Abstract
Purpose
Our study aimed at evaluating age- and gender-specific references describing lower-limb alignment in a large population of children using an accurate and reliable method (EOS 2D/3D).
Methods
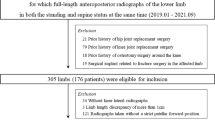
From our database, we selected 523 EOS records suitable for 3D modelling representing age groups between two and 16 years in which no relevant deviation influencing lower-limb biomechanics could be observed (the majority of the examined population had mild scoliosis). We performed reconstruction of both lower limbs, thus obtaining the value of the mechanical tibiofemoral angle (mTFA) and the femoral mechanical axis–femoral shaft angle (FM-FS) and calculated the anatomical tibiofemoral angle (aTFA) from previous parameters. Statistical analysis was carried out using the Kolmogorov–Smirnov test, Spearman correlation, regression analysis and Welch test.
Results
The aTFA reaches its maximum by the age of three years: 13.07° in boys and 10.73° in girls; it then varies ∼4.44° in both genders. By the age of three years, the mTFA reaches 8.04° in boys and 4.85° in girls; it starts to decrease to −1.47° in boys and 0.13° in girls. By the age of three years, FM-FS increases to 5.02° in boys, then fluctuates at ∼4.08°, while in girls, it increases to 5.87°, then fluctuates at ∼4.24°.
Conclusions
The pattern found in this study confirms the results of previous publications investigating Caucasian populations; however, absolute values differ significantly in several cases.




Similar content being viewed by others
References
Engel GM, Staheli LT (1974) The natural history of torsion and other factors influencing gait in childhood. A study of the angle of gait, tibial torsion, knee angle, hip rotation, and development of the arch in normal children. Clin Orthop Relat Res 99:12–17
Heath CH, Staheli LT (1993) Normal limits of knee angle in white children--genu varum and genu valgum. J Pediatr Orthop 13:259–262
Salenius P, Vankka E (1975) The development of the tibiofemoral angle in children. J Bone Joint Surg Am 57:259–261
Kraus VB, Vail TP, Worrell T et al (2005) A comparative assessment of alignment angle of the knee by radiographic and physical examination methods. Arthritis Rheum 52:1730–1735. doi:10.1002/art.21100
Cooke TD, Sled EA, Scudamore RA (2007) Frontal plane knee alignment: a call for standardized measurement. J Rheumatol 34:1796–1801
Thelen P, Delin C, Folinais D et al (2012) Evaluation of a new low-dose biplanar system to assess lower-limb alignment in 3D: a phantom study. Skeletal Radiol 41:1287–1293. doi:10.1007/s00256-012-1438-x
Sabharwal S, Zhao C (2009) The hip-knee-ankle angle in children: reference values based on a full-length standing radiograph. J Bone Joint Surg Am 91:2461–2468. doi:10.2106/JBJS.I.00015
Charpak G (1996) Prospects for the use in medicine of new detectors of ionizing radiation. Bull Acad Natl Med 180:161–168, discussion 168-169
Illés T, Somoskeöy S (2012) The EOS™ imaging system and its uses in daily orthopaedic practice. Int Orthop 36:1325–1331. doi:10.1007/s00264-012-1512-y
Deschênes S, Charron G, Beaudoin G et al (2010) Diagnostic imaging of spinal deformities: reducing patients radiation dose with a new slot-scanning X-ray imager. Spine (Phila Pa 1976) 35:989–994. doi:10.1097/BRS.0b013e3181bdcaa4
Dietrich TJ, Pfirrmann CW, Schwab A et al (2013) Comparison of radiation dose, workflow, patient comfort and financial break-even of standard digital radiography and a novel biplanar low-dose X-ray system for upright full-length lower limb and whole spine radiography. Skeletal Radiol 42:959–967. doi:10.1007/s00256-013-1600-0
Chaibi Y, Cresson T, Aubert B et al (2012) Fast 3D reconstruction of the lower limb using a parametric model and statistical inferences and clinical measurements calculation from biplanar X-rays. Comput Methods Biomech Biomed Engin 15:457–466. doi:10.1080/10255842.2010.540758
Assi A, Chaibi Y, Presedo A et al (2013) Three-dimensional reconstructions for asymptomatic and cerebral palsy children’s lower limbs using a biplanar X-ray system: a feasibility study. Eur J Radiol 82:2359–2364. doi:10.1016/j.ejrad.2013.07.006
Lazennec JY, Brusson A, Dominique F et al (2014) Offset and anteversion reconstruction after cemented and uncemented total hip arthroplasty: an evaluation with the low-dose EOS system comparing two- and three-dimensional imaging. Int Orthop. doi:10.1007/s00264-014-2616-3
Journé A, Sadaka J, Bélicourt C et al (2012) New method for measuring acetabular component positioning with EOS imaging: feasibility study on dry bone. Int Orthop 36:2205–2209. doi:10.1007/s00264-012-1650-2
Gheno R, Nectoux E, Herbaux B et al (2012) Three-dimensional measurements of the lower extremity in children and adolescents using a low-dose biplanar X-ray device. Eur Radiol 22:765–771. doi:10.1007/s00330-011-2308-y
Schlégl AT, Szuper K, Somoskeöy S et al (2014) Evaluation of the usefulness of the EOS 2D/3D system for the measurement of lower limbs anatomical and biomechanical parameters in children. Orv Hetil 155:1701–1712. doi:10.1556/OH.2014.30009
Szuper K, Schlégl Á, Leidecker E et al (2015) Three-dimensional quantitative analysis of the proximal femur and the pelvis in children and adolescents using an upright biplanar slot-scanning X-ray system. Pediatr Radiol 45:411–421. doi:10.1007/s00247-014-3146-2
Folinais D, Thelen P, Delin C et al (2013) Measuring femoral and rotational alignment: EOS system versus computed tomography. Orthop Traumatol Surg Res 99:509–516. doi:10.1016/j.otsr.2012.12.023
Winer BJ (1971) Statistical principles in experimental design. McGraw Hill, New York, pp 283–293
Saini UC, Bali K, Sheth B et al (2010) Normal development of the knee angle in healthy Indian children: a clinical study of 215 children. J Child Orthop 4:579–586. doi:10.1007/s11832-010-0297-z
Cheng JC, Chan PS, Chiang SC et al (1991) Angular and rotational profile of the lower limb in 2,630 Chinese children. J Pediatr Orthop 11:154–161
Cahuzac JP, Vardon D, Sales de Gauzy J (1995) Development of the clinical tibiofemoral angle in normal adolescents. A study of 427 normal subjects from 10 to 16 years of age. J Bone Joint Surg Br 77:729–732
Yoo JH, Choi IH, Cho TJ et al (2008) Development of tibiofemoral angle in Korean children. J Korean Med Sci 23:714–717. doi:10.3346/jkms.2008.23.4.714
Joubert K, Mag K, van’t Hof M et al (2006) The growth rate of height between the ages of 3 and 18 around the millennium in Hungary (on the basis of the Hungarian Nation-wide Representative Longitudinal Growth Study. Gyermekgyógy 5:517–527
Acknowledgments
No benefits in any form have been received or will be received from a commercial party related, directly or indirectly. The authors declare that there are no potential conflicts of interest in connection with this paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schlégl, Á.T., Szuper, K., Somoskeöy, S. et al. Three dimensional radiological imaging of normal lower-limb alignment in children. International Orthopaedics (SICOT) 39, 2073–2080 (2015). https://doi.org/10.1007/s00264-015-2851-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-015-2851-2