Abstract
Objective
This study aimed to estimate the total healthcare costs associated with elderly chronic pain (CP) patients, define cost-related factors in this population, and examine cost evolution over two years.
Method
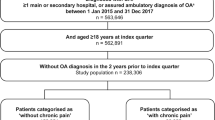
This is an ancillary study from the CP S.AGE subcohort, including non-institutionalized patients aged over 65 suffering from CP. 1190, 1108, 1042, and 950 patients were reviewed with available healthcare data at follow-up visits at 6, 12, 18, and 24 months, respectively. Healthcare components included medical and paramedical visits, medication prescription, and hospitalization.
Result
The mean total cost in the first semester was estimated at €2548 ± €8885 per patient. Hospitalization represented the largest cost component (50 %) followed by paramedical care (24 %), medications (21 %), and medical visits (5 %). Significant cost-associated factors were comorbidity (OR 1.49, 95 % CI 1.35–1.64), dependency in daily activities (OR 1.85, 95 % CI 1.39–2.47), probable depression (OR 1.71, 95 % CI 1.09–2.69), permanent pain (OR 1.48, 95 % CI 1.18–1.86), neuropathic pain (OR 1.94, 95 % CI 1.38–2.73), living alone (OR 1.45, 95 % CI 1.16–1.82), chronic back pain (OR 1.35, 95 % CI 1.07–1.71), and vertebral fracture/compression (OR 1.47, 95 % CI 1.08–2.01). Healthcare costs increased significantly by 48 % (p < 0.0001) during follow-up namely due to hospitalizations. Elevated costs were associated with a higher risk of future hospitalization (OR 1.95, CI 95 % 1.33–2.87).
Conclusion
Healthcare costs increased rapidly over time, largely due to hospitalization. Prevention strategies to limit hospitalizations in elderly appear to be the most useful in order to achieve cost savings in the future.
Similar content being viewed by others
References
Gaskin DJ, Richard P (2012) The economic costs of pain in the United States. J Pain 13(8):715–724
Andersson HI, Ejlertsson G, Leden I, Schersten B (1999) Impact of chronic pain on health care seeking, self care, and medication. Results from a population-based Swedish study. J Epidemiol Community Health 53(8):503–509
Dominick KL, Ahern FM, Gold CH, Heller DA (2004) Health-related quality of life and health service use among older adults with osteoarthritis. Arthritis Rheum 51(3):326–331
Lalonde L, Choiniere M, Martin E, Berbiche D, Perreault S, Lussier D (2014) Costs of moderate to severe chronic pain in primary care patients—a study of the ACCORD Program. J Pain Res 7:389–403
Gustavsson A, Bjorkman J, Ljungcrantz C, Rhodin A, Rivano-Fischer M, Sjolund KF, Mannheimer C (2012) Socio-economic burden of patients with a diagnosis related to chronic pain—register data of 840,000 Swedish patients. Eur J Pain 16(2):289–299
Raftery MN, Ryan P, Normand C, Murphy AW, de la Harpe D, McGuire BE (2012) The economic cost of chronic noncancer pain in Ireland: results from the PRIME study, part 2. J Pain 13(2):139–145
Depont F, Hunsche E, Abouelfath A, Diatta T, Addra I, Grelaud A, Lagnaoui R, Molimard M, Moore N (2010) Medical and non-medical direct costs of chronic low back pain in patients consulting primary care physicians in France. Fundam Clin Pharmacol 24(1):101–108
Pradalier A, Auray JP, El Hasnaoui A, Alzahouri K, Dartigues JF, Duru G, Henry P, Lanteri-Minet M, Lucas C, Chazot G, Gaudin AF (2004) Economic impact of migraine and other episodic headaches in France: data from the GRIM2000 study. Pharmacoeconomics 22(15):985–999
Kobelt G, Woronoff AS, Richard B, Peeters P, Sany J (2008) Disease status, costs and quality of life of patients with rheumatoid arthritis in France: the ECO-PR Study. Joint Bone Spine 75(4):408–415
Knight T, Schaefer C, Chandran A, Zlateva G, Winkelmann A, Perrot S (2013) Health-resource use and costs associated with fibromyalgia in France, Germany, and the United States. Clinicoecon Outcome Res 5:171–180
