Abstract
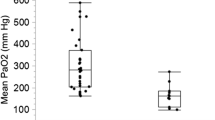
Hypercapnia has been reported to play an active role in protection against organ injury. The aim of this study was to determine whether a higher level of partial pressure of arterial carbon dioxide (PaCO2) within the normal range in pediatric patients undergoing cardiac surgery had a similar organ-protective effect. From May 2017 to May 2018, 83 consecutive infant patients undergoing ventricular septal defect (VSD) repair with cardiopulmonary bypass were retrospectively enrolled. We recorded the end-expiratory tidal partial pressure of carbon dioxide (Pet-CO2) as an indirect and continuous way to reflect the PaCO2. The patients were divided into a low PaCO2 group (LPG; 30 mmHg < Pet-CO2 < 40 mmHg) and a high PaCO2 group (HPG; 40 mmHg < Pet-CO2 < 50 mmHg). The regional cerebral oxygen saturation (rScO2), cerebral blood flow velocity (CBFV), and hemodynamics at five time points throughout the operation, and perioperative data were recorded and analyzed for the two groups. In total, 34 LPG and 49 HPG patients were included. Demographics and perioperative clinical data showed no significant difference between the groups. Compared with LPG, the HPG produced lower postoperative creatine kinase isoenzyme-MB (40.88 versus 50.34 ng/mL, P = 0.038). The postoperative C-reactive protein of HPG trended lower than in LPG (61.09 versus 73.4 mg/L, P = 0.056). The rScO2 and mean CBFV of HPG were significantly higher compared with LPG (P < 0.05) except at the end of cardiopulmonary bypass. Hemodynamic data showed no significant difference between the groups. As a convenient and safe approach, higher-normal PaCO2 could attenuate brain injury, heart injury, and inflammatory response in infant patients undergoing VSD repair.




Similar content being viewed by others
Abbreviations
- ABG:
-
Arterial blood gas
- BSA:
-
Body surface area
- CBFV:
-
Cerebral blood flow velocity
- CCE:
-
Cardiac cycle efficiency
- Ccr:
-
Creatinine clearance rate
- CHD:
-
Congenital heart disease
- CI:
-
Cardiac index
- CK:
-
Creatine kinase
- CKMB:
-
Creatine kinase isoenzyme-MB
- CPB:
-
Cardiopulmonary bypass
- CRP:
-
C-creative protein
- CS-AKI:
-
Cardiac surgery-associated kidney injury
- DiaP:
-
Diastolic blood pressure
- DicP:
-
Dicrotic blood pressure
- dp/dtmax :
-
Maximal slope of systolic upstroke
- FiO2 :
-
Fraction of inspire O2
- HCA:
-
Hypercapnic acidosis
- HPG:
-
High PaCO2 group
- ICAM:
-
Intracellular adhesion molecule
- ICU:
-
Intensive care unit
- IL:
-
Interleukin
- LPG:
-
Low PaCO2 group
- IS:
-
Inotropic score
- MCA:
-
Middle cerebral artery
- MV:
-
Minute volume
- NF:
-
Nuclear factor
- NIRS:
-
Near-infrared spectroscopy
- OI:
-
Oxygenation index
- PaCO2 :
-
Partial pressure of arterial carbon dioxide
- Pet-CO2 :
-
End-expiratory tidal partial pressure of carbon dioxide
- PPV:
-
Pulse pressure variation
- PRAM:
-
Pressure recording analytical method
- rScO2 :
-
Regional cerebral oxygen saturation
- SCr:
-
Serum creatinine
- SVRI:
-
Systemic vascular resistance index
- SysP:
-
Systolic blood pressure
- TCD:
-
Transcranial Doppler
- TNF:
-
Tumor necrosis factor
- TV:
-
Tidal volume
- V max :
-
Maximum flow velocity
- V mean :
-
Mean flow velocity
- V min :
-
Minimum flow velocity
- VSD:
-
Ventricular septal defect
- WBC:
-
White blood cell
References
Kollef MH, Wragge T, Pasque C (1995) Determinants of mortality and multiorgan dysfunction in cardiac surgery patients requiring prolonged mechanical ventilation. Chest 107(5):1395–1401
