Abstract
Purpose
The purpose of the study is to evaluate the utility of apparent diffusion coefficient (ADC), chemical shift signal intensity index (SII), and contrast enhancement in distinguishing between benign lesions and renal cell carcinoma (RCC) and between subtypes of renal lesions.
Methods
This retrospective study included 98 renal lesions (≤ 3 cm) on MRI with correlative surgical pathology. Scanner field strength, lesion location, and size were recorded. Two readers blinded to surgical pathology independently measured ADC ratio (ADC lesion/ADC non-lesion kidney), SII, and absolute/relative enhancement in the corticomedullary and nephrographic phases of contrast.
Results
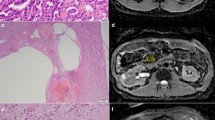
There were 76 malignant and 22 benign lesions. 42 RCC were clear cell (ccRCC), 19 papillary (pRCC), 5 chromophobe (cbRCC). Benign lesions included both solid and cystic lesions. Interreader agreement for all variables was good–excellent (ICC 0.70–0.91). There was no difference in ADC or SII between benign and malignant lesions. There was greater absolute corticomedullary enhancement of benign versus malignant lesions (150.0 ± 111.5 vs. 81.1 ± 74.8, p = 0.0115), which did not persist when excluding pRCC. For lesion subtype differentiation, ADCratio for pRCC was lower than benign lesions (0.74 ± 0.35 vs. 1.03 ± 0.46, p = 0.0246). ccRCC demonstrated greater SII than other RCC (0.09 ± 0.22 vs. 0.001 ± 0.26, p = 0.0412). Oncocytomas and angiomyolipoma (AML) showed greater absolute corticomedullary enhancement than ccRCC and pRCC (145.6 ± 65.2 vs. 107.2 ± 85.3, p = 0.043 and 186.2 ± 93.9 vs. 37.6 ± 35.3, p = 0.0108), respectively.
Conclusions
While corticomedullary-phase enhancement was a differentiating feature, quantitative metrics from diffusion and chemical shift imaging cannot reliably differentiate benign from malignant lesions. Quantitative assessment may be useful in differentiating some benign and malignant lesion subtypes.






Similar content being viewed by others
References
Collins S, McKiernan J, Landman J (2006) Update on the epidemiology and biology of renal cortical neoplasms. J Endourol 20(12):975–985. https://doi.org/10.1089/end.2006.20.975
Johnson DC, Vukina J, Smith AB, et al. (2015) Preoperatively misclassified, surgically removed benign renal masses: a systematic review of surgical series and United States population level burden estimate. J Urol 193(1):30–35. https://doi.org/10.1016/j.juro.2014.07.102
Ha SC, Zlomke HA, Cost N, Wilson S (2015) The past, present, and future in management of small renal masses. J Oncol 2015:364807. https://doi.org/10.1155/2015/364807
Volpe A, Cadeddu JA, Cestari A, et al. (2011) Contemporary management of small renal masses. Eur Urol 60(3):501–515. https://doi.org/10.1016/j.eururo.2011.05.044
Pedrosa I, Sun MR, Spencer M, et al. (2008) MR imaging of renal masses: correlation with findings at surgery and pathologic analysis. Radiographics 28(4):985–1003. https://doi.org/10.1148/rg.284065018
Karlo CA, Donati OF, Burger IA, et al. (2013) MR imaging of renal cortical tumours: qualitative and quantitative chemical shift imaging parameters. Eur Radiol 23(6):1738–1744. https://doi.org/10.1007/s00330-012-2758-x
Pierorazio PM, Hyams ES, Tsai S, et al. (2013) Multiphasic enhancement patterns of small renal masses (≤4 cm) on preoperative computed tomography: utility for distinguishing subtypes of renal cell carcinoma, angiomyolipoma, and oncocytoma. Urology 81(6):1265–1271. https://doi.org/10.1016/j.urology.2012.12.049
Sandrasegaran K, Sundaram CP, Ramaswamy R, et al. (2010) Usefulness of diffusion-weighted imaging in the evaluation of renal masses. AJR Am J Roentgenol 194(2):438–445. https://doi.org/10.2214/AJR.09.3024
Mirka H, Korcakova E, Kastner J, et al. (2015) Diffusion-weighted imaging using 3.0 T MRI as a possible biomarker of renal tumors. Anticancer Res 35(4):2351–2357
Erbay G, Koc Z, Karadeli E, et al. (2012) Evaluation of malignant and benign renal lesions using diffusion-weighted MRI with multiple b values. Acta Radiol 53(3):359–365. https://doi.org/10.1258/ar.2011.110601
