Abstract
Purpose
The objective of this study was to evaluate kinaesthetic proprioceptive deficit after knee anterior cruciate ligament (ACL) reconstruction in two populations of athletes, those in the post-surgery period and those in re-training during the intensive program-training phase.
Methods
We performed a prospective study in ACL-operated athletes without previous knee injuries, with 32 athletes in each group. Time since surgery in the operated athletes in the post-surgery group was 21 to 35 days, and between three and 9 months in the re-training group. We also analysed a control group of 32 uninjured non-operated subjects with a similar sporting level. Proprioception was evaluated using the threshold to detection of passive motion (TDPM) test with Biodex-type isokinetic equipment comparing operated knees, non-operated knees and control uninjured non-operated group. The control group was tested twice, 1 day apart to control reproducibility, using the intraclass correlation coefficient (ICC). The p-value threshold for statistical significance between different groups in hypothesis testing was <.05.
Results
TDPM reproducibility was excellent (right knee: ICC = 0.80, left knee: ICC =0.72). We found a bilateral kinaesthetic deficit in post-surgery patients compared to the control group (p < 0.001 and p = 0.011), which was significantly higher on the operated side (p = 0.001). Re-training patients had no significant difference between operated and uninjured knees, but had a kinaesthetic deficit on operated limbs (p = 0.036) compared to the control group.
Conclusion
There was a bilateral deficit in post-surgery athletes with a significant difference between injured and healthy knees, which could be explained by a change in the central nervous system. Compared to the control group, a proprioceptive deficit was only seen for re-training patients on the operated side and not in the healthy limb. Kinaesthetic recovery may be faster for the uninjured side as initial deficit is lower.
Level of evidence II.
Similar content being viewed by others
Introduction
The anterior cruciate ligament (ACL) is essential for the structural and functional stability of the knee. ACL tears are frequent in sport traumatology, within an incidence in the US of 100,000 cases annually in 2010 (Micheo et al., 2010). ACL reconstruction leads to histological and physiological modifications which have consequences on proprioceptive, muscular and functional sport performances (Ben Moussa Zouita et al., 2008; Zouita Ben Moussa et al., 2009).
Afferent proprioception information comes from articular, muscular and cutaneous receptors. The ACL may have up to 2.5% of neural elements consisting of ruffini nerve endings, Golgi tendon organs (both slow-adapting receptors which are sensitive to joint positioning) and Pacinian corpuscles (fast-adapting receptors, which are sensitive to changes in speed or direction during a joint movement) (Jennings, 1994; Ozenci et al., 2007; Reider et al., 2003; Riemann et al., 2002; Schultz et al., 1984). Using its various receptors and acting as a static stabiliser for the knee, the ACL also plays a dynamic stabiliser role, which allows joint muscular tension adaptation (Boerboom et al., 2008). Studies have suggested that proprioceptive deficiency may be responsible for instability after an ACL tear occurs, even in the absence of any significant motor deficit (Ben Moussa Zouita et al., 2008).
Several studies have reported proprioceptive modifications after an ACL tear both following knee reconstruction (Anders et al., 2008; Angoules et al., 2011; Ben Moussa Zouita et al., 2008; Bonfim et al., 2003) and without surgery (Bonfim et al., 2008; Borsa et al., 1997; Friden et al., 1997; Friden et al., 1999), however others have reported an absence of such modifications (Harrison et al., 1994; Henriksson et al., 2001; Mattacola et al., 2002; Pap et al., 1999), and a consensus is yet to be reached. It is important to keep in mind that these studies include patients with very different post-surgery follow-up durations, which is likely to have a major influence on the level of proprioceptive deficit and rehabilitation. Angoules (Angoules et al., 2011) showed decreased joint position sense (JPS) and threshold to detection of passive motion (TDPM) performances for injured knees both before surgery and 3 months later, but not at six or 12 months post-surgery. Moreover, in most of the studies the time between surgery and enrolment was very long sometimes 2 years (Ben Moussa Zouita et al., 2008; Henriksson et al., 2001; Mattacola et al., 2002), with only a few studies performing proprioceptive evaluation immediately after surgery (Angoules et al., 2011; Reider et al., 2003).
