Abstract
Background
RAD140 (Testalone) is a novel selective androgen receptor modulator with very limited data currently available on adverse effects related to this compound. The first-in-human phase 1 trial was recently published and did report a significant proportion of elevated aspartate aminotransferase, alanine transaminase, and total bilirubin among the test subjects. RAD140 may be associated with an idiosyncratic drug-induced liver injury. It is easily purchased online as a workout supplement. Given its ease of use from being an oral formulation, and not requiring a physician’s prescription, its use among the young male population will likely rise. Clinicians should ask about the use of RAD140, and other workout supplements, in young men presenting with acute liver injury.
Case presentation
We present the case of a 26-year-old Caucasian male without any significant past medical history who presented with nausea, vomiting, severe right upper quadrant abdominal pain, and jaundice from acute liver injury. Extensive inpatient workup did not reveal a definite cause for his liver injury other than the use of a novel selective androgen receptor modulator called RAD140 (Testalone). He was treated with supportive care and discharged after short hospitalization. He was instructed to stop RAD140, which he reported compliance with, and on 2-month follow-up his liver function panel had normalized without recurrence of any symptoms.
Conclusion
Novel selective androgen receptor modulators such as RAD140 may be associated with idiosyncratic drug-induced liver injury. Workup of new liver injury in young and middle-aged males should involve asking about use of these novel compounds, for if missed and use continues, it can likely lead to fulminant liver failure or decompensated liver cirrhosis.
Similar content being viewed by others
Introduction
Young men are using oral androgen agonists more often, and there is a constant influx of these unregulated agents, which can be easily purchased over the internet. The adverse effects of these substances are not well researched. Unregulated, these substances may contain active compounds and contaminants ultimately associated with adverse effects, including hepatotoxicity. The use of these agents will likely increase given their ease of use compared with traditional testosterone therapy, which is intramuscular and available by prescription only. It is important for the clinician to be aware of these substances and the potential adverse effects, such as acute liver injury, to ensure the appropriate diagnosis can be made and the patient can be instructed to stop the use of these substances to prevent further liver injury, and ultimately fulminant liver failure. This case also highlights the value of thorough history taking, which can be difficult to perform in the modern age of productivity-based medical practice.
Case presentation
A 26-year-old Caucasian male without any past medical history presented to emergency department with chief complaint of yellow skin and eyes, nausea, nonbloody vomiting, and severe right upper quadrant abdominal pain. These symptoms first started 9 days prior and had been getting progressively worse. The abdominal pain was intermittent and associated with dark, tea-colored urine and constipation. He denied use of any acetaminophen recently, alcohol use, illicit drug use, or personal/family history of hereditary hemochromatosis, Wilson’s disease, or celiac disease. He did report use of a new workout supplement called RAD140 (Testalone). He had previously been using a powdered version of the compound but switched to a liquid version approximately 2 months ago. Physical exam was significant for jaundice with scleral icterus and epigastric, as well as right upper quadrant abdominal, tenderness to palpation without rigidity, rebound, or guarding.
Laboratory work revealed transaminitis with aspartate transaminase (AST) of 51 IU/L, alanine transaminase (ALT) of 243 IU/L, and hyperbilirubinemia with total bilirubin of 4.9 mg/dL. Lactate dehydrogenase (LDH), alkaline phosphatase, and gamma-glutamyltransferase (GGT) were all within norms. Computed tomography (CT) of the abdomen and pelvis showed normal appearing liver and gallbladder. Right upper quadrant ultrasound was unremarkable, revealing a liver with homogeneous echotexture without focal parenchymal lesion, a common bile duct of 8 mm without biliary ductal dilatation, and a normal gallbladder without evidence of cholecystitis. Antismooth muscle, antimitochondrial, liver–kidney microsomal, antitissue transglutaminase, anti-endomysial, and gliadin immunoglobulin (Ig)G antibodies and antinuclear antibodies (ANA) were all negative. IgG, IgA, IgM, and ceruloplasmin all within normal limits. Tested negative for hepatitis A, B, and C. Acetaminophen level was undetectable. Hemochromatosis gene testing was negative. Research into RAD140 revealed that it was a novel selective androgen receptor modulator (SARM) called Testolone and has been associated with drug-induced liver injury (DILI) in case reports in the available literature. Due to extensive negative workup and discussion with hepatology colleagues, it was determined that the most likely cause of DILI was either RAD140 itself or another unknown but active compound or contaminant in the over-the-counter product. Treatment was supportive care via pain control, nausea control, and hydration. He was counseled to stop taking RAD140, which he was agreeable to.
He was hospitalized for a total of 4 days and discharged home. His symptoms of abdominal pain, nausea, and vomiting resolved during the hospitalization. Although the transaminitis improved while inpatient, the hyperbilirubinemia trended up. Per hepatology, this was attributed to being part of the typical course of DILI and he was safe to be discharged. Repeat outpatient laboratory work revealed normalization of AST, ALT, and total bilirubin 1 month after discharge. He followed up with hepatology in the clinic 2 months after discharge and reported cessation of RAD140 medication and was asymptomatic at that time without recurrence of abdominal pain, nausea, vomiting, or jaundice.
