Abstract
Purpose
Selective androgen receptor modulators (SARMs) have demonstrated agonist activity on the androgen receptor in various tissues, stimulating muscle mass growth and improving bone reconstruction. Despite being in clinical trials, none has been approved by the Food and Drug Administration (FDA) or European Medicines Agency for pharmacotherapy. Still, SARMs are very popular as performance-enhancing drugs. The FDA has issued warnings about the health risks associated with SARMs, but the long-term exposure and possible adverse events still need to be fully understood. This review aims to evaluate the adverse events associated with using SARMs by humans.
Methods
PubMed database was searched from September 16, 2022, to October 2, 2023. In total, 20 records were included in the final review. Data from preclinical and clinical studies supported the review.
Results
Since 2020, 20 reports of adverse events, most described as drug-induced liver injury associated with the use of SARM agonists, have been published. The main symptoms mentioned were cholestatic or hepatocellular liver injury and jaundice. Limited data are related to the dosages and purity of SARM supplements.
Conclusion
Promoting SARMs as an anabolic agent in combination with other performance-enhancing drugs poses a risk to users not only due to doping controls but also to health safety. The lack of quality control of consumed supplements makes it very difficult to assess the direct impact of SARMs on the liver and their potential hepatotoxic effects. Therefore, more detailed analyses are needed to determine the safety of using SARMs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Selective androgen receptor modulators (SARMs) are a group of compounds with therapeutic potential. SARMs act as ligands by diffusing into the cell and binding to the androgen receptor in the cytoplasm. This creates a receptor–ligand complex that translocate to the nucleus where it binds to DNA and acts as a transcriptional regulator of androgen genes response. Unlike natural ligands of this receptor, SARMs have a tissue-selective effect, which gives them a significant advantage over other steroidal anabolic substances [1]. Currently, only SARMs antagonists, such as flutamide, nilutamide, bicalutamide, and enzalutamide, have been introduced to pharmacotherapy as nonsteroidal antiandrogen drugs for the treatment of prostate cancer. However, SARM agonists, which have shown the potential to stimulate muscle growth (anabolic effect) and improve bone reconstruction, are undergoing clinical trials and have not yet been approved by the Food and Drug Administration (FDA) or European Medicine Agency (EMA) for pharmacotherapy [2].
For the first time, a method for detecting SARM agonists (arylpropionamide derivatives) was proposed in spiked urine specimens using liquid chromatography/electrospray ionization tandem mass spectrometry with monitoring and simultaneous precursor ion scanning. The primary reason for developing this assay was to detect the potential misuse of SARMs as a doping agent by elite athletes. Since 2008, SARMs have been included on the World Anti-Doping Agency (WADA) Prohibited List in the class of anabolic agents [3, 4]. Currently, SARMs are still recognized as doping agents and covered by the WADA Prohibited List in the group S1 Anabolic Agents (Other anabolic agents in subsection 2) [5]. In 2009, SARMs were first detected in products available on the market [6, 7]. Despite this, SARM agonists are still available for sale. Some products are labeled as dietary supplements, while others do not have a specific classification or contain statements such as “Not for human consumption” or “Research use only.” SARMs available for sale online are offered in the form of tablets/capsules, liquid, or powder [8,9,10].
Only a few studies have reported on the prevalence of SARM use in recreational exercisers. In a study conducted in Greece, among 170 adolescent gym users surveyed using a questionnaire, 9% reported using products containing anabolic–androgenic steroids, prohormones, SARMs (including LGD-4033 and MK-2866), and aromatase inhibitors [11], [12].
A more precise estimate of the prevalence of SARMs use comes from a cross-sectional study conducted in the Netherlands. In this study, a completed online questionnaire was used to collect data from a group of young male gym users (n = 2269; aged 24 ± 6 years). The study found that 2.7% of all participants reported using SARMs [13]. The most commonly used SARMs were ligandrol (LGD-4033), enobosarm (MK-2866), also known as ostarine, and testolone (RAD-140). The majority of recreational SARMs users are males aged 18–29 years, who consume the substances individually or in stacks. Furthermore, these users have reported various adverse events (AEs) after 3 months of use, including but not limited to mood swings, decreased testicular size, and acne [14].
In 2012, data from WADA adverse analytical findings (AAF) reported only five AAF related to SARMs. However, the number of AAF increased in the following years, reaching its peak in 2019 with ostarine—74, ligandrol—62, RAD-140—4, and single cases of SARM S-23 and andarine. The latest available data from 2020 reported a decrease in these results. However, it should be emphasized that the total number of samples collected was 46.1% lower in 2020 compared to 2019 [5]. SARMs have led to annual increases in positive test results through detection methods in different biological samples, such as hair, nails, urine, and blood [15]. The presence of SARMs in biological samples may be unintentional and unconscious and result from contamination of dietary supplements with microdoses [16].
Recent cases of doping in Olympic and professional sports have involved ostarine and S-23 in athletics and basketball, respectively, as well as LGD-4033 in canoeing. However, the actual prevalence of SARM use is likely to be higher among fitness enthusiasts [17]. Several cases of SARMs detection in athletes have been reported previously [18, 19]. The popularity of SARMs among elite and competitive athletes is fueled by aggressive online marketing that includes many false and unauthorized health claims attributed to SARMs. One frequently used false argument in online advertising is that SARMs are a safe alternative to AAS and do not cause adverse effects. While SARMs do not cause the typical androgenic side effects specific to AAS, the short-term and long-term effects of AAS use and related adverse effects are recognized and expected. In the case of SARMs, the long-term exposure and possible adverse effects are not fully known, which confirms that no molecules from the SARM agonist group have been approved for pharmacotherapy [13, 20, 21].
The FDA has issued a warning letter about the health risks associated with the use of body-building products containing SARMs, informing about the potential increase in the risk of heart attack or stroke and other life-threatening adverse reactions such as liver damage [22, 23]. A large number of notifications about SARM detection have been registered in the database CFSAN Adverse Event Reporting System (CAERS) as potential AEs (The CFSAN 2022).
Warnings about the presence of unauthorized ingredients from SARMs such as ligandrol, ostarine, and testolone in food supplements sold online have been reported on the RASFF panel, mainly from Poland [24].
