Abstract
Purposes
Acetabular fractures are more and more common in the elderly. Open reduction and internal fixation (ORIF) may lead to poor outcomes and high revision rates. Primary total hip arthroplasty (THA) combined with internal fixation, also known as the combined hip procedure (CHP), associated with dual mobility cup (DM-CHP) could be an efficient procedure in selected elderly patients. The aim of this study is to compare functional and radiological outcomes between ORIF and DM-CHP.
Methods
Between 2007 and 2018, 51 patients older than 65 years were surgically treated for acetabular fractures. Twenty-six patients were treated by DM-CHP and 25 by ORIF. Each group was divided into two subgroups regarding a single or combined approach. Hospital stay, surgical time, intraoperative blood loss, and complications were documented. The Harris Hip Score (HHS) was used for measuring the functional outcome. Radiological analysis was used to assess the centre of rotation in the DM-CHP group.
Results
Median surgery time and intra-operative blood loss were higher in DM-CHP than those in ORIF. Early medical complication rate was higher for a combined approach as compared with a single posterior approach in DM-CHP (p = 0.003). Dislocation rate was 7.7% in DM-CHP. Revision rate was higher in ORIF (20% versus 7.7%). HHS was similar in both groups.
Conclusions
DM-CHP leads to similar functional outcomes and less revision than ORIF. This study strengthens the practice of using only the posterior approach for primary THA in the elderly. Dual mobility is a valid therapeutic option for acetabular fractures in elderly patients.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Avoid common mistakes on your manuscript.
Introduction
Acetabular fractures in patients aged 60 years and older have steadily become more frequent with a report of a 2.4-fold increase in incidence [1]. Kannus et al. [2] have also shown a rise of 23% of osteoporotic pelvic fractures with an ever older population. Low-energy trauma (LE) accounts for more than 50% of elderly acetabular fractures [3], which normally lead to a “senior fracture pattern”. This pattern consists of a displaced anterior column fracture associated with a posterior column fragment with a large portion of the quadrilateral surface displaced medially and cranially [1].
Some studies have shown that there are predictable factors of poor outcome concerning open reduction and internal fixation (ORIF), namely, age and non-anatomical reduction [4], superior anteromedial dome impaction [5], involvement of the posterior wall with marginal impaction or comminution [6], and femoral head damage [7]. About 17% of the patients [8] will need secondary total hip arthroplasty (THA) after acetabular fracture treated by ORIF. This surgery can be technically difficult and lead to high complication rates [9].
ORIF associated with primary THA, also known as the “ combined hip procedure” (CHP), seems to be an attractive procedure with satisfactory results in selected patients [10,11,12,13] and lead to equivalent non-fatal complication rate as ORIF [8]. Compared with ORIF, there is no need for an anatomic reduction, but there must be an adequate stability and bone stock to achieve THA. This surgical procedure allows for early mobilization with total weight-bearing [12], which should theoretically lead to fewer post-operative complications [14].
Dislocation rate in acetabular fractures treated by acute THA can run up to 23% [11, 15]. Dual mobility cups (DMC) are associated with lower rates of dislocation in primary surgery [16], revision surgery [17], and in primary THA for femoral neck fractures [18]. DMC could therefore be a useful tool for acetabular fractures.
Our hypothesis is that dual mobility-combined hip procedure (DM-CHP) is a safe procedure, with comparable clinical results and less early revision rate than ORIF in selected patients older than 65 years treated for acetabular fractures.
The aim of this study is to compare the functional and radiological outcomes between DM-CHP versus ORIF in consecutive patients older than 65 years treated for acetabular fractures.
Patients and methods
Patients
We retrospectively reviewed in our level I trauma department consecutively patients older than 65 years with acetabular fracture on a native hip who were treated surgically with ORIF or DM-CHP from January 2007 to September 2018.
Patients were divided into two groups based on two surgical methods: ORIF and DM-CHP. The indications for DM-CHP were severe comminuted articular fractures and marginal impaction (especially in weight-bearing area), fracture displacement of more than 20 mm, concomitant femoral head or neck fracture, marked osteoporosis (Singh index ≤ 2), and pre-existing symptomatic hip degenerative joint disease. ORIF group was divided into two subgroups: operated by a single approach (SA-ORIF) (anterior or posterior) and operated by a combined approach (CA-ORIF) (anterior and posterior). DM-CHP was subdivided in a single approach (SA-CHP) and combined approach (CA-CHP).
