Abstract
The eyebrow is a complex structure of the human face, which has both functional (communication) and aesthetic aspects and contributes to a persons’ individual appearance. Ptosis of the eyebrow is a common condition, especially among the elderly and smokers. Facial appearance is disrupted by eyebrow ptosis, and in many cases, correction and treatment are needed. No specific type of browlift has been shown to be superior to another, and since there is a wide variation in treatment preference between patients, it requires an individual approach to each specific patient. This review provides an overview of the history of the browlift, non-surgical treatment and current surgical techniques available.
Level of evidence: Not ratable.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A common issue among the elderly is ptosis of the forehead or eyebrows. The muscles moving the eyebrows communicate a variety of emotions and gestures, which can be quickly identified. Properly aligned eyebrows with a mouth that is allowed to smile communicate an alert and rested state, lateral incline eyebrows transmit sadness, medial incline eyebrows transmit anger, drawn-up eyebrows convey surprise and low standing eyebrows convey exhaustion [1, 2].
The corrugator supercilii, depressor supercilii, orbicularis oculi and procerus muscles (brow depressor) and frontalis muscle (brow elevator) affect the position of the eyebrow [3]. Branches of the facial nerve supply the motor innervation. The frontal, superior part of the orbicularis oculi, the transverse head of the corrugator supercilii and the superior part of the procerus muscles are innervated by the temporal facial branch.
Complaints commonly associated with brow ptosis are a tired and heavy feeling of the eyes, resulting in a limited field of vision, increased tearing and difficulty reading or watching television and may transmit unintended gestures that can be misunderstood. In addition, constant stimulation of the scalp and forehead muscles can cause discomfort, headaches, rhytids and eyestrain [4]. Due to the low brow position, the skin of the upper eyelid is brought down and may be falsely interpreted as blepharochalasis [5, 6]. In these cases, an upper blepharoplasty might increase complaints if a browlift is performed in a later tempus, as there might not have been excess upper eyelid skin in the first place, resulting in an older, more tired or even angry appearance [5,6,7,8,9].
Many browlift techniques have been validated, but there is no gold standard treatment that is applicable to every individual needs. To recognise the patient’s characteristics and matching them to the technique best suited allow for maximal functional and aesthetic effect. Techniques range from only lifting (part of) the eyebrow to a full forehead lift [5, 10,11,12,13,14,15,16,17,18,19]. More traditional techniques (crescent skin excision) leave prominent scars cranial to the eyebrow [16,17,18,19,20,21]. Open techniques, such as the foreheadplasty or pretrichial procedures, take approximately the same amount of time as the endoscopic approaches and have the capacity to adapt to various wrinkles, creases and/or forehead hairline considerations [5]. The transpalpebral approach and the transblepharoplasty technique resect the corrugator muscles and divide the procerus muscle with several temporal incisions to elevate the lateral eyebrow [22, 23].
It is clear that patients wish an improvement in brow position, which provides a long-lasting and natural appearance. The visibility of the scars and also practical issues, such as the use of anaesthetic, procedure time (surgery and anaesthesia) and costs of the procedure influence the eventual decision.
The goal of this review is to give a clear overview of the development of eyebrow lifting techniques over time. This includes surgical and non-surgical methods. We searched the literature to provide an extensive summary of the most relevant techniques.
Review methodology
Despite the fact that this article is not a systematic review, a comprehensive search of the literature was undertaken. Cochrane Library, Medline and PubMed were searched until November 2020 using the terms ‘eye brow’, ‘brow lift’, ‘plastic surgery’, ‘cosmetic’ and ‘history’. The search was limited to English, Dutch and German language papers. Initial searches revealed > 4000 abstracts that were screened and approximately 60 papers were found eligible for this review. It has to be taken into account that despite the extensive literature search and the clinical and surgical expertise of the authors, not all techniques are covered.
History of the eyebrow lift
For almost a century, the (surgical) elevation of the brow is part of the aesthetic improvement of the aging process of the face [24]. The results of this procedure have improved over time and for the last decades, the endoscopic approach is in an upcoming fashion.