It is also important to highlight protocol differences between these studies, notably with respect to the reference used for evaluating proprioceptive deficit in the injured knee. Some studies use the contralateral limb for comparison (Angoules et al., 2011; Bonfim et al., 2003; Dauty et al., 2010), whereas others use healthy populations (Anders et al., 2008; Denti et al., 2000; Fremerey et al., 2000), which makes comparisons of the outcomes challenging.
In the current study, we thus implemented a double comparison using both the contralateral knee as well as a healthy population. The aim of the study was to analyse kinaesthetic modifications in a population of athletes after ACL reconstruction, and compared them with a population uninjured athletes having a similar sporting level. After verifying the reliability of the TDPM test in this setting, comparisons were made at two time-points, post-surgery (at the end of the first month) and during re-training (when running is possible and before the end of the period of rehabilitation). TDPM was selected as the measure of proprioception deficit, as it is considered the most sensitive and validated test for detecting the start of a movement (Reider et al., 2003).
Materials and methods
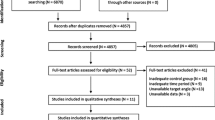
We carried out a prospective study of proprioceptive evaluation using kinaesthetic motion detection after ACL reconstruction in athletes. Reproducibility of the kinaesthetic test was evaluated. And we have measured these kinaesthetic modifications in two operated populations in terms of timing, one during the post-surgery period and the other during the re-training phase. We also compared the results of these injured athletes to a healthy non-operated population. Thus three cohorts of athletes were included, a post-surgical group, a re-training period operated group and a control non-operated group. To be eligible, patients had to have undergone prior ACL reconstruction, be aged between 18 and 40 years old, with a post-surgery delay between 21 and 35 days for the post-surgery operated population or between three and 9 months for the operated population in the re-training phase. The athletes had to have participated in at least regional competitions during the previous 12 months. Patients with previous orthopaedic or traumatic injuries to both knee, simultaneous joint injuries, knee flexion less than 90°, pain, or who were taking any associated medication were excluded.
Proprioception was evaluated using the kinaesthetic test TDPM (Reider et al., 2003) on a Biodex-type isokinetic equipment (Biodex Medical Systems, Shirley, NY). Both knees were evaluated one after another, starting with the uninjured knee to reassure athletes. Athletes were seated with 5 cm between the popliteal fossa and the seat to prevent contact with the underlying surface. Athletes wore shorts to minimize material rubbing against their skin. The thigh was strapped and the leg was connected to the mobile arm of the Biodex using a pneumatic cuff at the level of the ankle. The centre of rotation was placed at the level of the lateral condyle of the knee. For each participant, the anatomic zero point was considered to be the extension position. Athletes were blind-folded and listened to music loud enough to cover any sounds from equipment sound, using headphones, because white noise was impossible with the other patients. The same music was used for all persons. Athletes used a press-button to stop the equipment with a single press of the thumb. Before initiating the TDPM test, a full explanation was given to each patient. Each athlete performed two practice tests (listening to music and blind-folded) to become familiar with the procedure. The starting position of each measurement was a 15° knee flexion (Pitman et al., 1992). After an unspecified period of time, the limb was moved into flexion with a 4°/sec angular velocity. Athletes were asked to use the thumb-button as soon as they detected a knee movement. Pressure on the button instantaneously stopped the movement. The range of motion between the initiation of the movement and the stopping of the machine was recorded in degrees. The examiner then returned the device to the initial position, replacing the leg at 15° flexion, by an extension movement to 0° then a flexion of the knee to 15° which was calculated by a program in the Biodex. At the starting position, the athlete was informed that the next test would begin. The entire TDPM procedure included 10 tests for both limbs. The range of motion between the start position and the perception of movement were averaged for each knee. In first, we checked the reproducibility of this TDPM procedure on an isokinetic Biodex-style machine. In this context, we performed two measures on a healthy control population at a 1 day interval. The study was approved by the Ethics Biomedical Commission of the Academic Hospital of the UCL of Louvain-la-Neuve (Number: B403 2012 14,124). All participants provided written informed consent.