Surgical procedure
Surgery was done by two of our senior lower limb trauma surgeons. For the ORIF group, the surgical approach was decided depending on the fracture pattern [19]. When the anterior column was involved, a modified Stoppa approach was realized. For posterior column or posterior wall fractures, the Kocher-Langenbeck approach was performed. Finally, in both column fractures, anterior followed by posterior approaches were used. Osteosynthesis was realized with a suprapectineal quadrilateral buttress plate (PRO Quadrilateral surface plates, Stryker®, Kalamazoo, MC, USA) when anterior column was involved and by a reconstruction plate (Matta pelvic plates, Stryker®, Kalamazoo, MC, USA) or one-third tubular plate (DePuySynthes®, New Brunswick, NJ, USA) when posterior column or wall was involved. For four patients, the outer window of the ilioinguinal approach was used in combination with a modified Stoppa approach.
In the DM-CHP group, osteosynthesis was done first, followed by the THA. When the anterior column was involved, a modified Stoppa approach was realized, and osteosynthesis was done with a suprapectineal quadrilateral buttress plate. Then, the patient was positioned in lateral decubitus, and a Kocher-Langenbeck approach was used for posterior column or wall osteosynthesis followed by the THA. When the anterior column was not involved, Kocher-Langenbeck approach was performed with posterior column or wall osteosynthesis followed by THA. Arthroplasty involved an acetabular reinforcement ring (Ganz ring, Zimmer-Biomet®, Warsaw, Indiana, USA) with a cemented dual mobility cup (Symbol cup DM, Dedienne santé®, Mauguio, France). Various stems were used throughout the study period (Symbios®, Yverdon-les-Bains, Switzerland). Stems were cemented or uncemented regarding the proximal femur bone quality.
Clinical and radiological assessment
Characteristics of patients included age, gender, American Society of Anesthesiologists score (ASA), Charlson comorbidity index (CCI) [20], fracture patterns, Singh index, energy of trauma, surgery time, intra-operative blood loss, postoperative length of stay, early medical complications, surgical site infection, dislocation rate, late complications, Harris hip score (HHS), surgical revision, analysis of post-operative radiographs, and computed tomography (CT).
Follow-up time was calculated from the day of surgery to the date of the most recent visit or when the patient died. Charlson comorbidity index were divide into 3 groups according to the scores: 0, 1–3, and > 4 [20]. The surgical approach, surgery time (incision to end of wound closure), and intra-operative blood loss were retrospectively obtained from the surgical and anaesthesiologic reports. Post-operative length of stay (defined as the number of calendar days from the operation to hospital discharge), early medical complications (from the surgery day to 6 weeks), surgical site infection, dislocations, osteoarthritis, surgery revision, heterotopic ossification (HO), and post-operative functional outcome score (Harris Hip Score) were retrospectively reviewed from the medical reports.
Fracture patterns were classified by two fellowship trained senior surgeons according to the Letournel classification [19] and the AO classification (Arbeitsgemeinschaft für Osteosynthesefragen) on pre-operative X-rays and CT scan. The Singh index was evaluated on pre-operative anteroposterior pelvic X-rays. The lower index of both femurs was taken as reference. For the ORIF group, the quality of postoperative fracture reduction was analyzed by CT scan examining the largest remaining gap [4]. The reduction quality was expressed in millimeters (mm). A gap between fracture fragments of ≤ 2 mm was considered as anatomic.
Anteroposterior pelvic, obturator, and iliac view X-rays for ORIF were assessed at every clinical follow-up searching for osteoarthritis, osteonecrosis, loss of reduction, and HO. Concerning DM-CHP, radiologic follow-up was assessed by anteroposterior pelvic X-ray and axial X-ray of the operated hip searching for loosening and HO. The degree of HO was evaluated using the Brooker classification [21]. The biomechanical centre of rotation (COR) reconstruction was calculated as the difference from the contralateral hip [10] with TraumaCad® software (Brainlab®, Munich, Germany).