Razek AA, Farouk A, Mousa A, Nabil N (2011) Role of diffusion-weighted magnetic resonance imaging in characterization of renal tumors. J Comput Assist Tomogr 35(3):332–336. https://doi.org/10.1097/RCT.0b013e318219fe76
Galmiche C, Bernhard JC, Yacoub M, et al. (2017) Is multiparametric MRI useful for differentiating oncocytomas from chromophobe renal cell carcinomas? AJR Am J Roentgenol 208(2):343–350. https://doi.org/10.2214/AJR.16.16832
Rosenkrantz AB, Hindman N, Fitzgerald EF, et al. (2010) MRI features of renal oncocytoma and chromophobe renal cell carcinoma. AJR Am J Roentgenol 195(6):W421–427. https://doi.org/10.2214/AJR.10.4718
Cornelis F, Tricaud E, Lasserre AS, et al. (2014) Routinely performed multiparametric magnetic resonance imaging helps to differentiate common subtypes of renal tumours. Eur Radiol 24(5):1068–1080. https://doi.org/10.1007/s00330-014-3107-z
Roy C, Sauer B, Lindner V, et al. (2007) MR Imaging of papillary renal neoplasms: potential application for characterization of small renal masses. Eur Radiol 17(1):193–200. https://doi.org/10.1007/s00330-006-0271-9
Patel HD, Druskin SC, Rowe SP, et al. (2017) Surgical histopathology for suspected oncocytoma on renal mass biopsy: a systematic review and meta-analysis. BJU Int 119(5):661–666. https://doi.org/10.1111/bju.13763
Taouli B, Thakur RK, Mannelli L, et al. (2009) Renal lesions: characterization with diffusion-weighted imaging versus contrast-enhanced MR imaging. Radiology 251(2):398–407. https://doi.org/10.1148/radiol.2512080880
Zhong Y, Wang H, Shen Y, et al. (2017) Diffusion-weighted imaging versus contrast-enhanced MR imaging for the differentiation of renal oncocytomas and chromophobe renal cell carcinomas. Eur Radiol. https://doi.org/10.1007/s00330-017-4906-9
Dhyani M, Grajo JR, Rodriguez D, et al. (2017) Aorta-Lesion-Attenuation-Difference (ALAD) on contrast-enhanced CT: a potential imaging biomarker for differentiating malignant from benign oncocytic neoplasms. Abdom Radiol (NY) 42(6):1734–1743. https://doi.org/10.1007/s00261-017-1061-3
Choi JH, Kim JW, Lee JY, et al. (2015) Comparison of computed tomography findings between renal oncocytomas and chromophobe renal cell carcinomas. Korean J Urol 56(10):695–702. https://doi.org/10.4111/kju.2015.56.10.695
Bird VG, Kanagarajah P, Morillo G, et al. (2011) Differentiation of oncocytoma and renal cell carcinoma in small renal masses (< 4 cm): the role of 4-phase computerized tomography. World J Urol 29(6):787–792. https://doi.org/10.1007/s00345-010-0586-7
Jinzaki M, Tanimoto A, Mukai M, et al. (2000) Double-phase helical CT of small renal parenchymal neoplasms: correlation with pathologic findings and tumor angiogenesis. J Comput Assist Tomogr 24(6):835–842
Young JR, Margolis D, Sauk S, et al. (2013) Clear cell renal cell carcinoma: discrimination from other renal cell carcinoma subtypes and oncocytoma at multiphasic multidetector CT. Radiology 267(2):444–453. https://doi.org/10.1148/radiol.13112617
Chen F, Gulati M, Hwang D, et al. (2017) Voxel-based whole-lesion enhancement parameters: a study of its clinical value in differentiating clear cell renal cell carcinoma from renal oncocytoma. Abdom Radiol (NY) 42(2):552–560. https://doi.org/10.1007/s00261-016-0891-8
Lee-Felker SA, Felker ER, Tan N, et al. (2014) Qualitative and quantitative MDCT features for differentiating clear cell renal cell carcinoma from other solid renal cortical masses. AJR Am J Roentgenol 203(5):W516–524. https://doi.org/10.2214/AJR.14.12460
Lim RS, Flood TA, McInnes MDF, Lavallee LT, Schieda N (2017) Renal angiomyolipoma without visible fat: can we make the diagnosis using CT and MRI? Eur Radiol. https://doi.org/10.1007/s00330-017-4988-4
Park JJ, Kim CK (2017) Small (< 4 cm) renal tumors with predominantly low signal intensity on T2-weighted images: differentiation of minimal-fat angiomyolipoma from renal cell carcinoma. AJR Am J Roentgenol 208(1):124–130. https://doi.org/10.2214/AJR.16.16102
Zhang YY, Luo S, Liu Y, Xu RT (2013) Angiomyolipoma with minimal fat: differentiation from papillary renal cell carcinoma by helical CT. Clin Radiol 68(4):365–370. https://doi.org/10.1016/j.crad.2012.08.028