The first described browlift dates from 1919 where Passot used elliptical excisions to uplift the brows and to remove crow’s feet [24, 25]. In 1926, Hunt used the coronal incisions in the hairline and anterior to this point [24, 25]. Contrary to the coronal incisions, the parietal ones were not effective in removing rhytids [24]. Consecutive approaches were forehead lifting, several forms of undermining of the forehead and the implementation of grafts [24]. The classical coronal browlift was first described in 1933 by Claoué, who found that releasing the temporal ligaments at the lines of fusion would free up the arcus marginalis, permitting a greater degree of tissue mobilisation, a more thorough rejuvenation of the eyebrow/forehead complex and increasing the precision of excess skin removal [24].
The technique by Fomon in 1939 is an adaptation of the technique by Passot, by also undermining the forehead skin off the underlying frontalis muscle, next to the elliptical skin removal just cranial of the eyebrow with or without ablation of the corrugator muscles allows for a smoother forehead [24].
In the 1950s, the understanding was that long-lasting results could only be achieved by modification of the frontalis muscle. In earlier techniques, the frontal branch of the facial nerve was transected to increase longevity, causing profound side effects [24].
In the modern coronal browlift by Viñas in 1965, a long incision from ear to ear is made, down to the periosteum where the forehead skin is completely undermined in the subgaleal plane, allowing easy dissection of the entire forehead and superior orbital regions where the temporal fusion lines and arcus maginalis are released, exposing the entire frontalis muscle and the insertions of the corrugator muscles. After scoring or resection of part of these muscles, the overlying skin can be redraped and fixated to the frontalis muscles; and after the excess cranial skin is removed, the incision can be closed [24, 26].
The approach by Regnault in 1972 dissected the subgaleal layer of the forehead to the eyebrows and the upper margin of the crow’s feet with galeal relaxing incisions for improved traction. In addition, a subcutaneous face-lift dissection was performed to preserve the neurovascular bridge in the temporal area [24, 27].
Kaye modified the Vinas procedure in 1977 by elevating the forehead flap deep to the galea and resecting segments of the corrugator supercilia muscles as well as a strip of frontalis and fascia. This method preserved the facial nerve and avoided the accompanying side effects [24, 28].
Pitanguy’s blocking technique (1970s) consists of the following: (1) blocking the facial flaps with stiches, so there are no alterations in anatomical positions after the procedure; (2) an open approach with wide exposure of the forehead flap; and (3) weakening of the muscles by making incisions in the aponeurosis. Although being common practice, this technique gave many side effects such as a sensation of tightness in the forehead, too highly positioned eyebrows, pain, bruising and swelling and numbness located at the incision [24].
In 1994, the first endoscopic browlift approach was described by Vásconez [11,12,13, 15, 29,30,31,32,33,34,35,36,37,38,39]. Due to the advantages (less scaring, less numbness posterior to the scar and less alopecia), the technique is relatively popular. The frequency of the endoscopic lift has recently decreased in practice, despite the relatively high satisfaction rate (70%) [40]. This is most likely due to high instrumental costs, operation time and the requirement of an operating theatre, which makes the procedure impossible to be performed on an outpatient basis. Both endoscopic and open browlift procedures describe decreased forehead sensation after surgery [41].
Indications for brow lifting
The most important indications for brow lifting according to Matarasso and Terino [8] are as follows: eyebrow ptosis, forehead rhytids, frown muscle imbalance, upper eyelid aesthetics, lateral temporal laxity (temporal hooding) and an abnormal (angry/sad) expression.
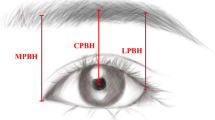
According to Westmore, who described the ideal eyebrows for women, the eyebrow needs to begin superiorly to the lateral nasal ala and forms a gentle arch laterally, peaking at the lateral limbus above the orbital rim, descending to end on a line drawn from the lateral nasal ala through the lateral canthus where the lateral and medial aspect of the eyebrow should be at the same height, although this might differ in women with a different facial configuration [1, 2, 42]. The anatomical position of the eyebrows in men is on or just above the superior orbital rim, and they are less positioned in an arch with less pretarsal skin in comparison to women [5]. There is a range of surgical and conservative procedures to ease symptoms associated with brow ptosis. A brow lift has the possibility to elevate the eyebrow between 0 and 7 mm [10, 12]. This is depicted in Fig. 1.