Statistical analysis
Continuous variables with normal distribution (age, HHS) were presented as mean and standard deviation. Continuous variables with non-normal distribution (intra-operative blood loss, surgery time, length of post-operative stay) were presented as median values and range. Categorical variables were presented as proportions. The Fischer exact test was used for hypothesis testing of binary variables, and the Mann Whitney U test or Student t test was used for continuous variables. Binary logistic regression was used to assess the correlation between CCI and early complications rate in the two groups (odds ratio with the 95% confidence interval (CI). The relationship between HHS and COR reconstruction was assessed by the Pearson correlation coefficient. All analyses were performed using STATA 15.0 soft-ware (StataCorp, College Station, TX, USA), and a P value of < 0.05 was considered significant.
Results
DM-CHP versus ORIF
Fifty-one patients met the inclusion criteria, from whom 25 patients were treated with ORIF and 26 with DM-CHP. Characteristics of both groups, including age, CCI, ASA score, and fracture patterns were similar. Gender distribution showed that the frequency of men was 80% (20/25) in the ORIF group compared with 58% (15/26) in the DM-CHP group (p = 0.09, Table 1).
Surgical approaches are reported in Table 1. Median surgery time (p < 0.001) and intra-operative blood loss (p = 0.006) were higher in the DM-CHP group. The length of post-operative stay, HHS, early complication rate, and infection rate were similar (Table 1).
Early complications are summarized in Table 2. We recorded one death due to cardiac arrest following a Mendelson syndrome in the ORIF group during hospital stay and another one from unrelated cause after hospital stay in DM-CHP.
In the ORIF group, the anatomical reduction was observed in 72% (18/25 patients). The rate of post-operative secondary arthritis was 32% (9/25 patients) looking at all fracture patterns, with 87.5% in associated fracture patterns.
The revision rate was 20% (5/25) in the ORIF group compared with 7.7% (2/26) in the DM-CHP group (Table 1). Reasons for revisions in ORIF were four secondary THA (three symptomatic osteoarthritis and one osteonecrosis) and one early infection. The four fracture patterns that needed secondary THA were as follow: one comminuted posterior wall fracture, two T-type fractures with severe dome comminution, and one anterior column with posterior hemi-transverse (AC-PHT) fracture (Fig. 1). The median time between ORIF and secondary THA was 11 months (range 6–24). Reasons for revisions in DM-CHP were two early infections. Two dislocations occurred: one early (2 weeks post-operative) and one delayed (1-year post-operative) due to a fall. Both unique dislocations were managed successfully by closed reduction.
Pre-operative coronal, sagittal and axial views (a, b and c) on CT scan of an 87-year-old male patient who sustained an anterior column with posterior hemi-transverse fracture. (d, e, and f) Post-operative anteroposterior, obturator, and iliac X-rays after ORIF. (g) Anteroposterior pelvic X-ray at 15 months of follow-up showing osteonecrosis of the femoral head and acetabular collapse. (h) Anteroposterior pelvic X-ray after secondary THA with dual mobility cup.
Subgroups analysis
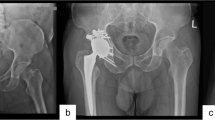
There were 21 patients in the SA-ORIF group and four patients in the CA-ORIF group. There were 18 patients in the SA-CHP group (Fig. 2) and eight patients in the CA-CHP group (Fig. 3). Mean surgery time and intra-operative blood loss were higher for combined approaches in each group. Early complication rate was 11.1% (2/18) in SA-CHP compared with 75% (6/8) in CA-CHP (p = 0.003). Early complication rate was 28.6% (6/21) in SA-ORIF compared with 50% (2/4) in CA-ORIF (p = 0.34) (Table 2).
Pre-operative axial (a) and coronal (b) views on CT scan of an 82-year-old female patient who sustained a comminuted posterior wall fracture associated with posterior hip dislocation treated by DM-CHP with posterior approach only (SA-CHP). Post-operative anteroposterior pelvic (c) and axial hip (d) X-rays at 12 months of follow-up post-SA-CHP.