Balzer F, Sander M, Simon M, Spies C et al (2015) (2015) High central venous saturation after cardiac surgery is associated with increased organ failure and long-term mortality: an observational cross-sectional study. Crit Care 19:168
Stoppe C, Schälte G, Rossaint R, Coburn M et al (2011) The intraoperative decrease of selenium is associated with the postoperative development of multiorgan dysfunction in cardiac surgical patients. Crit Care Med 39(8):1879–1885
Laffey JG, Kavanagh BP (1999) Carbon dioxide and the critically ill–too little of a good thing? Lancet 354(9186):1283–1286
Xu F, Uh J, Brier MR et al (2011) The influence of carbon dioxide on brain activity and metabolism in conscious humans. J Cerebr Blood Flow Metab 31(1):58–67
Beaudin AE, Brugniaux JV, Vöhringer M, Flewitt J, Green JD, Friedrich MG, Poulin MJ (2011) Cerebral and myocardial blood flow responses to hypercapnia and hypoxia in humans. Am J Physiol-Heart C 301(4):H1678–H1686
Kregenow DA, Rubenfeld GD, Hudson LD, Swenson ER (2006) Hypercapnic acidosis and mortality in acute lung injury. Crit Care Med 34(1):1–7
Benumof JL, Wilson WC (2005) Anesthesia for thoracic surgery. In: Miller RD (ed) Miller's anesthesia. Churchill Livingstone, Philadelphia, pp 1847–1939
Bendixen HH, Hedley-Whyte J, Laver MB (1963) Impaired oxygenation in surgical patients during general anethesia with controlled ventilation. A concept of atelectasis. New Engl J Med 269:991–996
Kussman BD, Wypij D, Laussen P et al (2010) Relationship of intraoperative cerebral oxygen saturation to neurodevelopmental outcome and brain magnetic resonance imaging at 1 year of age in infants undergoing biventricular repair. Circulation 122:245–254
Spaeder MC, Klugman D, Skurow-Todd K, Glass P, Jonas RA, Donofrio MT (2017) Perioperative near-infrared spectroscopy monitoring in neonates with congenital heart disease: relationship of cerebral tissue oxygenation index variability with neurodevelopmental outcome. Pediatr Crit Care Med 18(3):213–218
Orihashi K, Sueda T, Okada K, Imai K (2004) Near-infrared spectroscopy for monitoring cerebral ischemia during selective cerebral perfusion. Eur J Cardio-Thorac Surg 26(5):907–911
Rowley AB, Ainslie PN, Poulin MJ, Payne SJ (2008) Multivariate system identification for cerebral autoregulation. Ann Biomed Eng 36(2):308–320
Noble L, Nesbitt K, Fallah S, Shah V, Shah PS (2005) Agreement of carbon dioxide levels measured by arterial, transcutaneous and end tidal methods in preterm infants %3c or = 28 weeks gestation. J Perinatol 25(1):26–29
Khan M, Abbasi S (2007) Arterial to end-tidal carbon dioxide difference in neurosurgical patients undergoing craniotomy: a review of practice. J Pak Med Assoc 57(9):446–448
Schwartz GJ, Haycock GB, Edelmann CM, Spitzer A (1976) A simple estimate of glomerular filtration rate in children derived from body length and plasma creatinine. Pediatrics 58(2):259–263
Hajjar LA, Volpe MS, Fukushima JT et al (2017) Effect of intensive vs moderate alveolar recruitment strategies added to lung-protective ventilation on postoperative pulmonary complications: a randomized clinical trial. JAMA 317(14):1422–1432
Wernovsky G, Wypij D, Jonas RA et al (1995) Postoperative course and hemodynamic profile after the arterial switch operation in neonates and infants. A comparison of low-flow cardiopulmonary bypass and circulatory arrest. Circulation 92(8):2226–2235