Statistical analysis
Statistical analyses were performed using the Statistical Package for Social Sciences (IBM SPSS Statistics for Windows, Version 19, Chicago, Illinois) and verified by an expert statistician. Reproducibility was determined using the intraclass correlation coefficient (ICC) for both knees in the healthy non-operated population. The ICC scale was defined as insufficient for < 0.4, medium to good for 0.4–0.7, or excellent for > 0.7. Groups were compared using univariate variance analysis (ANOVA, Tukey post-hoc tests) for mean values after we have verified normality and homogeneity. The p-value threshold for statistical significance in hypothesis testing was <.05. For the healthy non-operated population, statistical analyses of knee performances were combined to avoid influencing results by the dominant side (i.e., the mean of the right and left knees). And we have used chi2 and T tests to verify if populations have statistical differences in terms of age, sex, laterality, type of surgery, sporting level, and type of sport.
Results
Population
Thirty-two athletes were included in each of the three cohorts (Table 1). The mean time since surgery was 29.4 days for the post-surgery group, and 164.7 days for the re-training group. Mean age was 24.9 years for both operated groups of athletes, and 26.2 years for the control group. All three groups included more male athletes (post-surgery 78.1%; re-training 68.8% and control 68.8%). There were no statistical differences in terms of age, sex and sporting level between the three groups, with similar proportions of patients participating at the regional and national levels, slightly favouring regional sport. Four surgical techniques were used in each of the two operated groups of patients (Table 2). Hamstring tendon autografts were the most common technique in both groups, used for 78.1% of post-surgery athletes and 75.0% of re-training athletes. The second most common technique in both groups was patellar tendon autografts, reported for 12.5% of post-surgery athletes and 15.6% of re-training athletes. Four-strand semitendinosus graft and fascia lata graft (intra and extra articular) were used with the same proportion in both groups. There were no significant differences between groups in terms of the surgical technique used. In the post-surgery group, 17 left knees and 15 right knees were reconstructed. In the re-training group, 16 left knees and 16 right knees were reconstructed. There were no significant differences between groups for injury laterality.
Reproducibility of the TDPM test
The ICC between the two TDPM tests on two consecutive days in the control non-operated group was 0.80 for the right knee and 0.72 for the left knee, reflecting very high reproducibility for both knees.
Kinaesthetic evaluation in terms of timing
Kinaesthetic evaluation was performed by comparing the following five sub-groups: operated knees of post-surgery athletes, healthy knees of post-surgery athletes, operated knees of re-training athletes, healthy knees of re-training athletes, and left and right healthy knees of non-operated athletes (Table 3).
Post-surgery patients
A significant difference was seen between knees of the control non-operated group versus the operated knees in the post-surgery group (mean .66° vs 1.22°; p < .001; mean difference .56°) as well as versus healthy knees in the post-surgery group (.95°; p = .011; mean difference .29°) which might reflect lower bilateral kinaesthetics immediately after surgery. We also identified a significant difference between operated knees (1.22°) and healthy knees (0.95°) in the post-surgery group (p = .001; mean difference .27°) which suggests lower kinaesthetic perception for operated knees compared to healthy knees.
Re-training period patients
In the re-training group, a significant difference (p = .036; mean difference .25°) was seen for athletes between operated knees (.91°) and knees in the control non-operated population (.66°). However there was no difference between healthy knees (.86°) and either the operated knees of the retraining group or the healthy knees of the control non-operated group (p = .16), reflecting that a kinaesthetic deficit is only present for re-training operated knees.