Pre-operative coronal, sagittal and axial views (a, b, and c) on CT scan of an 87-year-old female patient who sustained a both column fracture treated by DM-CHP with combined approach (CA-CHP). Anteroposterior pelvic (d) and axial hip (e) X-rays at 24 months of follow-up after CA-CHP showing implants in good position.
The COR reconstruction measurements for DM-CHP are provided in Table 3. There was no statistically correlation between HHS and COR reconstruction.
Discussion
This study showed no difference in term of functional outcome (HHS), non-fatal complication rate, and infection rate between ORIF and DM-CHP, which is in accordance with the systematic review of Capone et al. [8]
Our results showed a significantly higher blood loss and higher surgery time for the DM-CHP group. The subgroup analysis also showed higher blood loss and longer surgery time for the combined approach in both groups. Moreover, there was a statistically correlation between medical complication rate and combined approaches in the DM-CHP group which can be explained by the higher blood loss and increased surgery time due to the double approach and patient repositioning during surgery. In our study, 56% of all fractures involved the anterior column, and stabilization of this part of the acetabulum could not be achieved using a posterior approach [15]. Inspired by Tidemark’s work on primary THA with Burch-Schneider antiprotrusion cage [22], Boelch et al. [10] have implanted nine primaries THA by single approach (Bauer or Kocher-Langenbeck). The stability of the posterior column was one of the essential factors of the surgical strategy. More recently, Lont et al. [14] had shown the importance of posterior column stabilization associated with the prevention of central migration using a posterior column plate and an antiprotrusion cage. Stabilization of the posterior column only in acute THA leads to reduced operation time, easier approach, and low post-operative complications [14]. Mean surgery time was lower [10, 14, 22], mean blood loss was lower [10] or similar [14, 22], and mean HHS was higher for Tidemark et al. [22] in comparison with our CA-CHP group. On the other hand, Rickman et al. [12] used combined approaches on 20 elderly patients with only two post-operative complications. The mean surgery time was 193 minutes [12] compared with 212 minutes in our CA-CHP group. Our study strengthens the practice of using only the posterior approach for CHP in the elderly who sustained acetabular fractures.
In the present study, the anatomical reduction was obtained in more than 70% of all the 25 cases, which probably explains the relatively low rate of conversion to secondary THA (16%) [8]. All of our secondary THA after ORIF presented predictors of poor outcomes, namely, one posterior wall comminution, and three supero-medial (quadrilateral plate) comminutions (2 T-type fractures and 1 AC-PHT fracture). Kreder et al. [6] published that 54% of early hip replacement were done after primary ORIF for complicated posterior wall. Fica et al. [23] observed that T-type fractures were associated with poor clinical outcome. On the other hand, Matta et al. [4] have found 77% of good or excellent clinical results for 31 T-type fractures. Quadrilateral plate comminution was associated with poor post-operative reduction and low HHS [24]. We reported a higher revision rate in the ORIF group than in the DM-CHP group essentially represented by secondary THA, which is in accordance with the results of others study [10, 14] and systematic review [8].
Dislocation was one of the most common complications in primary THA for acetabular fracture, together with infection and HO. Herscovici et al. [15] reported a 23% dislocation rate in 22 elderly patients, which lead to five revisions. On the other hand, Salama et al. [11] reported no cases of dislocation in their series of 18 patients. We found only one study which mentioned DMC as a primary implant for THA for acetabular fractures in the elderly [13], with a dislocation rate of 11% in a cohort of 27 patients. Our dislocation was 7.7% (2/26) with non-surgical management in both cases. The theoretical aim of DMC is to increase stability by allowing a large, effective head-to-neck ratio, and by creating two articulating surfaces [25]. There are some well-described THA instability risk factors related to patients, implants, and surgical techniques. COR and offset reconstruction are two of the major factors involved in THA stability. One study recorded the biomechanical reconstruction of their acute THA for acetabular fractures [10] and showed relevant variations in the COR reconstruction. This coincides with our results. Their dislocation rate was 22% [10]. Our low dislocation rate could also be partially explained by the use of DMC. Outcomes of DMC were evaluated, especially in femoral neck fracture, showing a reduced revision risk for DMC THA due to dislocation [18].