Kim Y, Sung DJ, Sim KC, et al. (2017) Renal tumors with low signal intensities on T2-weighted MR image: radiologic-pathologic correlation. Abdom Radiol (NY) 42(8):2108–2118. https://doi.org/10.1007/s00261-017-1097-4
Yang CW, Shen SH, Chang YH, et al. (2013) Are there useful CT features to differentiate renal cell carcinoma from lipid-poor renal angiomyolipoma? AJR Am J Roentgenol 201(5):1017–1028. https://doi.org/10.2214/AJR.12.10204
Wang H, Cheng L, Zhang X, et al. (2010) Renal cell carcinoma: diffusion-weighted MR imaging for subtype differentiation at 3.0 T. Radiology 257(1):135–143. https://doi.org/10.1148/radiol.10092396
Hotker AM, Mazaheri Y, Wibmer A, et al. (2016) Use of DWI in the differentiation of renal cortical tumors. AJR Am J Roentgenol 206(1):100–105. https://doi.org/10.2214/AJR.14.13923
Yu X, Lin M, Ouyang H, Zhou C, Zhang H (2012) Application of ADC measurement in characterization of renal cell carcinomas with different pathological types and grades by 3.0T diffusion-weighted MRI. Eur J Radiol 81(11):3061–3066. https://doi.org/10.1016/j.ejrad.2012.04.028
Jhaveri KS, Elmi A, Hosseini-Nik H, et al. (2015) Predictive value of chemical-shift MRI in distinguishing clear cell renal cell carcinoma from non-clear cell renal cell carcinoma and minimal-fat angiomyolipoma. AJR Am J Roentgenol 205(1):W79–86. https://doi.org/10.2214/AJR.14.13245
Outwater EK, Bhatia M, Siegelman ES, Burke MA, Mitchell DG (1997) Lipid in renal clear cell carcinoma: detection on opposed-phase gradient-echo MR images. Radiology 205(1):103–107. https://doi.org/10.1148/radiology.205.1.9314970
Hindman N, Ngo L, Genega EM, et al. (2012) Angiomyolipoma with minimal fat: can it be differentiated from clear cell renal cell carcinoma by using standard MR techniques? Radiology 265(2):468–477. https://doi.org/10.1148/radiol.12112087
Agnello F, Roy C, Bazille G, et al. (2013) Small solid renal masses: characterization by diffusion-weighted MRI at 3 T. Clin Radiol 68(6):e301–308. https://doi.org/10.1016/j.crad.2013.01.002
Muller MF, Prasad PV, Bimmler D, Kaiser A, Edelman RR (1994) Functional imaging of the kidney by means of measurement of the apparent diffusion coefficient. Radiology 193(3):711–715. https://doi.org/10.1148/radiology.193.3.7972811
Siegel CL, Aisen AM, Ellis JH, Londy F, Chenevert TL (1995) Feasibility of MR diffusion studies in the kidney. J Magn Reson Imaging 5(5):617–620
Cova M, Squillaci E, Stacul F, et al. (2004) Diffusion-weighted MRI in the evaluation of renal lesions: preliminary results. Br J Radiol 77(922):851–857. https://doi.org/10.1259/bjr/26525081
Namimoto T, Yamashita Y, Mitsuzaki K, et al. (1999) Measurement of the apparent diffusion coefficient in diffuse renal disease by diffusion-weighted echo-planar MR imaging. J Magn Reson Imaging 9(6):832–837
Notohamiprodjo M, Reiser MF, Sourbron SP (2010) Diffusion and perfusion of the kidney. Eur J Radiol 76(3):337–347. https://doi.org/10.1016/j.ejrad.2010.05.033
Thoeny HC, De Keyzer F, Oyen RH, Peeters RR (2005) Diffusion-weighted MR imaging of kidneys in healthy volunteers and patients with parenchymal diseases: initial experience. Radiology 235(3):911–917. https://doi.org/10.1148/radiol.2353040554
Reuter VE, Tickoo SK (2010) Differential diagnosis of renal tumours with clear cell histology. Pathology (Phila) 42(4):374–383. https://doi.org/10.3109/00313021003785746
Acknowledgements
The authors acknowledge the administrative assistance of Denise Garcia.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was obtained for this study.
Conflict of interest
The authors have no potential conflicts of interest to disclose.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was waived by the institutional research committee for this HIPAA compliant retrospective study.
Rights and permissions
About this article
Cite this article
Yano, M., Fowler, K.J., Srisuwan, S. et al. Quantitative multiparametric MR analysis of small renal lesions: correlation with surgical pathology. Abdom Radiol 43, 3390–3399 (2018). https://doi.org/10.1007/s00261-018-1612-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-018-1612-2