Evolution over time in operated versus healthy knees
Interestingly, a significant difference was found between operated knees in the post-surgery (1.22°) and re-training (.91°) groups (p < .001; mean difference .31°), which may reflect that the improvement of the kinaesthetic sense of the operated knee depends on the post-surgical delay. For operated knees in the re-training group, there was a significant difference (p = .036; mean difference .25°) with the control non-operated group (.66°), supporting incomplete recovery of the kinaesthetic perception in healthy knees even during re-training phase. The healthy knee of the post-surgery group (.95°) was significantly different (p = .011; mean difference .29°) from the control group (.66°), but not the healthy knee of the re-training subgroup (.86°). A lower initial deficit after surgery for the healthy knee compared to the operated knee could lead to a slightly faster recovery of the kinaesthetic perception of the healthy knee compared to the injured knee.
Discussion
We have demonstrated a bilateral kinaesthetic deficit during the post-surgical phase of ACL reconstruction surgery. This bilateralism confirms previous reports in multiple studies, including in patients with a deficient ACL (Bonfim et al., 2008; Gauffin et al., 1990; Lysholm et al., 1998; Pap et al., 1999) and in some cases after ACL reconstruction (Denti et al., 2000; Fremerey et al., 2000). The hypothesis proposed in the literature to explain this bilateralism is a change in the central nervous system (CNS), with the loss of ACL mechano-receptors that occurs during the tear altering the proprioceptive information in the CNS. Supporting this theory are reports of central reorganization after sensory deprivation or a peripheral lesion (Kapreli & Athanasopoulos, 2006). Several studies have reported central somatosensory changes after ACL tears (Courtney & Rine, 2006; Valeriani et al., 1996; Valeriani et al., 1999), and the cerebral cortex is known to participate in voluntary motor control. Pitmann et al. (Pitman et al., 1992) have reported somatosensory evoked potentials after direct stimulation of the ACL during surgery. Valériani et al. (Valeriani et al., 1996; Valeriani et al., 1999) have measured somatosensory evoked potentials before and after reconstruction in seven patients and found decreased knee kinaesthetic position perception and a lack of the cortical P27 potential on the side of the ACL lesion. Baumeister et al. (Baumeister et al., 2008) have also shown that electroencephalography changed cortical activity after ACL reconstruction. Modifications mostly concern the anterior frontal cortex (theta) and parietal cortical (alpha-2) areas. These modifications are also found during stimulation of healthy limbs in operated patients, explaining the change of proprioceptive capacities. This central reorganization could explain bilateral proprioceptive modifications.
Nevertheless, despite a bilateral deficit after surgery, no significant difference between operated and healthy knees was present during the re-training period. Various studies have found no differences between operated and healthy knees 3, 6 and 12 months after surgery (Angoules et al., 2011; Muaidi et al., 2009a; Muaidi et al., 2009b), but have not compared athletes’ performance to a control group. The current study highlighted a kinaesthetic deficit for operated knees during re-training (p = .036) compared to non-operated controls. Healthy knees in re-training and non-operated patients gave similar performances (p = .160). These results show a likely partial recovery of proprioceptive capacities in injured limbs and almost complete recovery in healthy limbs during re-training. Recovery in injured limbs can be expected to be slower than in healthy (non-injured) limbs. The same principal may apply with a greater kinaesthetic deficit in operated knees than in healthy ones immediately after surgery (p = .001). There may be an evolution of proprioceptive capacities during recovery, as both operated and healthy knees in re-training athletes were significantly more efficient in proprioception than operated knees immediately after surgery. It would have been interesting to follow the same population after surgery and re-training to confirm this faster recovery for the healthy knee. Based on these results, it is difficult to compare healthy limbs to injured ones for evaluation during re-training, and it is important to perform proprioceptive rehabilitation for both injured and healthy knees after surgery, at least until the re-training phase.