Most of the AEs associated with the intake of SARMs are drug-induced liver injuries (DILI). DILI can be divided into two groups: intrinsic and idiosyncratic. The intrinsic type includes drugs that produce DILI in a dose-related manner with a predictable capacity, and the rate of occurrence is high when the drug is given in high doses, such as acetaminophen (paracetamol) or selected plant raw materials containing pyrrolizidine alkaloids [25].
Most DILI cases are classified as idiosyncratic, where the drug reaction is unpredictable and not related to the known pharmacological action of the drug, and the rate of occurrence is low. This category includes drugs such as isoniazid, selected antibiotics, statins, and selected ingredients in dietary supplements. An immune response is important in the pathogenesis of idiosyncratic DILI. The threshold of serum alanine aminotransferase (ALT), alkaline phosphatase (ALP), aspartate aminotransferase (AST), and total bilirubin (TB) is used to assess severity of DILI. DILI can be classified as hepatocellular (predominantly an elevation of ALT), cholestatic (mostly elevated ALP), and mixed type of liver damage when the elevation of ALT and ALP is between them. DILI severity is evaluated according to Hy’s Law. Hy’s law assessments are used by the FDA in drug development, including serum activity of ALT of at least three times the upper limit of normal (ULN), and ALT > 3 ULN and TB > 2 ULN without a significant ALP (< 2 × ULN) increase. The “New Hy’s Law” proposed by the Spanish DILI Registry includes a specific factor signed as “nR” and calculated based on dependencies, where (ALT or AST whichever higher/ULN)/(ALP/ULN), and if the result is > 5 and TB > 2 ULN, then nR is considered positive, regardless of the ALP value. To identify and classify DILI cases, the values of aminotransferases, ALP, and TB are used, and serum ALT has greater liver tissue specificity than serum AST [26]. Information resources about DILI and specific drugs that induce them are included in the LiverTox database, but there is no information about SARM agonists [27].
Recently, there have been many reports of liver damage caused by SARMs, as well as comprehensive reviews of the probable causative mechanisms [28, 29]. Our review also takes into account changes in carbohydrate and lipid metabolism, including studies on animal models. Moreover, we summarized the toxicophores in more common SARMs on the black market. Emerging work indicates a problem with the potential risk posed by the use of SARMs and a comprehensive analysis is necessary to better understand the causes of toxic effects.
The aim of this review is to evaluate liver injury cases associated with the use of SARM agonists by humans and to assess their safety according to the most current available knowledge.
Methodology
To collect data, we searched PubMed for articles published from September 16, 2022, to October 2, 2023, using the search strategy: “((selective androgenic receptor modulators) OR (SARM)) AND ((safety) OR (health risk) OR (adverse event) OR (adverse reaction) OR (side effect) OR (hepatotoxicity) OR (liver injury) OR (drug‐induced liver injury)).”
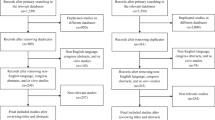
The first queries provided 341 records, which were screened to exclude 191 records due to their review or systematic review status. Only full-text articles were assessed for eligibility, and in the next stage, all records were screened by title and abstract. We excluded 150 records that were not related to the aim of the review and basic queries, and we added 4 records from other sources.
In total, 20 records were included in the final review. The methodology and data workflow is demonstrated in Fig. 1.
Results
Liver injury has been reported in humans using SARMs, mainly through spontaneous reports. For example, a case of severe DILI with cholestatic hepatitis and perisinusoidal fibrosis was reported in a subject who declared an intake of ligandrol at a dose of 10 mg/day [30]. However, clinical trials have determined that the safe daily doses of ligandrol are 0.1, 0.3, and 1 mg for 21 days. This suggests that the subject was using a much higher dose than what was reported in the clinical trial. Nonetheless, this AE report has some limitations, such as no performed analytical test to detect ligandrol in the suspected product, or no performed toxicological test of blood (or hairs) sample to confirm (or exclude) a share of ligandrol. Details for all collected AEs associated with the use of SARMs agonists are shown in Table 1.
In most cases, increased liver enzymes were identified. Elevated alanine aminotransferase (ALT), aspartate aminotransferase (AST), and lactate dehydrogenase (not measured in the reported cases) are considered to be indicative of cell damage. Alkaline phosphatase (ALP) and total bilirubin (TB) were also measured in reported cases. Generally, hepatocellular damage is indicated by increased aminotransferase activity, while higher ALP and GTTP activity indicates cholestatic liver injury.
Among the reported cases of oral use of SARMs, most often cholestatic liver damage was diagnosed. SARMs are typically used orally and the mechanism of liver damage may be similar to 17α-alkylated AAS [28] and directly contribute to a highly characteristic form of acute cholestasis, ranging from very mild to severe. Patients diagnosed with cholestatic liver injury had characteristic symptoms including nausea, pruritus, fatigue, jaundice, and dark urine and those were the main reasons for being admitted to the hospital.
These disorders occurred regardless of the SARM used—they accompanied the intake of ostarine, RAD-140, and LGD-4033 individually [31], [34] as well as in the combination of these three SARMs [46]. No additional supplementation was reported in any of these cases. Among the remaining reported cases of cholestatic liver injury, patients used combinations of several SARMs [39] as well as in combination with other substances, such as finasteride and zopiclone [35], an unnamed pre-workout supplement [42], and a mix of acetaminophen, caffeine, and aspirin [44].
Other results related to liver damage concerned perisinusoidal fibrosis, where the patient only declared taking LDG-4033 [30]. The remaining results concerned hepatocellular liver injury due to the intake of LGD-4033 and S-23 [45] as well as liver cytolysis due to the combination of ostarine and the metabolism modulator GW-1516 [36].
Only in a few cases was the dose of the substances taken precisely determined, but it should be noted that no laboratory analysis was performed to confirm the purity and content of the substances. Only one study found the content of LGD-4033 and RAD-140 [31], while the second one analyzed biological samples (blood, urine, and hair) obtained from the patient [36].