du Plessis AJ, Wessel DL, Jonas RA, Newburger JW (2002) Current incidence of acute neurologic complications after open-heart operations in children. Ann Thorac Surg 73(6):1752–1758
Freeman K, Glogowski K, Fogg S, Duncan KF (2005) The significance of baseline cerebral oxygen saturation in children undergoing congenital heart surgery. Am J Surg 190(2):260–263
Jobsis FF (1977) Noninvasive, infrared monitoring of cerebral and myocardial oxygen sufficiency and circulatory parameters. Science 198(4323):1264–1267
Austin EH, Edmonds HL, Auden SM, et al (1997) Benefit of neurophysiologic monitoring for pediatric cardiac surgery. J Thorac Cardiovasc Surg 114(5):707–715, 717
Brian JE (1998) Carbon dioxide and the cerebral circulation. Anesthesiology 88(5):1365–1386
Takada K, Tomizawa Y, Nishiyama K, Kawamata M, Ozaki M (2007) Permissive range of hypercapnia for improved peripheral microcirculation and cardiac output in rabbits. Crit Care Med 35(9):2171–2175
Pollock JM, Deibler AR, Whitlow CT et al (2008) Hypercapnia-induced cerebral hyperperfusion: an underrecognized clinical entity. Am J Neuroradiol 30:378–385
Quarti A, Nardone S, Manfrini F, D'Orfeo F, Genova S, Silvano R, Pozzi M (2013) Effect of the adjunct of carbon dioxide during cardiopulmonary bypass on cerebral oxygenation. Perfusion 28(2):152–155
Nomura F, Forbess JM, Mayer JE (1994) Effects of hypercarbic acidotic reperfusion on recovery of myocardial function after cardioplegic ischemia in neonatal lambs. Circulation 90:I321–I327
Cregg N, Engelberts D, Takeuchi A, Fedorko L, Kavanagh BP (1998) Hypercapnic acidosis may attenuate acute lung injury by inhibition of endogenous xanthine oxidase. Am J Resp Crit Care 158:1578–1584
Weil MH, Gazmuri RJ, Bisera J, Rackow EC (1991) Reversible impairment of myocardial contractility due to hypercarbic acidosis in the isolated perfused rat heart. Crit Care Med 19(2):218–224
West MA, Baker J, Bellingham J (1996) Kinetics of decreased LPS-stimulated cytokine release by macrophages exposed to CO2. J Surg Res 63(1):269–274
Takeshita K, Suzuki Y, Nishio K et al (2003) Hypercapnic acidosis attenuates endotoxin-induced nuclear factor-κB activation. Am J Respir Cell Mol 29(1):124–132
Hanouz JL, Le Manach Y, Gué X, Monier E, Guillou L, Riou B (2009) Simultaneous measurement of cardiac troponin I, B-type natriuretic peptide, and C-reactive protein for the prediction of long-term cardiac outcome after cardiac surgery. Anesthesiology 111(2):250–257
Al Aklabi M, Bhattacharya S, Cave D et al (2018) Cardiac surgery-associated kidney injury in children and renal oximetry. Pediatr Crit Care Med 19(9):839–845
Gores GJ, Nieminen AL, Wray BE, Herman B, Lemasters JJ (1989) Intracellular pH during “chemical hypoxia” in cultured rat hepatocytes. Protection by intracellular acidosis against the onset of cell death. J Clin Investig 83(2):386–396
Acknowledgements
We would like to acknowledge the physicians of the pediatric cardiac center of Beijing Anzhen Hospital.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
The institutional review board at Anzhen Hospital approved the use of clinical data for this study and the informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fan, F., Xie, S., Ou-Yang, C. et al. The Organ-Protective Effect of Higher Partial Pressure of Arterial Carbon Dioxide in the Normal Range for Infant Patients Undergoing Ventricular Septal Defect Repair. Pediatr Cardiol 41, 372–381 (2020). https://doi.org/10.1007/s00246-019-02269-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-019-02269-y