The TDPM test has often been used with an electrogoniometer (Reider et al., 2003) in the literature. We have confirmed its reliability with the isokinetic Biodex® machine which measures the same movement, with the control group performing two evaluations with a one-day interval. This short interval took into account that athletes would not improve their proprioceptive capacities between the tests. High reliability was seen with an ICC between the two tests of .80 for the right knee and .72 for the left knee. In our study, kinaesthetic capacities were assessed by TDPM, which was selected from the proprioceptive reference tests available in the literature in light of its superior sensitivity and reliability (Ageberg, 2002; Ageberg et al., 2007; Reider et al., 2003). As joint receptors are mostly stimulated at the end of the range of motion, the knee is more sensitive to movement close to complete extension, and proprioceptive deficit after ACL tears are better detected. To account for this, the test began with a 15° flexion of the knee (Ageberg et al., 2007; Angoules et al., 2011; Friden et al., 2001; Friden et al., 1996; Friden et al., 1997; Ozenci et al., 2007; Riemann & Lephart, 2002; Riemann et al., 2002). A slow angular speed was chosen to increase stimulation of joint receptors and decrease the neuromuscular spindle as suggested by some studies (Ageberg et al., 2007; Friden et al., 1997; Ozenci et al., 2007; Riemann & Lephart, 2002), even when using slower angular speeds of between .5 and 2.5°/sec. We decided to slightly increase angular speed (to 4°/sec), to increase the extent of the arc in degrees and emphasize the differences between groups. Concerning detection of a passive motion, we limited input from other information sources with patients being blindfolded, listening to music to ensure any equipment sound was covered, with shorts to minimize skin rubbing sensations with the ankle strapped to the arm of the Biodex.
The use of this test in a research protocol is relevant, but not in clinical valuation because of the small clinical difference (for example .56° between knees of the control non-operated group versus the operated knees in the post-surgery group) despite significant difference (p < .001). As a result, this evaluation is not commonly used in rehabilitation protocols. For the future, it could be more important to have a global approach with functional valuation (analyse of running or jumping for example) which is closer to the real-life setting, especially for athletes, despite this approach don’t make difference between proprioceptive and muscular parameters.
Conclusion
We identified a bilateral proprioceptive deficit after ACL surgery in injured athletes, with a significant difference between operated and healthy knees. A deficit on injured limbs during re-training was only seen compared to the control group but not to healthy limbs. We presume that kinaesthetic recovery is faster for healthy knees than for injured ones. These results also show the difficulty of comparing healthy and injured knees as no differences were identified during re-training. The results must be compared to a control population to be interpretable during rehabilitation. In the future, more ecological procedures will probably be used to assess deficit during re-training such as functional evaluation which is closer to the real world, especially for athletes.
Abbreviations
- ACL:
-
anterior cruciate ligament
- ICC:
-
intraclass correlation coefficient
- TDPM:
-
threshold to detection of passive motion
References
Ageberg E (2002) Consequences of a ligament injury on neuromuscular function and relevance to rehabilitation - using the anterior cruciate ligament-injured knee as model. J Electromyogr Kinesiol 12(3):205–212
Ageberg E, Flenhagen J, Ljung J (2007) Test-retest reliability of knee kinesthesia in healthy adults. BMC Musculoskelet Disord 3(8):57