Occurrences unrelated to liver injury included acute myocarditis. This was the first reported case of a SARM that may have a causal relationship with acute myocarditis. However, the patient had a medical history of type 1 diabetes which was being controlled with insulin injections and was also undergoing opioid-assisted treatment with sublingual buprenorphine due to a history of drug abuse. The case is ambiguous and it is unclear whether acute myocarditis was caused by the SARM or by the additional medications administered to the patient. The report suggests that there may be a potential interaction between SARMs and insulin and/or opioid medications [40]. Arayangkool et al. described the case of a patient who also suffered from bile cast nephropathy because of SARM-associated drug-induced liver injury [46].
Discussion
To address the potential inconsistencies in spontaneous AE reports, the authors summarized the duration of exposure, dosage, safety assessment, and pharmacokinetic parameters of selected SARM agonists covered in clinical trials. This information is accessed in Supplementary section. It should be noted that preclinical studies on the andarine (S-4) compound, which is also available for sale online, were suspended and did not advance to phase I of clinical trials [2].
In the clinical trials conducted with SARM agonists, some participants experienced elevations in AST/ALT/TB levels. However, these trials used controlled and precise doses of the investigational product. In the case reports of DILI, the exact dose of SARMs used by the subjects was not specified in most cases. In some cases where the dose was mentioned, it was found to be several times higher than the dose used in clinical trials, but this information was based only on the label of the product and not confirmed through analytical testing.
It is important to note that the selected chemical structures of SARMs contain various toxicophores, which are well recognized in medicinal chemistry as potential causes of toxicity in drugs (Fig. 2). For example, ligandrol contains a nitrile substituent (Ar–CN) and an aziridine moiety, while testolone contains two Ar–CN groups and an aromatic azo group (Ar–N = N–Ar). Andarine contains an aromatic nitro substituent (Ar–NO2) and a potentially unstable substructure of (Ar–NHCO–C(OH)(CH3)–CH2–O–Ar), which is also found in ostarine, along with two Ar–CN groups. This substructure, which is similar to the main toxicophore of paracetamol (acetaminophen), can be unstable and form reactive and hepatotoxic N-acetyl-p-benzo imine derivatives during oxidative metabolism in the liver. This is especially concerning in cases where the substance is administered at an unknown or uncontrolled dosage or when multiple substances are taken in a single dose. The presence of selected toxicophores, such as Ar–NO2 in andarine, may be associated with higher toxicity of this compound [50,51,52,53].
Previous studies have shown that out of 44 dietary supplements sold as SARMs, 39% of them contained unapproved substances other than SARMs, such as ibutamoren (a growth hormone secretagogue), cardarine (GW501516, a peroxisome proliferator-activated receptor-δ agonist), and SR9009 (Rev-Erba [a circadian clock protein] agonist). Mass spectrometry analysis of these dietary supplements revealed that only 52% of them contained SARMs, indicating that many of these products were mislabeled [8,9,10, 15].
The CAERS database provides interesting observations, including many reports of potential AEs for specific keywords/queries related to SARMs (Table 2). We searched the CAERS database using the following keywords: “SARM,” “andarine,” “S-4,” “ostarin(e),” “MK-2866,” “ligandrol,” “LGD-4033,” “testolone,” “RAD-140,” and “YK-11.” In summary, the reports not only included cases of liver injury but also blindness or a visual impairment, cerebrovascular accidents, paresthesia, abnormal hormone levels, testicular disorders, gynecomastia, increased blood prolactin, sexual dysfunction, altered mood, and a single fatal case of cardiac death [54].
The widespread availability of SARMS can be demonstrated by looking at the additional sources such as the RASFF (summary of findings are included in Supplementary section), at the Polish market (Allegro.pl) as an example, and in the NIH Label Database. All data from the analysis of Polish market and NIH Label Database is presented in Table 3. However, all the information which we analyzed are based only on the description included on the label of the product provided by the producer.
The WADA provides more precise data on antidoping testing figures, which detect all prohibited substances through analytical tests (Table 4) [55].
At first, the heterogeneity of SARMs’ chemical structures posed a challenge to the development of precise detection methods. However, in subsequent years, there has been intensive development of new testing assays [6, 7].
Sobolevsky et al. provided the first human excretion results on ligandrol and confirmed several hydroxylated metabolites, including monohydroxylated and bishydroxylated, as well as hydroxylated and ring-cleaved metabolites [56].
Some potential mechanisms underlying liver damage from the use of SARMs as performance-enhancing substances have not been well studied [57]. In reported cases, increased liver enzymes indicating cell damage as well as cardiac muscle damage were reported. The recently published report on the profibrotic and cardiotoxic effects of ostarine may indirectly indicate the direction of further research [58]. One possible explanation is that SARMs significantly increase carbohydrate metabolism, particularly gluconeogenesis, resulting in hyperglycemia and insulin resistance [59]. The rate of gluconeogenesis in the liver is largely regulated by the activity of FOXO1 and PGC-1α [60], although their exact relationship in the context of SARM induction remains unclear.
Interestingly, PGC-1α is also involved in fatty acid metabolism, specifically increasing beta-oxidation in the liver and playing a crucial role in metabolic adaptation during starvation in this tissue [61]. The overstimulation of both pathways due to SARM-induced anabolism can lead to oxidative stress and insulin resistance in hepatocytes [62], which may in turn increase proinflammatory mechanisms such as interleukin secretion [63] and peroxidated molecule production, further contributing to the inflammatory cascade [64]. Ultimately, these processes may activate apoptotic cascades [65].
The effect of SARMs on lipid metabolism is an area that requires further investigation, as the available literature on the anabolic effect of SARMs poorly reports their effects on nontarget tissues and the liver. However, changes in lipid metabolism have been reported in animal models, including in the liver [66, 67], plasma [68, 69], and adipose tissue [69, 70]. Table 5 summarizes the reported changes in lipid metabolism in animal models. Excess body fat can have adverse effects on metabolic changes due to the adipokines it produces. Ostarine has been shown to reduce the secretion of leptin and adiponectin from white adipocytes [71], while low levels of leptin can intensify de novo lipogenesis in the liver and promote lipid accumulation in muscles, affecting insulin production in the pancreas and contribute to insulin resistance [72,73,74]. Similarly, low levels of adiponectin can promote negative effects such as oxidative stress and mitochondrial dysfunction in the liver [75, 76]. The results of Min et al. using another SARM, S-42, reported no change in the level of adiponectin [67]. In addition, the results show the downregulation of SREBP-1c factors as well as FAS, which are crucial elements in lipogenesis de novo. This is the opposite of the results obtained using SAA [77].