The paralysed eyebrow
The golden standard in the treatment of the paralysed eyebrow should be dynamic reanimation, but this is not possible for all patients. Especially for patients with a short life span, several comorbidities, elderly or other contraindications for dynamic reconstructions, static corrections could be a good alternative. A static correction could improve resting symmetry and function [43]. There should be paid further awareness to corneal exposure and lagophthalmos [44, 45].
Techniques used mostly in facial paralysis patients include all options described above, with or without fine-tuning procedures such as chemodenervation using Botulinum toxin to inhibit muscle contraction in synkinesis patients or contralateral chemodenervation of the frontalis muscle or corrugator complex [44, 45]. The direct browlift is mostly used in patients afflicted with facial palsy, since these patients often require substantial brow elevation and would be more likely to accept the scar [46]. However, advancements are being made in facial paralysis patients with endoscopic procedures [47].
Non-surgical methods
The most common way to treat brow-ptosis is the surgical approach, but there are also some non-surgical techniques [8]. The benefits of the non-surgical methods are that the treating physician needs less experience and a correction is easier done compared to surgery [8, 9]. The downside is that the results are almost always temporary [8, 9].
One of the treatments could be an injection with Botulinum toxin A. A botulinum toxin A (BTX-A) injection in the glabellar and crow’s feet area will affect the brow depressors (orbital orbicularis oculi, procerus, corrugators and depressor supercilii) and this will usually lead to a lateral brow lift. The effect will vanish in three to six months [8]. The effect on the central brow is just 1 mm and the effect on the lateral brow is 4.8 mm on average [8]. There could be seen some side effects accompanying BTX-A injections among others erythema and oedema, muscle weakness, pain and asymmetry [8]. BTX-A has also been used in other browlift procedures and no long-term difference was noted between patients who had received it versus those who did not [42].
Besides the BTX-A injections, there is also the method that uses soft tissue fillers [8]. Fillers are often used when BTX-A fails to elevate the eyebrow enough [8]. Besides the eyebrow lift, fillers also could enhance volume and contour of the eyebrows [8]. The base for the fillers is most often hyaluronic acid. The fillers with high stiffness and high viscosity could lead to a long-lasting effect on the brow lift, especially if they are implanted pre-periosteal [8, 9]. Overcorrection of the eyebrow could occur, and this will look like a very high-profile eyebrow or it could lead to oedema [8]. Due to the fact that fillers are foreign bodies, there could be granulomas and/or migration of the filler. Besides that, there is also a higher chance of infection, biofilm reaction, necrosis of the surrounding skin and the most important complication is blindness. The blindness will occur from retrograde injection into the ocular arterial system [49]. This is the reason why patients with one functioning eye are a contraindication for this procedure.
Surgical methods
Current techniques
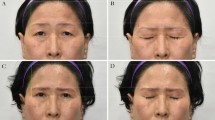
Browlifts are an evident component of the (facial) plastic surgery practice. The most common approaches are relatively clear and could be done by resecting excess skin or suspending the frontalis muscles. An overview is presented in Table 1 and Fig. 2.
Endoscopic browlift
The endoscopic approach utilises multiple (three to six) minor incisions and allows elevation of the eyebrow without the removal of excess skin and this results also in a high degree of browlift (approximately 10 mm), but there is still a lot of variation. In the procedure, the temporal line is released to fully mobilise the brow and forehead. It is paramount to avoid injury to the temporal branch of the facial nerve, which is done by staying immediately superficial to the deep temporal fascia (DTF) in the dissection anterior to the tragus in the temple region; another landmark is the sentinel vein, along the lateral margin of the forehead [3]. Also, the supraorbital and the supratrochlear nerves need to be avoided to protect scalp and brow sensation. Furthermore, to fully mobilise the brow, the arcus marginalis should be completely released [3]. The outcomes are mostly comparable to the coronal browlift [50]. Benefits are that every aspect of the eyebrow could be raised, revolving around the used incision sites. Some of the detrimental effects are obscuring of vision, sightly cosmesis and tarsorrhaphy, which could be avoided by using Botulinum toxin A injections [51]. Other adverse effects include the use of general anaesthetics, high cost of instruments and longer operation time [3].