This study has some limitations. It is a retrospective study with a small number of patients. In addition, the pre-operative functional scores of the hip (HHS) were not assessed, which would probably yield a useful perspective on the post-operative HHS score. Moreover, median follow-up times were relatively low. Thus, results and conclusions do not explore mid-term and long-term outcomes.
Conclusion
DM-CHP has a similar short-term functional outcome compared with ORIF. Early medical complications are significantly higher when DM-CHP was performed with combined approaches due to higher blood loss and longer surgical time. Our study supports the importance of posterior approach only in acute THA for acetabular fracture in the elderly. Furthermore, this procedure leads to less revision than ORIF. To our knowledge, this is the first study which evaluates the potential of DMC in primary THA for acetabular fractures. DMC should have a place in the therapeutic option for acetabular fractures in high dislocation risk populations like elderly patients. DM-CHP could be a good therapeutic option in selected patients who are at risk of poor outcomes with ORIF and in case of higher instability risk. Further investigations and longer follow-up are necessary to confirm this conclusion.
References
Ferguson TA, Patel R, Bhandari M, Matta JM (2010) Fracture of the acetabulum in patients aged 60 years and older: an epidemiological and radiological study. J Bone Joint Surg (Br) 92-B:250–257. https://doi.org/10.1302/0301-620X.92B2.22488
Kannus P, Palvanen M, Niemi S, Parkkari J, Järvinen M (2000) Epidemiology of osteoporotic pelvic fractures in elderly people in Finland: sharp increase in 1970-1997 and alarming projection for the new millennium. Osteoporos Int 11(5):443–448. https://doi.org/10.1007/s001980070112
Dyskin E, Hill BW, Torchia MT, Cole PA (2019) A survey of high- and low-energy acetabular fractures in elderly patients. Geriatr Orthop Surg Rehabil 10:2151459319870426. https://doi.org/10.1177/2151459319870426
Matta JM (1996) Fractures of the acetabulum: accuracy of reduction and clinical results in patients managed operatively within three weeks after the injury. J Bone Joint Surg Am 78(11):1632–1645
Laflamme GY, Hebert-Davies J, Rouleau D, Benoit B, Leduc S (2011) Internal fixation of osteopenic acetabular fractures involving the quadrilateral plate. Injury 42(10):1130–1134. https://doi.org/10.1016/j.injury.2010.11.060
Kreder HJ, Rozen N, Borkhoff CM, Laflamme YG et al (2006) Determinants of functional outcome after simple and complex acetabular fractures involving the posterior wall. J Bone Joint Surg (Br) 88(6):776–782. https://doi.org/10.1302/0301-620X.88B6.17342
Clarke-Jenssen J, Røise O, Storeggen SAØ, Madsen JE (2017) Long term survival and risk factors for failure of the native hip joint after operatively treated displaced acetabular fractures. Bone Joint J 99-B(6):834–340. https://doi.org/10.1302/0301-620X.99B6.BJJ-2016-1013.R1
Capone A, Peri M, Mastio M (2017) Surgical treatment of acetabular fractures in the elderly: a systematic review of the results. EFORT Open Rev 2:97–103. https://doi.org/10.1302/2058-5241.2.160036
Ranawat A, Zelken J, Helfet D, Buly R (2009) Total hip arthroplasty for posttraumatic arthritis after acetabular fracture. J Arthroplast 24(5):759–767. https://doi.org/10.1016/j.arth.2008.04.004
Boelch SP, Jordan MC, Meffert RH, Jansen H (2017) Comparison of open reduction and internal fixation and primary total hip replacement for osteoporotic acetabular fractures: a retrospective clinical study. Int Orthop 41(9):1831–1837. https://doi.org/10.1007/s00264-016-3260-x
Salama W, Mousa S, Khalefa A, Sleem A, Kenawey M, Ravera L, Masse A (2017) Simultaneous open reduction and internal fixation and total hip arthroplasty for the treatment of osteoporotic acetabular fractures. Int Orthop 41(1):181–189. https://doi.org/10.1007/s00264-016-3175-6