Some studies have found changes in lipoproteins, triglycerides, and cholesterol in clinical trials and animal models. Although inconsistent results were noted for triglycerides and low-density lipoprotein in human subjects studies, the lowering of high-density lipoprotein (HDL) confirmed in clinical trials deserves attention [80,81,82]. Other studies have also reported a reduction in apolipoprotein AI, a main protein in HDL [83,84,85]. Although these changes may be significant for the cardiovascular system, long-term reduced production of HDL may be related to liver dysfunction and limited regenerative processes of this organ [86, 87]. It is important to note that the results returned to baseline levels after the end of treatment but only concerned a relatively short period of administration (from 14 to 86 days). The longest administration time (113 days and 6 months) did not assess these parameters. The effect of long-term use of SARMs at high doses remains unclear. Summary of selected clinical trials demonstrated in supplementary data [88,89,90,91].
The use of SARMs can disrupt metabolic pathways and potentially impact liver metabolism. However, the varying effects observed in studies can be attributed to factors such as the type of SARM, dose, and physiological state of the subjects. Although animal studies may not be entirely reliable due to differences in metabolism, they can provide partial insights into the mechanisms underlying DILI. Given the limited use of SARMs in human studies, animal models with humanized livers, chimeric mice with humanized cytochrome P450 enzymes, or cell models are crucial in identifying the mechanisms involved in DILI.
Conclusions
Our review provides a comprehensive overview of the harmful effects of SARMs on the liver. However, current knowledge of the toxicity mechanisms of SARMs is insufficient. Uncontrolled dosing and/or combining several SARM compounds in one product may lead to AEs related to liver damage and affect lipid metabolism disorders. Withdrawal of the substance often results in liver recovery, but the actual number of SARM users remains unclear. Analytical tests have confirmed many discrepancies in both quantity and quality analysis, indicating a very low quality of SARM products available on the market. Labels often do not provide accurate information for consumers, and cases of counterfeit and fake manipulation among ingredients and declared doses have been confirmed.
Assessing liver damage, severity, and potential hepatotoxicity of SARM compounds, as well as their causality, can be helpful in the diagnosis and implementation of effective treatment in clinical practice. Promoting SARMs as a safe alternative to other anabolic compounds is significantly dangerous and poses a risk to public health. Increasing consumer awareness of the risks of SARM supplementation is crucial in preventing harmful effects.
Data Availability
The data that support the findings of this study are available on request.
References
Narayanan R, Coss CC, Dalton JT (2018) Development of selective androgen receptor modulators (SARMs). Mol Cell Endocrinol 465:134–142. https://doi.org/10.1016/j.mce.2017.06.013
Fonseca GWPD, Dworatzek E, Ebner N, Von Haehling S (2020) Selective androgen receptor modulators (SARMs) as pharmacological treatment for muscle wasting in ongoing clinical trials. Expert Opin Investig Drugs 29(8):881–891. https://doi.org/10.1080/13543784.2020.1777275
Thevis M, Schänzer W (2008) Mass spectrometry of selective androgen receptor modulators. J Mass Spectrom 43(7):865–876. https://doi.org/10.1002/jms.1438
Thevis M, Kamber M, Schänzer W (2006) Screening for metabolically stable aryl-propionamide-derived selective androgen receptor modulators for doping control purposes. Rapid Commun Mass Spectrom 20(5):870–876. https://doi.org/10.1002/rcm.2389
WADA World Anti-Doping Agency Antidoping Testing Figures 2011 - 2020. https://www.wada-ama.org/en/resources/anti-doping-stats. 2020. Accessed on 26 April 2023
Thevis M, Beuck S, Thomas A, Kortner B, Kohler M, Rodchenkov G, Schänzer W (2009) Doping control analysis of emerging drugs in human plasma - identification of GW501516, S-107, JTV-519, and S-40503. Rapid Commun Mass Spectrom 23(8):1139–1146. https://doi.org/10.1002/rcm.3987
Thevis M, Geyer H, Kamber M, Schänzer W (2009) Detection of the arylpropionamide-derived selective androgen receptor modulator (SARM) S-4 (Andarine) in a black-market product. Drug Test Anal 1(8):387–392. https://doi.org/10.1002/dta.91
Chakrabarty R, Grainger J, Goebel C, Brooker L, George A (2021) “For research use only”: a comprehensive analysis of SARMs and related IPEDs purchased on local Australian websites between 2017 and 2018. Perform Enhanc Heal 9(3–4):100201. https://doi.org/10.1016/j.peh.2021.100201
Leaney AE, Beck P, Biddle S, Brown P, Grace PB, Hudson SC, Mawson DH (2021) Analysis of supplements available to UK consumers purporting to contain selective androgen receptor modulators. Drug Test Anal 13(1):122–127. https://doi.org/10.1002/dta.2908
Van Wagoner RM, Eichner A, Bhasin S, Deuster PA, Eichner D (2017) Chemical composition and labeling of substances marketed as selective androgen receptor modulators and sold via the Internet. JAMA 318(20):2004–2010. https://doi.org/10.1001/jama.2017.17069
Tsarouhas K, Kioukia-Fougia N, Papalexis P, Tsatsakis A, Kouretas D, Bacopoulou F, Tsitsimpikou C (2018) Use of nutritional supplements contaminated with banned doping substances by recreational adolescent athletes in Athens. Greece Food Chem Toxicol 115:447–450. https://doi.org/10.1016/j.fct.2018.03.043