Mid-forehead browlift
The mid-forehead indirect browlift incision is made in an existing deep rhytid and dissects superficially to the frontalis and preorbital muscles to the level of the supraorbital rim with a suspension of the inferior skin flap to the periost of the superior incision margin to lift the brow providing a more cosmetically pleasing scare although it may heal unpredictable and is not recommended in younger patients with a high chance of supratrochlear and supraorbital nerve paraesthesia [3].
Transblepharoplasty browlift
The hidden scar is the main asset of the transblepharoplasty technique. The scar is hidden in the traditional blepharoplasty incision, which is optimal in patients where a concurrent upper blepharoplasty is performed. This technique has a relatively minor browlift elevation effect (2-3 mm), could be performed under local anaesthesia, and due to supraorbital and supratrochlear nerve dissection, forehead paraesthesia could occur [3]. Paul et al. [25] presented an altered variant of the transblepharoplasty forehead lift where the corrugator muscle is transected and is subperiosteally advanced to the temporal scalp behind the hairline where another incision is made and the frontalis is suspended using a periosteal elevator to allow for more elevation of the forehead altogether than the transblepharoplasty browlift alone.
Direct browlift
The direct brow lift is performed under local anaesthesia and the skin along the superior margin of the eyebrow is excised. This technique is preferred for patients with sufficient brow hairs. The benefit is that the brow could be readjusted exactly without alteration to hair or rhytid lines. Due to the fact that only the skin is dissected, the main problem is the durability which is less than in periosteal suspension techniques; besides that, a grand visible scar remains along the upper margin of the eyebrow, and also paraesthesia and numbness are common practice (27.5–60%) [3, 52].
(Pre)trichial browlift
The (pre)trichial approach is performed under general anaesthesia and the skin is directly dissected anterior to or localised at the anterior hairline. This could be used to lower the frontal hairline to compress the forehead. The dissection is tunnelled under the subgaleal or subcutaneous plan to the supraorbital rim, located at the position where the forehead skin flap is draped back over the initial incision line lifting the eyebrow. This approach leaves a very visible scar, so it is often considerable to wear the hair in a fashion to cover the scar. [5].
Coronal browlift
The gold standard is the coronal browlift technique. There is an ear-to-ear curvilinear incision giving complete exposure where a myotomy or myectomy of corrugator, procerus, depressor supercilii and frontalis muscles can be performed to address brow ptosis and forehead rhytids. The significant and often occurring disadvantages are paraesthesia, scar formation and alopecia. [5, 7, 11].
Other techniques
Since it is impossible to give a totally complete depiction of all (often individual) types of browlift, this article is limited to the aforementioned techniques. Of those techniques, two techniques are specifically used in particular occasions:
Lateral temporal subcutaneous browlift
In this type of browlift that is particularly used in lateral brow ptosis, the incisions are placed either in or at the hair-bearing scalp (approximately 3.5 cm lateral to the midline); an elliptical excision of excess skin is performed according to the preferred correction of the brow. This is followed by blunt dissection of the underlying frontalis muscle to the upper edge of the brow and the wound is closed in layers. This technique is mostly effective in the improvement of lateral brow ptosis and provides acceptable scars with no notation of neural complications [48, 53].
Power browlift
Especially useful in patients with facial-paralysis-associated brow ptosis, this technique is performed in an outpatient setting through a 2 cm scalp incision on the affected side, with dissection carrying down through the subcutaneous tissue where a subperiosteal pocket is created. There a titanium miniplate is placed and through three 2 mm stab incisions evenly spaced within the hair-bearing eyebrow, two silk ties are placed and adjusted to the titanium plate, creating a “U” shape, adequately correcting the brow height. The significant advantage of this technique is that it is easy to perform under local anaesthesia with no risk of visible superciliary scar or postoperative forehead hypesthesia [54].