Bertin P, Rannou F, Grange L, Dachicourt JN, Bruel P, Emery C, Grandfils N, Ch T (2014) Annual cost of patients with osteoarthritis of the hip and knee in France. J Musculoskelet Pain 22(4):356–364
Becquemont L, Benattar-Zibi L, Bertin P, Berrut G, Corruble E, Danchin N, Delespierre T, Derumeaux G, Falissard B, Forette F, Hanon O, Pasquier F, Pinget M, Ourabah R, Piedvache C (2013) National observatory on the therapeutic management in ambulatory care patients aged 65 and over, with type 2 diabetes, chronic pain or atrial fibrillation The S.AGES cohort, design and baseline characteristics of the study population. Therapie 68(4):1–19
Bertin P, Becquemont L, Corruble E, Derumeaux G, Falissard B, Hanon O, Pinget M, Forette F (2013) The therapeutic management of chronic pain in ambulatory care patients aged 65 and over in France: the S.AGES Cohort. Baseline data. J Nutr Heal Aging 17(8):681–686
Bucher S, Bauduceau B, Benattar-Zibi L, Bertin P, Berrut G, Corruble E, Danchin N, Delespierre T, Derumeaux G, Doucet J, Falissard B, Forette F, Hanon O, Ourabah R, Pasquier F, Piedvache C, Pinget M, Ringa V, Becquemont L (2014) Primary care management of non-institutionalized elderly diabetic patients: the S.AGES cohort—baseline data. Prim Care Diabetes. doi:10.1016/j.pcd.2014.07.004
Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW (1963) Studies of illness in the aged. The index of ADL: a standardized measure of biological and psychosocial function. JAMA 185:914–919
Barberger-Gateau P, Dartigues JF, Letenneur L (1993) Four instrumental activities of daily living score as a predictor of one-year incident dementia. Age Ageing 22(6):457–463
Marc LG, Raue PJ, Bruce ML (2008) Screening performance of the 15-item geriatric depression scale in a diverse elderly home care population. Am J Geriatr Psychiatry 16(11):914–921
http://www.insee.fr/fr/bases-de-donnees/bsweb/serie.asp?idbank=000642334.
http://www.ameli.fr/professionnels-de-sante/medecins/votre-convention/tarifs/index.php.
Huscher D, Mittendorf T, von Hinuber U, Kotter I, Hoese G, Pfafflin A, Bischoff S, Zink A (2014) Evolution of cost structures in rheumatoid arthritis over the past decade. Ann Rheum Dis 74(4):738–745
Martin BI, Deyo RA, Mirza SK, Turner JA, Comstock BA, Hollingworth W, Sullivan SD (2008) Expenditures and health status among adults with back and neck problems. JAMA 299(6):656–664
Lubeck DP (2001) A review of the direct costs of rheumatoid arthritis: managed care versus fee-for-service settings. Pharmacoeconomics 19(8):811–818
Yelin E, Wanke LA (1999) An assessment of the annual and long-term direct costs of rheumatoid arthritis: the impact of poor function and functional decline. Arthritis Rheum 42(6):1209–1218
Michaud K, Messer J, Choi HK, Wolfe F (2003) Direct medical costs and their predictors in patients with rheumatoid arthritis: a three-year study of 7,527 patients. Arthritis Rheum 48(10):2750–2762
Sabariego C, Brach M, Stucki G (2011) Determinants of major direct medical cost categories among patients with osteoporosis, osteoarthritis, back pain or fibromyalgia undergoing outpatient rehabilitation. J Rehabil Med 43(8):703–708
Margolis JM, Juneau P, Sadosky A, Cappelleri JC, Bryce TN, Nieshoff EC (2014) Health care resource utilization and medical costs of spinal cord injury with neuropathic pain in a commercially insured population in the United States. Arch Phys Med Rehabil 95(12):2279–2287
Walen HR, Cronan PA, Bigatti SM (2001) Factors associated with healthcare costs in women with fibromyalgia. Am J Manag Care 7 Spec No:SP39-47
Dellaroza MS, Pimenta CA, Lebrao ML, Duarte YA (2013) Association of chronic pain with the use of health care services by older adults in Sao Paulo. Rev Saude Publica 47(5):914–922