Vasilev V, Boyadjiev N. Selective androgen receptor modulators (SARMs) in sports: a review. Athens J. Sport. 2021;8(3):215–30. https://doi.org/10.30958/ajspo.8-3-4
Hilkens L, Cruyff M, Woertman L, Benjamins J, Evers C (2021) Social media, body image and resistance training: creating the perfect ‘me’ with dietary supplements, anabolic steroids and SARM’s. Sports Med Open 7(1):81. https://doi.org/10.1186/s40798-021-00371-1
Efimenko IV, Valancy D, Dubin JM, Ramasamy R (2022) Adverse effects and potential benefits among selective androgen receptor modulators users: a cross-sectional survey. Int J Impot Res 34(8):757–761. https://doi.org/10.1038/s41443-021-00465-0
Kintz P (2022) The forensic response after an adverse analytical finding (doping) involving a selective androgen receptor modulator (SARM) in human athlete. J Pharm Biomed Anal 207:114433. https://doi.org/10.1016/j.jpba.2021.114433
Wagener F, Guddat S, Görgens C, Angelis YS, Petrou M, Lagojda A, Kühne D, Thevis M (2022) Investigations into the elimination profiles and metabolite ratios of micro-dosed selective androgen receptor modulator LGD-4033 for doping control purposes. Anal Bioanal Chem 414(2):1151–1162. https://doi.org/10.1007/s00216-021-03740-7
Hahamyan HA, Vasireddi N, Voos JE, Calcei JG (2022) Social media’s impact on widespread SARMs abuse. Phys Sportsmed 20:1–3. https://doi.org/10.1080/00913847.2022.2078679
Cox HD, Eichner D (2017) Detection of LGD-4033 and its metabolites in athlete urine samples. Drug Test Anal 9(1):127–134. https://doi.org/10.1002/dta.1986
Earl M, Vouillamoz M, Kwiatkowska D, Turek-Lepa E, Pokrywka A, Saugy M, Baume N, Gmeiner G (2014) The UEFA Euro 2012 anti-doping programme - scientific review. Biol Sport 31(2):85–93. https://doi.org/10.5604/20831862.1096037
Efimenko IV, Chertman W, Masterson TA, Dubin JM, Ramasamy R (2021) Analysis of the growing public interest in selective androgen receptor modulators. Andrologia 53(11):e14238. https://doi.org/10.1111/and.14238
Machek SB, Cardaci TD, Wilburn DT, Willoughby DS (2020) Considerations, possible contraindications, and potential mechanisms for deleterious effect in recreational and athletic use of selective androgen receptor modulators (SARMs) in lieu of anabolic androgenic steroids: a narrative review. Steroids 164:108753. https://doi.org/10.1016/j.steroids.2020.108753
US FDA United States Food & Drug Administration. WARNING LETTER Umbrella [Internet]. 2023. Available from: https://www.fda.gov/inspections-compliance-enforcement-and-criminal-investigations/warning-letters/umbrella-612037-05182021. Accessed on 26 April 2023
US FDA United States Food & Drug Administration. FDA In Brief: FDA warns against using SARMs in body-building products. 2023. https://www.fda.gov/news-events/fda-brief/fda-brief-fda-warns-against-using-sarms-body-building-products. Accessed on 26 April 2023
European Commission (EC). RASFF. 2022. https://webgate.ec.europa.eu/rasff-window/screen/search. Accessed on 16 September 2022.
Danan G, Teschke R (2018) Drug-induced liver injury: why is the Roussel Uclaf Causality Assessment Method (RUCAM) still used 25 years after its launch? Drug Saf 41(8):735–743. https://doi.org/10.1007/s40264-018-0654-2
Robles-Diaz M, Lucena MI, Kaplowitz N, Stephens C, Medina-Cáliz I, González-Jimenez A, Ulzurrun E, Gonzalez AF, Fernandez MC, Romero-Gómez M, Jimenez-Perez M, Bruguera M, Prieto M, Bessone F, Hernandez N, Arrese M, Andrade RJ; Spanish DILI Registry; SLatinDILI Network; Safer and Faster Evidence-based Translation Consortium. Use of Hy’s law and a new composite algorithm to predict acute liver failure in patients with drug-induced liver injury. Gastroenterology. 2014;147(1):109–118.e5.
Teschke R, Danan G (2021) The LiverTox paradox-gaps between promised data and reality check. Diagnostics (Basel) 11(10):1754. https://doi.org/10.3390/diagnostics11101754
Mohideen H, Hussain H, Dahiya DS, Wehbe H. Selective androgen receptor modulators: an emerging liver toxin. J Clin Transl Hepatol. 2023;11(1):188–196. https://doi.org/10.14218/JCTH.2022.00207.
Vignali JD, Pak KC, Beverley HR, DeLuca JP, Downs JW, Kress AT, Sadowski BW, Selig DJ (2023) Systematic review of safety of selective androgen receptor modulators in healthy adults: implications for recreational users. J Xenobiot 13(2):218–236. https://doi.org/10.3390/jox13020017
Barbara M, Dhingra S, Mindikoglu AL. Ligandrol (LGD-4033)-induced liver injury. ACG Case Rep J. 2020;7(6):e00370. https://doi.org/10.14309/crj.0000000000000370
Flores JE, Chitturi S, Walker S (2020) Drug-induced liver injury by selective androgenic receptor modulators. Hepatol Commun 4(3):450–452. https://doi.org/10.1002/hep4.1456
Barbara M, Dhingra S, Mindikoglu AL. Drug-induced liver injury associated with Alpha Bolic (RAD-140) and Alpha Elite (RAD-140 and LGD-4033). ACG Case Rep J. 2020;7(6):e00409. https://doi.org/10.14309/crj.0000000000000409
Baliss M, Kline K, Merwat S (2020) S2718 Harmful gains: drug-induced liver injury from selective androgen receptor modulators. Am J Gastroenterol 115(1):S1421–S1421. https://doi.org/10.14309/01.ajg.0000712920.97943.a8
Koller T, Vrbova P, Meciarova I, Molcan P, Smitka M, Adamcova Selcanova S, Skladany L. Liver injury associated with the use of selective androgen receptor modulators and post-cycle therapy: two case reports and literature review. World J Clin Cases. 2021;9(16):4062–4071. https://doi.org/10.12998/wjcc.v9.i16.4062.
Bedi H, Hammond C, Sanders D, Yang HM, Yoshida EM. Drug-induced liver injury from enobosarm (ostarine), a selective androgen receptor modulator. ACG Case Rep J. 2021;8(1):e00518. https://doi.org/10.14309/crj.0000000000000518.