Discussion and conclusions
RAD140 was first discovered by Radius Health, Inc in 2010. It belongs to a group called selective androgen receptor modulators (SARMs), which are nonsteroidal, orally active molecules developed to bind androgen receptors strongly in targeted tissues (muscle and bone) and weakly in genital tissues, with the goal of treating sarcopenia and osteoporosis while minimizing worsening of prostate disease in men and virilization in women [1]. SARMs are widely available on the internet as nutritional supplements, despite not being approved for human consumption. One study of various SARM products found that only 23/44 (53%) of the products tested contained 1 or more SARM, 17 (39%) contained another unapproved drug, and 4 (9%) did not contain any active compound [2]. Only one case report from early 2020 documented DILI with RAD140/Testolone [3]. There is also a single case report documenting acute myocarditis associated with RAD140 [4].
The first in-human phase 1 clinical trial of RAD140 was published in January 2022 and included a total of 22 postmenopausal women with stage IV, ER+/HER2− breast cancer. The most common adverse effects were elevated AST (59.1%), ALT (45.5%), total bilirubin (27.3%), and hypophosphatemia (22.7%), as well as dehydration, vomiting, anorexia, and weight loss (27.3% each). The acceptable safety profile was at doses of 50–100 mg daily, with the 150 mg daily dose group having significantly more hyperbilirubinemia and hypophosphatemia. All these adverse events were reversible, and there were no treatment-related deaths or serious adverse events (AE) leading to study withdrawal [5].
Owing to frequent contamination and mislabeling of nutritional supplements, it is difficult to conclude whether this case of DILI was due to the active compound RAD140, or another active component or contaminant. The wide availability of these compounds to retail consumers should encourage physicians who encounter acute liver injury of undetermined etiology to inquire about the recreational use of these novel compounds. Individuals are at high risk of taking excessive doses or dosing too frequently since data on safe doses has only just recently been published [5]. The use of a liquid form of RAD140 via dropper, as was the case with our patient, likely made administration of an accurate dose more challenging, leading to unintentional toxic dosing of the compound.
Patients with acute liver injury require a thorough diagnostic workup to reveal the pathology. Etiologies such as autoimmune hepatitis, Wilson’s disease, alcoholic hepatitis, Tylenol toxicity, acute and chronic viral hepatitis, primary sclerosing cholangitis, and primary biliary cholangitis must be ruled out prior to making a diagnosis of idiosyncratic DILI. DILI not associated with Tylenol use is typically managed with supportive care, immediate cessation of the insulting compound, and referral to liver transplantation if the patient presents with fulminant acute liver failure or there is worsening of liver injury, despite cessation of the insulting compound. Our patient was managed with supportive care and had resolution of DILI after cessation of RAD140 use.
Availability of data and materials
Not applicable.
References
Miller CP, Shomali M, Lyttle CR, et al. Design, synthesis, and preclinical characterization of the selective androgen receptor modulator (SARM) RAD140. ACS Med Chem Lett. 2011;2(2):124–9. https://doi.org/10.1021/ml1002508.
Van Wagoner RM, Eichner A, Bhasin S, Deuster PA, Eichner D. Chemical composition and labeling of substances marketed as selective androgen receptor modulators and sold via the internet. JAMA. 2017;318(20):2004–10. https://doi.org/10.1001/jama.2017.17069.
Barbara M, Dhingra S, Mindikoglu AL. Drug-induced liver injury associated with alpha bolic (RAD-140) and alpha elite (RAD-140 and LGD-4033). ACG Case Rep J. 2020;7(6):e00409. https://doi.org/10.14309/crj.0000000000000409.
Padappayil RP, Chandini Arjun A, Vivar Acosta J, Ghali W, Mughal MS. Acute myocarditis from the use of selective androgen receptor modulator (SARM) RAD-140 (testolone). Cureus. 2022;14(1):e21663. https://doi.org/10.7759/cureus.21663.
LoRusso P, Hamilton E, Ma C, et al. A first-in-human phase 1 study of a novel selective androgen receptor modulator (SARM), RAD140, in ER+/HER2− metastatic breast cancer. Clin Breast Cancer. 2022;22(1):67–77. https://doi.org/10.1016/j.clbc.2021.08.003.
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
Case report was written chiefly by ML, with contributions and editing done by KT, AB, and BD. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
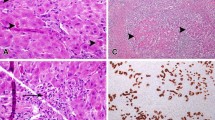
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The author declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ladna, M., Taylor, K., Bhat, A. et al. Idiosyncratic drug-induced liver injury related to use of novel selective androgen receptor modulator RAD140 (Testalone): a case report. J Med Case Reports 17, 134 (2023). https://doi.org/10.1186/s13256-023-03847-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13256-023-03847-8