Anders JO, Venbrocks RA, Weinberg M (2008) Proprioceptive skills and functional outcome after anterior cruciate ligament reconstruction with a bone-tendon-bone graft. Int Orthop 32(5):627–633
Angoules AG, Mavrogenis AF, Dimitriou R, Karzis K, Drakoulakis E, Michos J, Papagelopoulos PJ (2011) Knee proprioception following ACL reconstruction; a prospective trial comparing hamstrings with bone-patellar tendon-bone autograft. Knee 18(2):76–82
Baumeister J, Reinecke K, Weiss M (2008) Changed cortical activity after anterior cruciate ligament reconstruction in a joint position paradigm: an EEG study. Scand J Med Sci Sports 18(4):473–484
Ben Moussa Zouita A, Zouita S, Dziri C, Ben Salah FZ, Zehi K (2008) Evaluation isocinétique, fonctionnelle et proprioceptive du footballeur à deux ans postopératoire d la reconstruction du ligament croisé antérieur du genou. Ann Phys Rehabil Med 51(4):248–256
Boerboom AL, Huizinga MR, Kaan WA, Stewart RE, Hof AL, Bulstra SK, Dierks RL (2008) Validation of a method to measure the proprioception of the knee. Gait Posture 28(4):610–614
Bonfim TR, Grossi DB, Paccola CA, Barela JA (2008) Additional sensory information reduces body sway of individuals with anterior cruciate ligament injury. Neurosci Lett 441(3):257–260
Bonfim TR, Jansen Paccola CA, Barela JA (2003) Proprioceptive and behavior impairments in individuals with anterior cruciate ligament reconstructed knees. Arch Phys Med Rehabil 84(8):1217–1223
Borsa PA, Lephart SM, Irrgang JJ, Safran MR, Fu FH (1997) The effects of joint position and direction of joint motion on proprioceptive sensibility in anterior cruciate ligament-deficient athletes. Am J Sports Med 25(3):336–340
Courtney CA, Rine RM (2006) Central somatosensory changes associated with improved dynamic balance in subjects with anterior cruciate ligament deficiency. Gait Posture 24(2):190–195
Dauty M, Collon S, Dubois C (2010) Change in posture control after recent knee anterior cruciate ligament reconstruction? Clin Physiol Funct Imaging 30(3):187–191
Denti M, Randelli P, Lo Vetere D, Moioli M, Bagnoli I, Cawley PW (2000) Motor control performance in the lower extremity: normals vs. anterior cruciate ligament reconstructed knees 5-8 years from the index surgery. Knee Surg Sports Traumatol Arthrosc 8(5):296–300
Fremerey RW, Lobenhoffer P, Zeichen J, Skutek M, Bosch U, Tscherne H (2000) Proprioception after rehabilitation and reconstruction in knees with deficiency of the anterior cruciate ligament: a prospective longitudinal study. J Bone Joint Surg Br 82(6):801–806
Friden T, Roberts D, Ageberg E, Walden M, Zatterstrom R (2001) Review of knee proprioception and the relation to extremity function after an anterior cruciate ligament rupture. J Orthop Sports Phys Ther 31(10):567–576
Friden T, Roberts D, Zatterstrom R, Lindstrand A, Moritz U (1996) Proprioception in the nearly extended knee Measurements of position and movement in healthy individuals and in symptomatic anterior cruciate ligament injured patients. Knee Surg Sports Traumatol Arthrosc 4(4):217–224
Friden T, Roberts D, Zatterstrom R, Lindstrand A, Moritz U (1997) Proprioception after an acute knee ligament injury: a longitudinal study on 16 consecutive patients. J Orthop Res 15(5):637–644
Friden T, Roberts D, Zatterstrom R, Lindstrand A, Moritz U (1999) Proprioceptive defects after an anterior cruciate ligament rupture -- the relation to associated anatomical lesions and subjective knee function. Knee Surg Sports Traumatol Arthrosc 7(4):226–231
Gauffin H, Pettersson G, Tegner Y, Tropp H (1990) Function testing in patients with old rupture of the anterior cruciate ligament. Int J Sports Med 11(1):73–77
Harrison EL, Duenkel N, Dunlop R, Russell G (1994) Evaluation of single-leg standing following anterior cruciate ligament surgery and rehabilitation. Phys Ther 74(3):245–252