Kintz P, Gheddar L, Paradis C, Chinellato M, Ameline A, Raul JS, Oliva-Labadie M (2021) Peroxisome proliferator-activated receptor delta agonist (PPAR-δ) and selective androgen receptor modulator (SARM) abuse: clinical, analytical and biological data in a case involving a poisonous combination of GW1516 (Cardarine) and MK2866 (Ostarine). Toxics 9(10):251. https://doi.org/10.3390/toxics9100251
Lam H, Wong S. S2730 At what cost: drug-induced liver injury secondary to selective androgen receptor modulator. Am J Gastroenterol. 2021;116(1):S1142–S1142. https://doi.org/10.14309/01.ajg.0000784452.64316.30
Akhtar N, Locke D, Stine J. S2851 Harm by SARM: a case of drug-induced liver injury in an amateur bodybuilder. Am. J. Gastroenterol. 2021;116(1):S1184-S1184 https://doi.org/10.14309/01.ajg.0000784936.08024.c4
Lee BK, Park BB, Bower RJ. Selective androgen receptor modulator-induced liver injury in active duty male. Mil Med. 2022;usac039. https://doi.org/10.1093/milmed/usac039.
Padappayil RP, Chandini Arjun A, Vivar Acosta J, Ghali W, Mughal MS (2022) Acute myocarditis from the use of selective androgen receptor modulator (SARM) RAD-140 (Testolone). Cureus 14(1):e21663. https://doi.org/10.7759/cureus.21663
Weinblatt D, Roy S. Drug-induced liver injury secondary to enobosarm: a selective androgen receptor modulator. J Med Cases. 2022;13(5):244–8. https://doi.org/10.14740/jmc3937
Khan S, Fackler J, Gilani A, Murphy S, Polintan L (2022) Selective androgen receptor modulator induced hepatotoxicity. Cureus 14(2):e22239. https://doi.org/10.7759/cureus.22239
Sotorník R, Suissa R, Ardilouze JL (2022) Could overt diabetes be triggered by abuse of selective androgen receptor modulators and growth hormone secretagogues? A case report and review of the literature. Clin Diabetes 40(3):373–379. https://doi.org/10.2337/cd21-0044
Leung K, Yaramada P, Goyal P, Cai CX, Thung I, Hammami MB. RAD-140 drug-induced liver injury. Ochsner J. 2022;22(4):361–365. https://doi.org/10.31486/toj.22.0005
Malave B (2023) Metabolic and hormonal dysfunction in asymptomatic patient using selective androgen receptor modulators: a case report. Bull Natl Res Cent 47:11. https://doi.org/10.1186/s42269-023-00989-z
Arayangkool C, Gozun M, Tanariyakul M, Techasatian W, Leesutipornchai T, Nishimura Y. Bile cast nephropathy because of acute liver injury associated with selective androgen receptor modulators. ACG Case Rep J. 2023;10(7):e01105. https://doi.org/10.14309/crj.0000000000001105.
Ladna M, Taylor K, Bhat A, Dideban B (2023) Idiosyncratic drug-induced liver injury related to use of novel selective androgen receptor modulator RAD140 (Testalone): a case report. J Med Case Rep 17(1):134. https://doi.org/10.1186/s13256-023-03847-8
Mohamed WT, Jahagirdar V, Fatima I, Ahmed MK, Jaber F, Wang K, Hassan A, Ewing E, Clarkston W, Likhitsup A (2023) Selective androgen receptor modulators (SARMs)-induced liver injury: a case report and review of literature. Cureus 15(2):e35094. https://doi.org/10.7759/cureus.35094
Cardaci TD, Machek SB, Wilburn DT, Heileson JL, Harris DR, Cintineo HP, Willoughby DS (2022) LGD-4033 and MK-677 use impacts body composition, circulating biomarkers, and skeletal muscle androgenic hormone and receptor content: a case report. Exp Physiol 107(12):1467–1476. https://doi.org/10.1113/EP090741
Dang NL, Matlock MK, Hughes TB, Swamidass SJ (2020) The metabolic rainbow: deep learning phase I metabolism in five colors. J Chem Inf Model 60(3):1146–1164. https://doi.org/10.1021/acs.jcim.9b00836
Fleming FF, Yao L, Ravikumar PC, Funk L, Shook BC (2010) Nitrile-containing pharmaceuticals: efficacious roles of the nitrile pharmacophore. J Med Chem 53(22):7902–7917. https://doi.org/10.1021/jm100762r
Meanwell NA (2016) Improving drug design: an update on recent applications of efficiency metrics, strategies for replacing problematic elements, and compounds in nontraditional drug space. Chem Res Toxicol 29(4):564–616. https://doi.org/10.1021/acs.chemrestox.6b00043
Williams DP, Park BK (2003) Idiosyncratic toxicity: the role of toxicophores and bioactivation. Drug Discov Today 8(22):1044–1050. https://doi.org/10.1016/s1359-6446(03)02888-5
The CFSAN Adverse Event Reporting System (CAERS). 2022. https://www.fda.gov/food/compliance-enforcement-food/cfsan-adverse-event-reporting-system-caers. Accessed on 16 September 2022
WADA World Anti-Doping Agency Prohibited List 2023. 2022. https://www.wada-ama.org/en/resources/world-anti-doping-program/2023-prohibited-list. Accessed on 26 April 2023
Sobolevsky T, Dikunets M, Dudko G, Rodchenkov G. Metabolism study of the selective androgen receptor modulator LGD-4033. In 33rd Cologne Workshop on Dope Analysis, Manfred-Donike Institute, Cologne, Germany (pp. 75–79). 2015;4033
Christiansen AR, Lipshultz LI, Hotaling JM, Pastuszak AW. Selective androgen receptor modulators: the future of androgen therapy? Transl Androl Urol. 2020;9(Suppl 2):S135-S148. https://doi.org/10.21037/tau.2019.11.02.