Complications of browlift techniques
Complications of any type of browlift are uncommon. Most patients will only experience some swelling and ecchymosis [4]. Literature about postoperative complications in brow surgery is sparse. However, a systematic review by Byun et al. [55] compared eighty-two studies using all-open and endoscopic browlift procedures and their associations with a variety of complications. Unacceptable scarring was found in 3.6% for endoscopic procedures and 2.1% for open procedures. Paraesthesia was found in 5.4% for open and 3.6% for endoscopic techniques. Other frequently seen browlift complications are asymmetry (0–9%), alopecia (3.0–8.5%), motor branch injury (0.0–6.4%) and skin necrosis (1.8% only after open browlift). The endoscopic procedure reports paraesthesia/dysesthesia (6.2%), asymmetry (3.6%), alopecia (3.0%), lagophthalmos (2.7%) and repeat surgery (2.4%) [55]. Comparisons between studies should be made with care, due to limitations adherent to case series. True complication rates need to be evaluated among various brow-lifting techniques [55].
Recurrence
Recurrences are often seen in several browlift procedures, with a ptosis recurrence or repeat surgery ranging from 0.3% in open browlifts versus 2.4% in endoscopic browlifts [56].
Conclusion
The eyebrow is a complex anatomical structure of the human face and has communicative and aesthetic elements that all contribute to a person’s individual appearance. Ptosis of the eyebrow is a common condition, especially among the elderly. Low eyebrow position results in unfavourable functional and aesthetic characteristics and often requires correction. No specific type of browlift has been shown to be superior to another technique, since there is a wide variation in anatomy and preferences between patients, requiring an individual approach for each specific patient.
References
Ellenbogen R (1983) Transcoronal eyebrow lift with concomitant upper blepharoplasty. Plast Reconstr Surg 71(4):490–499
Ellenbogen R (1980) Medial brow lift. Ann Plast Surg 5(2):151–152
Lee TS, Wang L, Han R, Mourad M, Ducic Y (2017) Options in repositioning the asymmetric brow from paralysis and trauma. Facial Plast Surg : FPS 33(6):627–638
Finsterer J (2003) Ptosis: causes, presentation, and management. Aesthet Plast Surg 27(3):193–204
Sundine MJ, Connell BF (2018) The open browlift. Facial Plast Surg: FPS 34(2):128–138
Connell BF, Marten TJ (1991) The male foreheadplasty. Recognizing and treating aging in the upper face. Clin Plast Surg 18(4):653–87
Flowers RS, Ceydeli A (2008) The open coronal approach to forehead rejuvenation. Clin Plast Surg. 35(3):331–51; discussion 29
Matarasso A, Terino EO (1994) Forehead-brow rhytidoplasty: reassessing the goals. Plast Reconstr Surg. 93(7):1378–89; discussion 90-1
Matarasso A (1995) Endoscopically assisted forehead-brow rhytidoplasty: theory and practice. Aesthetic Plast Surg 19(2):141–147
Troilius C (1999) A comparison between subgaleal and subperiosteal brow lifts. Plast Reconstr Surg. 104(4):1079–90; discussion 91-2
Dayan SH, Perkins SW, Vartanian AJ, Wiesman IM (2001) The forehead lift: endoscopic versus coronal approaches. Aesthetic Plast Surg 25(1):35–39
McKinney P, Sweis I (2001) An accurate technique for fixation in endoscopic brow lift: a 5-year follow-up. Plast Reconstr Surg. 108(6):1808–10; discussion 11-4
Jones BM, Grover R (2004) Endoscopic brow lift: a personal review of 538 patients and comparison of fixation techniques. Plast Reconstr Surg. 113(4):1242–50; discussion 51-2
Sidle DM, Loos BM, Ramirez AL, Kabaker SS, Maas CS (2005) Use of BioGlue surgical adhesive for brow fixation in endoscopic browplasty. Arch Facial Plast Surg 7(6):393–397