Rickmann M, Young J, Trompeter A, Pearce R, Hamilton M (2014) Managing acetabular fractures in the elderly with fixation and primary arthroplasty: aiming for early weightbearing. Clin Orthop Relat Res 472(11):3375–3382. https://doi.org/10.1007/s11999-014-3467-3
Giunta JC, Tronc C, Kerschbaumer G, Milaire M, Ruatti S, Tonetti J, Boudissa M (2019) Outcomes of acetabular fractures in the elderly: a five year retrospective study of twenty-seven patients with primary total hip replacement. Int Orthop 43(10):2383–2389. https://doi.org/10.1007/s00264-018-4204-4
Lont T, Nieminen J, Reito A, Pakarinen T-K, Pajamäki I, Eskelinen A, Laitinen MK (2019) Total hip arthroplasty, combined with a reinforcement ring and posterior column plating for acetabular fractures in elderly patients: good outcome in 34 patients. Acta Orthop 90(3):275–280. https://doi.org/10.1080/17453674.2019.1597325
Herscovici D Jr, Lindvall E, Bolhofner B, Scaduto JM (2010) The combined hip procedure: open reduction internal fixation combined with total hip arthroplasty for the management of acetabular fractures in the elderly. J Orthop Trauma 24(5):291–296. https://doi.org/10.1097/BOT.0b013e3181b1d22a
Boyer B, Philippot R, Geringer J, Farizon F (2012) Primary total hip arthroplasty with dual mobility socket to prevent dislocation: a 22-year follow-up of 240 hips. Int Orthop 36:511–518. https://doi.org/10.1007/s00264-011-1289-4
Grazioli A, Ek ET, Rüdiger HA (2012) Biomechanical concept and clinical outcome of dual mobility cups. Int Orthop 36(12):2411–2418. https://doi.org/10.1007/s00264-012-1678-3
Jobory A, Kärrholm J, Overgaard S, Becic Pedersen A, Hallan G et al (2019) Reduced revision risk for dual-mobility cup in total hip replacement due to hip fracture: a matched-pair analysis of 9,040 cases from the Nordic Arthroplasty Register Association (NARA). J Bone Joint Surg Am 101(14):1278–1285. https://doi.org/10.2106/JBJS.18.00614
Letournel E (1980) Acetabulum fractures: classification and management. Clin Orthop Relat Res 151:81–106
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40(5):373–383. https://doi.org/10.1016/0021-9681(87)90171-8
Brooker A, Bowerman J, Robinson R, Riley LJ (1973) Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Joint Surg Am 55:1629–1632
Tidemark J, Blomfeldt R, Ponzer S, Söderqvist A, Törnkvist H (2003) Primary total hip arthroplasty with a Burch-Schneider antiprotrusion cage and autologous bone grafting for acetabular fractures in elderly patients. J Orthop Trauma 17(3):193–197. https://doi.org/10.1097/00005131-200303000-00007
Fica G, Cordova M, Guzman L, Schweitzer D (1998) Open reduction and internal fixation of acetabular fractures. Int Orthop 22(6):348–351. https://doi.org/10.1007/s002640050275
Tosounidis TH, Gudipati S, Panteli M, Kanakaris NK, Giannoudis PV (2015) The use of buttress plates in the management of acetabular fractures with quadrilateral plate involvement: is it still a valid option? Int Orthop 39(11):2219–2226. https://doi.org/10.1007/s00264-015-2883-7
Darrith B, Courtney PM, Della Valle CJ (2018) Outcomes of dual mobility components in total hip arthroplasty: a systematic review of the literature. Bone Joint J 100-B(1):11–19. https://doi.org/10.1302/0301-620X.100B1.BJJ-2017-0462.R1
Funding
Open access funding provided by University of Lausanne.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Ethical approval
The Cantonal Ethics Committee VAUD (CER-VD Lausanne) approved the study. (BASEC Number: 2018–01416).
Disclaimer
There are no financial biases for any author. Any company had no influence of the study design, in- and exclusion of patients, and study results.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lannes, X., Moerenhout, K., Duong, H.P. et al. Outcomes of combined hip procedure with dual mobility cup versus osteosynthesis for acetabular fractures in elderly patients: a retrospective observational cohort study of fifty one patients. International Orthopaedics (SICOT) 44, 2131–2138 (2020). https://doi.org/10.1007/s00264-020-04757-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-020-04757-w