Leciejewska N, Pruszyńska-Oszmałek E, Nogowski L, Sassek M, Strowski MZ, Kołodziejski PA (2023) Sex-specific cytotoxicity of ostarine in cardiomyocytes. Mol Cell Endocrinol 577:112037. https://doi.org/10.1016/j.mce.2023.112037
Kuo T, McQueen A, Chen TC, Wang JC (2015) Regulation of glucose homeostasis by glucocorticoids. Adv Exp Med Biol 872:99–126. https://doi.org/10.1007/978-1-4939-2895-8_5
Zhang C, Zhong T, Li Y, Li X, Yuan X, Liu L, Wu W, Wu J, Wu Y, Liang R, Xie X, Kang C, Liu Y, Lai Z, Xiao J, Tang Z, Jin R, Wang Y, Xiao Y, Zhang J, Li J, Liu Q, Sun Z, Zhong J (2021) The hepatic AMPK-TET1-SIRT1 axis regulates glucose homeostasis. Elife 10:e70672. https://doi.org/10.7554/eLife.70672
Nakamura MT, Yudell BE, Loor JJ (2014) Regulation of energy metabolism by long-chain fatty acids. Prog Lipid Res 53:124–144. https://doi.org/10.1016/j.plipres.2013.12.001
Malik SA, Acharya JD, Mehendale NK, Kamat SS, Ghaskadbi SS (2019) Pterostilbene reverses palmitic acid mediated insulin resistance in HepG2 cells by reducing oxidative stress and triglyceride accumulation. Free Radic Res 53(7):815–827. https://doi.org/10.1080/10715762.2019.1635252
Brenner C, Galluzzi L, Kepp O, Kroemer G (2013) Decoding cell death signals in liver inflammation. J Hepatol 59(3):583–594. https://doi.org/10.1016/j.jhep.2013.03.033
Tsikas D (2017) Assessment of lipid peroxidation by measuring malondialdehyde (MDA) and relatives in biological samples: analytical and biological challenges. Anal Biochem 524:13–30. https://doi.org/10.1016/j.ab.2016.10.021
Luedde T, Kaplowitz N, Schwabe RF (2014) Cell death and cell death responses in liver disease: mechanisms and clinical relevance. Gastroenterology 147(4):765-783.e4. https://doi.org/10.1053/j.gastro.2014.07.018
Komrakova M, Büchler G, Böker KO, Lehmann W, Schilling AF, Roch PJ, Taudien S, Hoffmann DB, Sehmisch S (2022) A combined treatment with selective androgen and estrogen receptor modulators prevents bone loss in orchiectomized rats. J Endocrinol Invest 45(12):2299–2311. https://doi.org/10.1007/s40618-022-01865-9
Min L, Yanase T, Tanaka T, Fan W, Nomura M, Kawate H, Okabe T, Takayanagi R, Nawata H (2009) A novel synthetic androgen receptor ligand, S42, works as a selective androgen receptor modulator and possesses metabolic effects with little impact on the prostate. Endocrinology 150(12):5606–5616
Morimoto M, Yamaoka M, Hara T (2020) A selective androgen receptor modulator SARM-2f activates androgen receptor, increases lean body mass, and suppresses blood lipid levels in cynomolgus monkeys. Pharmacol Res Perspect 8(1):e00563. https://doi.org/10.1002/prp2.563
Schmidt A, Kimmel DB, Bai C, Scafonas A, Rutledge S, Vogel RL, McElwee-Witmer S, Chen F, Nantermet PV, Kasparcova V, Leu CT, Zhang HZ, Duggan ME, Gentile MA, Hodor P, Pennypacker B, Masarachia P, Opas EE, Adamski SA, Cusick TE, Wang J, Mitchell HJ, Kim Y, Prueksaritanont T, Perkins JJ, Meissner RS, Hartman GD, Freedman LP, Harada S, Ray WJ (2010) Discovery of the selective androgen receptor modulator MK-0773 using a rational development strategy based on differential transcriptional requirements for androgenic anabolism versus reproductive physiology. J Biol Chem 285(22):17054–17064. https://doi.org/10.1074/jbc.M109.099002
Kearbey JD, Gao W, Narayanan R, Fisher SJ, Wu D, Miller DD, Dalton JT (2007) Selective androgen receptor modulator (SARM) treatment prevents bone loss and reduces body fat in ovariectomized rats. Pharm Res 24(2):328–335. https://doi.org/10.1007/s11095-006-9152-9
Leciejewska N, Pruszynska-Oszmalek E, Bien J, Nogowski L, Kolodziejski PA. Effect of ostarine (enobosarm/GTX024), a selective androgen receptor modulator, on adipocyte metabolism in Wistar rats. J Physiol Pharmacol. 2019;70(4). https://doi.org/10.26402/jpp.2019.4.04.