Papadopulos NA, Eder M, Weigand C, Biemer E, Kovacs L (2012) A review of 13 years of experience with endoscopic forehead-lift. Arch Facial Plast Surg 14(5):336–341
Rafaty FM, Goode RL, Fee WE Jr (1975) The brow-lift operation. Arch Otolaryngol (Chicago, Ill : 1960). 101(8):467–8
Johnson CM Jr, Anderson JR, Katz RB (1979) The brow-lift 1978. Arch Otolaryngol (Chicago, Ill : 1960). 105(3):124–6
Lewis JR Jr (1983) A method of direct eyebrow lift. Ann Plast Surg 10(2):115–119
Ueda K, Harii K, Yamada A (1994) Long-term follow-up study of browlift for treatment of facial paralysis. Ann Plast Surg 32(2):166–170
Rafaty FM, Goode RL, Abramson NR (1978) The brow-lift operation in a man. Arch Otolaryngol (Chicago, Ill : 1960). 104(2):69–71
Angelos PC, Stallworth CL, Wang TD (2011) Forehead lifting: state of the art. Facial Plast Surg : FPS 27(1):50–57
Knize DM (1996) Limited-incision forehead lift for eyebrow elevation to enhance upper blepharoplasty. Plast Reconstr Surg 97(7):1334–1342
Knize DM (2001) Limited incision forehead lift for eyebrow elevation to enhance upper blepharoplasty. Plast Reconstr Surg 108(2):564–567
Paul MD (2001) The evolution of the brow lift in aesthetic plastic surgery. Plast Reconstr Surg 108(5):1409–1424
Paul MD (1996) Subperiosteal transblepharoplasty forehead lift. Aesthetic Plast Surg 20(2):129–134
Vinas JC, Caviglia C, Cortinas JL (1976) Forehead rhytidoplasty and brow lifting. Plast Reconstr Surg 57(4):445–454
Regnault P (1972) Complete face and forehead lifting, with double traction on “crow’s-feet.” Plast Reconstr Surg 49(2):123–129
Kaye BL (1977) The forehead lift: a useful adjunct to face lift and blepharoplasty. Plast Reconstr Surg 60(2):161–171
Vasconez LO, Core GB, Gamboa-Bobadilla M, Guzman G, Askren C, Yamamoto Y (1994) Endoscopic techniques in coronal brow lifting. Plast Reconstr Surg 94(6):788–793
de la Fuente A, Santamaría AB (2002) Endoscopic forehead lift: is it effective? Aesthetic Surg J 22(2):113–120
Iblher N, Manegold S, Porzelius C, Stark GB (2012) Morphometric long-term evaluation and comparison of brow position and shape after endoscopic forehead lift and transpalpebral browpexy. Plast Reconstr Surg 130(6):830e-e840
Graf RM, Tolazzi ARD, Mansur AEC, Teixeira V (2008) Endoscopic periosteal brow lift: evaluation and follow-up of eyebrow height. Plast Reconstr Surg 121(2):609–616
Graf R (2012) Discussion: morphometric long-term evaluation and comparison of brow position and shape after endoscopic forehead lift and transpalpebral browpexy. Plast Reconstr Surg 130(6):841e-e842
Javidnia H, Sykes J (2013) Endoscopic brow lifts: have they replaced coronal lifts? Facial Plast Surg Clin North Am 21(2):191–199
Jones BM, Lo SJ (2013) The impact of endoscopic brow lift on eyebrow morphology, aesthetics, and longevity: objective and subjective measurements over a 5-year period. Plast Reconstr Surg 132(2):226e-e238
Behmand RA, Guyuron B (2006) Endoscopic forehead rejuvenation: II. Long-term results. Plast Reconstr Surg. 117(4):1137–43; discussion 44
Guyuron B (2006) Endoscopic forehead rejuvenation: I Limitations, flaws, and rewards. Plast Reconstr Surg. 117(4):1121–33; discussion 34-6
Ramirez OM (1997) Why I prefer the endoscopic forehead lift. Plast Reconstr Surg. 100(4):1033–9; discussion 43-6
Stanek JJ, Berry MG (2014) Endoscopic-assisted brow lift: revisions and complications in 810 consecutive cases. J Plast Reconstr Aesthet Surg : JPRAS. 67(7):998–1000
Chiu ES, Baker DC (2003) Endoscopic brow lift: a retrospective review of 628 consecutive cases over 5 years. Plast Reconstr Surg. 112(2):628–33; discussion 34-5
