcomes following anterior cruciate ligament reconstruction with various types of tendon grafts. Int Orthop 44(2):365–380. https://doi.org/10.1007/s00264-019-04417-8
Christel P, Djian P, Darman Z, Witvoët J (1993) Etude des résultats de l’intervention de Marshall-MacIntosh selon trois systèmes d’évaluation (ARPEGE, Lysholm, IKDC). 90 cas revus avec un recul d’au moins un an [Results of Marshall-MacIntosh reconstruction according to 3 scoring systems (ARPEGE, Lysholm, IKDC). 90 cases reviewed with at least a one-year follow-up]. Rev Chir Orthop Reparatrice l’appar Mot` 79(6):473–483
Dingenen B, Gokeler A (2017) Optimization of the return-to-sport paradigm after anterior cruciate ligament reconstruction: a critical step back to move forward. Sports Med (Auckland, N.Z.) 47(8):1487–1500. https://doi.org/10.1007/s40279-017-0674-6
De Mille P, Osmak J (2017) Performance: bridging the gap after ACL surgery. Curr Rev Musculoskelet Med 10(3):297–306. https://doi.org/10.1007/s12178-017-9419-2
Graziano J, Chiaia T, de Mille P, Nawabi DH, Green DW, Cordasco FA (2017) Return to sport for skeletally immature athletes after ACL reconstruction: preventing a second injury using a quality of movement assessment and quantitative measures to address modifiable risk factors. Orthop J Sports Med 5(4):2325967117700599. https://doi.org/10.1177/2325967117700599
Czuppon S, Racette BA, Klein SE, Harris-Hayes M (2014) Variables associated with return to sport following anterior cruciate ligament reconstruction: a systematic review. Br J Sports Med 48(5):356–364. https://doi.org/10.1136/bjsports-2012-091786
Busfield BT, Kharrazi FD, Starkey C, Lombardo SJ, Seegmiller J (2009) Performance outcomes of anterior cruciate ligament reconstruction in the National Basketball Association. Arthrosc: J Arthrosc Relat Surg 25(8):825–830
Erickson BJ, Harris JD, Cvetanovich GL, Bach BR, Bush-Joseph CA, Abrams GD, Gupta AK, McCormick FM, Cole BJ (2013) Performance and return to sport after anterior cruciate ligament reconstruction in male major league soccer players. Orthop J Sports Med 1(2):2325967113497189. https://doi.org/10.1177/2325967113497189
Sikka R, Kurtenbach C, Steubs JT, Boyd JL, Nelson BJ (2016) Anterior cruciate ligament injuries in professional hockey players. Am J Sports Med 44(2):378–383. https://doi.org/10.1177/0363546515616802
Haida A, Coulmy N, Dor F, Antero-Jacquemin J, Marc A, Ledanois T, Tourny C, Rousseaux-Blanchi MP, Chambat P, Sedeaud A, Toussaint JF (2016) Return to sport among French alpine skiers after an anterior cruciate ligament rupture: results from 1980 to 2013. Am J Sports Med 44(2):324–330. https://doi.org/10.1177/0363546515612764
Howard JS, Lembach ML, Metzler AV, Johnson DL (2016) Rates and determinants of return to play after anterior cruciate ligament reconstruction in National Collegiate Athletic Association Division I Soccer Athletes: a study of the Southeastern conference. Am J Sports Med 44(2):433–439. https://doi.org/10.1177/0363546515614315
Shelbourne KD, Gray T (1997) Anterior cruciate ligament reconstruction with autogenous patellar tendon graft followed by accelerated rehabilitation. A two- to nine-year followup. Am J Sports Med 25(6):786–795. https://doi.org/10.1177/036354659702500610
Shelbourne KD, Gray T, Haro M (2009) Incidence of subsequent injury to either knee within 5 years after anterior cruciate ligament reconstruction with patellar tendon autograft. Am J Sports Med 37(2):246–251. https://doi.org/10.1177/0363546508325665
Wright RW, Dunn WR, Amendola A, Andrish JT, Bergfeld J, Kaeding CC, Marx RG, McCarty EC, Parker RD, Wolcott M, Wolf BR, Spindler KP (2007) Risk of tearing the intact anterior cruciate ligament in the contralateral knee and rupturing the anterior cruciate ligament graft during the first 2 years after anterior cruciate ligament reconstruction: a prospective MOON cohort study. Am J Sports Med 35(7):1131–1134. https://doi.org/10.1177/0363546507301318
Acknowledgements
The authors wish to thank the society that participate to this work: French Society of Sports Traumatology (SFTS).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception. Material preparation, data collection, and analysis were performed by E. Laboute and E. James-Belin. Data collections were performed by E. Verhaeghe, O. Ucay, and E. Laboute. The first draft of the manuscript was written by E. Laboute. A. Caubere commented on previous versions of the manuscript. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by a scientific ethics committee (Groupement de Cooperation Sanitaire Ramsay Générale de Santé pour l’Enseignement et la Recherche, Paris, IRB N. COS-RGDS-2015–09-018). Informed consent was obtained from all individual participants.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Laboute, E., James-Belin, E., Ucay, O. et al. Prospective study of functional outcomes and return to sports after anterior cruciate ligament reconstruction in the knee. International Orthopaedics (SICOT) 48, 455–463 (2024). https://doi.org/10.1007/s00264-023-05973-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-023-05973-w