Jiménez-Cortegana C, García-Galey A, Tami M, Del Pino P, Carmona I, López S, Alba G, Sánchez-Margalet V (2021) Role of leptin in non-alcoholic fatty liver disease. Biomedicines 9(7):762. https://doi.org/10.3390/biomedicines9070762
Martínez-Uña M, López-Mancheño Y, Diéguez C, Fernández-Rojo MA, Novelle MG (2020) Unraveling the role of leptin in liver function and its relationship with liver diseases. Int J Mol Sci 21(24):9368. https://doi.org/10.3390/ijms21249368
Park HK, Ahima RS (2015) Physiology of leptin: energy homeostasis, neuroendocrine function and metabolism. Metabolism 64(1):24–34. https://doi.org/10.1016/j.metabol.2014.08.004
Gamberi T, Magherini F, Modesti A, Fiaschi T (2018) Adiponectin signaling pathways in liver diseases. Biomedicines 6(2):52. https://doi.org/10.3390/biomedicines6020052
Neumeier M, Weigert J, Schäffler A, Weiss TS, Schmidl C, Büttner R, Bollheimer C, Aslanidis C, Schölmerich J, Buechler C (2006) Aldehyde oxidase 1 is highly abundant in hepatic steatosis and is downregulated by adiponectin and fenofibric acid in hepatocytes in vitro. Biochem Biophys Res Commun 350(3):731–735. https://doi.org/10.1016/j.bbrc.2006.09.101
Balgoma D, Zelleroth S, Grönbladh A, Hallberg M, Pettersson C, Hedeland M (2020) Anabolic androgenic steroids exert a selective remodeling of the plasma lipidome that mirrors the decrease of the de novo lipogenesis in the liver. Metabolomics 16(1):1–13. https://doi.org/10.1007/s11306-019-1632-0
Komrakova M, Schilling AF, Lehmann W, Vasilev V, Georgieva K, Gerginska F, Boyadjiev N, Delchev S (2023) Selective androgen receptor modulators combined with treadmill exercise have no bone benefit in healthy adult rats. Pharmaceuticals (Basel) 16(9):1249. https://doi.org/10.3390/ph16091249
Kearbey JD, Gao W, Fisher SJ, Wu D, Miller DD, Dalton JT (2009) Effects of selective androgen receptor modulator (SARM) treatment in osteopenic female rats. Pharm Res 26(11):2471–2477. https://doi.org/10.1007/s11095-009-9962-7
Basaria S, Collins L, Dillon EL, Orwoll K, Storer TW, Miciek R, Ulloor J, Zhang A, Eder R, Zientek H, Gordon G, Kazmi S, Sheffield-Moore M, Bhasin S (2013) The safety, pharmacokinetics, and effects of LGD-4033, a novel nonsteroidal oral, selective androgen receptor modulator, in healthy young men. J Gerontol A Biol Sci Med Sci 68(1):87–95. https://doi.org/10.1093/gerona/gls078
Bhattacharya I, Tarabar S, Liang Y, Pradhan V, Owens J, Oemar B (2016) Safety, pharmacokinetic, and pharmacodynamic evaluation after single and multiple ascending doses of a novel selective androgen receptor modulator in healthy subjects. Clin Ther 38(6):1401–1416. https://doi.org/10.1016/j.clinthera.2016.03.025
Dalton JT, Barnette KG, Bohl CE, Hancock ML, Rodriguez D, Dodson ST, Morton RA, Steiner MS (2011) The selective androgen receptor modulator GTx-024 (enobosarm) improves lean body mass and physical function in healthy elderly men and postmenopausal women: results of a double-blind, placebo-controlled phase II trial. J Cachexia Sarcopenia Muscle 2(3):153–161. https://doi.org/10.1007/s13539-011-0034-6
Clark RV, Walker AC, Andrews S, Turnbull P, Wald JA, Magee MH (2017) Safety, pharmacokinetics and pharmacological effects of the selective androgen receptor modulator, GSK2881078, in healthy men and postmenopausal women. Br J Clin Pharmacol 83(10):2179–2194. https://doi.org/10.1111/bcp.13316
Neil D, Clark RV, Magee M, Billiard J, Chan A, Xue Z, Russell A (2018) GSK2881078, a SARM, produces dose-dependent increases in lean mass in healthy older men and women. J Clin Endocrinol Metab 103(9):3215–3224. https://doi.org/10.1210/jc.2017-02644
Pencina KM, Burnett AL, Storer TW, Guo W, Li Z, Kibel AS, Huang G, Blouin M, Berry DL, Basaria S, Bhasin S (2021) A selective androgen receptor modulator (OPK-88004) in prostate cancer survivors: a randomized trial. J Clin Endocrinol Metab 106(8):2171–2186. https://doi.org/10.1210/clinem/dgab361
Ding BS, Liu CH, Sun Y, Chen Y, Swendeman SL, Jung B, Chavez D, Cao Z, Christoffersen C, Nielsen LB, Schwab SR, Rafii S, Hla T (2016) HDL activation of endothelial sphingosine-1-phosphate receptor-1 (S1P1) promotes regeneration and suppresses fibrosis in the liver. JCI Insight 1(21):e87058. https://doi.org/10.1172/jci.insight.87058
Manka P, Olliges V, Bechmann LP, Schlattjan M, Jochum C, Treckmann JW, Saner FH, Gerken G, Syn WK, Canbay A (2014) Low levels of blood lipids are associated with etiology and lethal outcome in acute liver failure. Plos One 9(7):e102351. https://doi.org/10.1371/journal.pone.0102351
Coss CC, Jones A, Dalton JT (2016) Pharmacokinetic drug interactions of the selective androgen receptor modulator GTx-024(Enobosarm) with itraconazole, rifampin, probenecid, celecoxib and rosuvastatin. Invest New Drugs 34(4):458–467. https://doi.org/10.1007/s10637-016-0353-8
Dobs AS, Boccia RV, Croot CC, Gabrail NY, Dalton JT, Hancock ML, Johnston MA, Steiner MS (2013) Effects of enobosarm on muscle wasting and physical function in patients with cancer: a double-blind, randomised controlled phase 2 trial. Lancet Oncol 14(4):335–345. https://doi.org/10.1016/S1470-2045(13)70055-X
LoRusso P, Hamilton E, Ma C, Vidula N, Bagley RG, Troy S, Annett M, Yu Z, Conlan MG, Weise A (2022) A first-in-human phase 1 study of a novel selective androgen receptor modulator (SARM), RAD140, in ER+/HER2− metastatic breast cancer. Clin Breast Cancer 22(1):67–77. https://doi.org/10.1016/j.clbc.2021.08.003
Papanicolaou DA, Ather SN, Zhu H, Zhou Y, Lutkiewicz J, Scott BB, Chandler J (2013) A phase IIA randomized, placebo-controlled clinical trial to study the efficacy and safety of the selective androgen receptor modulator (SARM), MK-0773 in female participants with sarcopenia. J Nutr Health Aging 17(6):533–543. https://doi.org/10.1007/s12603-013-0335-x
Funding
The study was supported by the National Science Centre, project number 2019/35/N/NZ7/00738 (NL).
Author information
Authors and Affiliations
Contributions
NL, KJ, VMGR, JMN and AP designed the concept and prepared the manuscript. VMGR and JMN helped in literature mining and data collection. Modifications and improvements in this manuscript were done by AP and BM. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Consent for publication
All authors consent to publish this manuscript.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Leciejewska, N., Jędrejko, K., Gómez-Renaud, V.M. et al. Selective androgen receptor modulator use and related adverse events including drug-induced liver injury: Analysis of suspected cases. Eur J Clin Pharmacol 80, 185–202 (2024). https://doi.org/10.1007/s00228-023-03592-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-023-03592-3