Guillot JM, Rousso DE, Replogle W (2011) Forehead and scalp sensation after brow-lift: a comparison between open and endoscopic techniques. Arch Facial Plast Surg 13(2):109–116
Baker SB, Dayan JH, Crane A, Kim S (2007) The influence of brow shape on the perception of facial form and brow aesthetics. Plast Reconstr Surg 119(7):2240–2247
Lafer MP, O TM (2018) Management of Long-Standing Flaccid Facial Palsy: Static Approaches to the Brow, Midface, and Lower Lip. Otolaryngol Clin North Am. 51(6):1141–50
Cooper L, Lui M, Nduka C (2017) Botulinum toxin treatment for facial palsy: a systematic review. J Plast Reconstr Aesthet Surg: JPRAS 70(6):833–841
Moody FP, Losken A, Bostwick J 3rd, Trinei FA, Eaves FF 3rd (2001) Endoscopic frontal branch neurectomy, corrugator myectomy, and brow lift for forehead asymmetry after facial nerve palsy. Plast Reconstr Surg 108(1):218–223
Karimi N, Kashkouli MB, Sianati H, Khademi B (2020) Techniques of eyebrow lifting: a narrative review. J Ophthalmic Vis Res 15(2):218–235
Holtmann L, Büchsenschütz K, Eckstein A, Schlüter A, Lang S, Mattheis S (2017) Endoscopic Browlift via Endotine Forehead Device in Patients with Facial Palsy. Laryngorhinootologie 96(10):691–697
Savetsky IL, Matarasso A (2020) Lateral temporal subcutaneous brow lift: clinical experience and systematic review of the literature. Plast Reconstr Surg Global open. 8(4):e2764
Chiang YZ, Pierone G, Al-Niaimi F (2017) Dermal fillers: pathophysiology, prevention and treatment of complications. J Eur Acad Dermatol Venereol : JEADV 31(3):405–413
Graham DW, Heller J, Kirkjian TJ, Schaub TS, Rohrich RJ (2011) Brow lift in facial rejuvenation: a systematic literature review of open versus endoscopic techniques. Plast Reconstr Surg 128(4):335e-e341
Ellis MF, Daniell M (2001) An evaluation of the safety and efficacy of botulinum toxin type A (BOTOX) when used to produce a protective ptosis. Clin Exp Ophthalmol 29(6):394–399
Booth AJ, Murray A, Tyers AG (2004) The direct brow lift: efficacy, complications, and patient satisfaction. Br J Ophthalmol 88(5):688–691
Miller TA, Rudkin G, Honig M, Elahi M, Adams J (2000) Lateral subcutaneous brow lift and interbrow muscle resection: clinical experience and anatomic studies. Plast Reconstr Surg. 105(3):1120–7; discussion 8
Hohman MH, Silver AL, Henstrom DK, Cheney ML, Hadlock TA. The “power” brow lift: efficient correction of the paralyzed brow. Int Schol Research Notices. 2013.
Byun S, Mukovozov I, Farrokhyar F, Thoma A (2013) Complications of browlift techniques: a systematic review. Aesthet Surg J 33(2):189–200
Ergün SS, Sahinoğlu K (2003) Eyebrow transplantation. Ann Plast Surg 51(6):584–586
Funding
None.
Author information
Authors and Affiliations
Contributions
Conception and design of the study: FJ, SP. Drafting and revision manuscript: FJ, ES, SP, KW, NH, SM, KI. Final approval: FJ, ES, SP, KW, NH, SM, KI.
Corresponding author
Ethics declarations
Ethical approval
This is a narrative review. No ethical approval is required.
Informed consent
No individual patients were included in this study.
Conflict of interest
Frank W. de Jongh, Elijah E. Sanches, Sjaak Pouwels, Laurens B. R. Kooiman, Kim M. E. Wehrens, Niels van Heerbeek, Stan J. Monstrey, Liang T. Tan and Koen J. A. O. Ingels declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
de Jongh, F.W., Sanches, E.E., Pouwels, S. et al. An overview of surgical techniques and non-surgical treatments in lifting the eyebrow including current treatments available. Eur J Plast Surg 46, 1–8 (2023). https://doi.org/10.1007/s00238-021-01911-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00238-021-01911-4