Henriksson M, Ledin T, Good L (2001) Postural control after anterior cruciate ligament reconstruction and functional rehabilitation. Am J Sports Med 29(3):359–366
Jennings AG (1994) A proprioceptive role for the anterior cruciate ligament: a review of the literature. J Orthopaedic Rheumatol 7:3–13
Kapreli E, Athanasopoulos S (2006) The anterior cruciate ligament deficiency as a model of brain plasticity. Med Hypotheses 67(3):645–650
Lysholm M, Ledin T, Odkvist LM, Good L (1998) Postural control--a comparison between patients with chronic anterior cruciate ligament insufficiency and healthy individuals. Scand J Med Sci Sports 8(6):432–438
Mattacola CG, Perrin DH, Gansneder BM, Gieck JH, Saliba EN, McCue FC (2002) Strength, functional outcome, and postural stability after anterior cruciate ligament reconstruction. J Athl Train 37(3):262–268
Micheo W, Hernandez L, Seda C (2010) Evaluation, management, rehabilitation, and prevention of anterior cruciate ligament injury: current concepts. PM R 2(10):935–944
Muaidi QI, Nicholson LL, Refshauge KM (2009a) Do elite athletes exhibit enhanced proprioceptive acuity, range and strength of knee rotation compared with non-athletes? Scand J Med Sci Sports 19(1):103–112
Muaidi QI, Nicholson LL, Refshauge KM, Adams RD, Roe JP (2009b) Effect of anterior cruciate ligament injury and reconstruction on proprioceptive acuity of knee rotation in the transverse plane. Am J Sports Med 37(8):1618–1626
Ozenci AM, Inanmaz E, Ozcanli H, Soyuncu Y, Samanci N, Dagseven T, Balci N, Gur S (2007) Proprioceptive comparison of allograft and autograft anterior cruciate ligament reconstructions. Knee Surg Sports Traumatol Arthrosc 15(12):1432–1437
Pap G, Machner A, Nebelung W, Awiszus F (1999) Detailed analysis of proprioception in normal and ACL-deficient knees. J Bone Joint Surg Br 81(5):764–768
Pitman MI, Nainzadeh N, Menche D, Gasalberti R, Song EK (1992) The intraoperative evaluation of the neurosensory function of anterior cruciate ligament in humans using somatosensory evoked potentials. Arthroscopy 8(4):442–447
Reider B, Arcand MA, Diehl LH, Mroczek K, Abulencia A, Stroud CC, Palm M, Gilbertson J, Staszak P (2003) Proprioception of the knee before and after anterior cruciate ligament reconstruction. Arthroscopy 19(1):2–12
Riemann BL, Lephart SM (2002) The sensorimotor system, part I: the physiologic basis of functional joint stability. J Athl Train 37(1):71–79
Riemann BL, Myers JB, Lephart SM (2002) Sensorimotor system measurement techniques. J Athl Train 37(1):85–98
Schultz RA, Miller DC, Kerr CS, Micheli L (1984) Mechanoreceptors in human cruciate ligaments. A histological study. J Bone Joint Surg Am 66(7):1072–1076
Valeriani M, Restuccia D, Dilazzaro V et al (1996) Central nervous system modifications in patients with lesion of the anterior cruciate ligament of the knee. Brain 119:1751–1762
Valeriani M, Restuccia D, Dilazzaro V et al (1999) Clinical and neurophysiological abnormalities before and after reconstruction of the anterior cruciate ligament of the knee. Acta Neurol Scand 99:303–307
Zouita Ben Moussa A, Zouita S, Dziri C, Ben Salah FZ (2009) Single-leg assessment of postural stability and knee functional outcome two years after anterior cruciate ligament reconstruction. Ann Phys Rehabil Med 52(6):475–484
Acknowledgements
The authors thank Dr. Sarah MacKenzie who provided medical writing services (funded by Ramsay Générale de Santé).
Ethical approval and consent to participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Funding
Funding was provided by Ramsay Générale de Santé.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Laboute, E., Verhaeghe, E., Ucay, O. et al. Evaluation kinaesthetic proprioceptive deficit after knee anterior cruciate ligament (ACL) reconstruction in athletes. J EXP ORTOP 6, 6 (2019). https://doi.org/10.1186/s40634-019-0174-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40634-019-0174-8