Evans RL, Hendricks RD, Lawrence KV, Bishop DS (1988) Identifying factors associated with health care use: a hospital-based risk screening index. Soc Sci Med 27(9):947–954
Dagenais S, Caro J, Haldeman S (2008) A systematic review of low back pain cost of illness studies in the United States and internationally. Spine J 8(1):8–20
Liotta G, Brenna A (2007) Evolution of the in-patient hospital expenditure for the elderly in Italy: 1996–2001 comparison. Arch Gerontol Geriatr 45(2):169–177
Blanco-Moreno A, Urbanos-Garrido RM, Thuissard-Vasallo IJ (2013) Public healthcare expenditure in Spain: measuring the impact of driving factors. Health Policy 111(1):34–42
Smith M, Davis MA, Stano M, Whedon JM (2013) Aging baby boomers and the rising cost of chronic back pain: secular trend analysis of longitudinal Medical Expenditures Panel Survey data for years 2000 to 2007. J Manipulative Physiol Ther 36(1):2–11
Fox MT, Persaud M, Maimets I, O'Brien K, Brooks D, Tregunno D, Schraa E (2012) Effectiveness of acute geriatric unit care using acute care for elders components: a systematic review and meta-analysis. J Am Geriatr Soc 60(12):2237–2245
Thompson E, Broadbent J, Bertino MD, Staiger PK (2015) Do pain-related beliefs influence treatment adherence? A systematic review. Clin J Pain. doi:10.1097/AJP.0000000000000235
Author contributions
Lazkani A: study design, data analysis, and manuscript preparation.
Becquemont L: study design, data analysis, and manuscript preparation.
Delespierre T: study design, data analysis, and manuscript preparation.
Bauduceau B: study design, manuscript revision, and approval of the final version for publication.
Pasquier F: study design, manuscript revision, and approval of the final version for publication.
Bertin P: study design, manuscript revision, and approval of the final version for publication.
Berrut G: study design, manuscript revision, and approval of the final version for publication.
Corruble E: study design, manuscript revision, and approval of the final version for publication.
Falissard B: study design, manuscript revision, and approval of the final version for publication.
Doucet J: study design, manuscript revision, and approval of the final version for publication.
Forette F: study design, manuscript revision, and approval of the final version for publication.
Hanon O: study design, manuscript revision, and approval of the final version for publication.
Benattar-Zibi L: study design, manuscript revision, and approval of the final version for publication.
Piedvache C: data analysis, manuscript revision, and approval of the final version for publication.
Conflicts of interest
Lazkani A has no conflict of interest.
Becquemont L received consulting fees from Sanofi-Aventis, Pfizer and Servier, and lecture fees from Genzyme, GlaxoSmithKline, Bristol-Myers Squibb, and Merck Sharp & Dohme; close family member working at Sanofi France.
Delespierre T has no conflict of interest.
Bauduceau B received consulting fees from Sanofi-Aventis, Bristol-Myers Squibb, Merck Sharp & Dohme, Roche, and Novo Nordisk.
Bertin P received consulting fees from Sanofi-Aventis, Pfizer, Ethypharm and Reckitt Benckiser, and speaking fees from Genevrier, Roche, Bristol-Myers Squibb, and Merck Sharp & Dohme.
Berrut G received fees from Sanofi, Lundbeck, Eisai, Novartis, MSD, Amgen, Boehringer Ingelheim, and Bayer.
Corruble E received consulting fees from Servier, Lundbeck, Sanofi-Aventis, Bristol Myers Squibb, and Eisai.
Doucet J received speaking fees from Novo Nordisk, consulting fees from Sanofi-Aventis, Novo Nordisk, and Merck Serono, and has a research partnership with Lilly.
Falissard B received consulting fees from Sanofi-Aventis, Servier, Roche, AstraZeneca, Grünenthal, Lilly, HRA, Boehringer Ingelheim, Bayer, Novartis, Genzyme, Stallergenes, Daiichi, Otsuka, and BMS.
Forette F received speaking and consulting fees from AstraZeneca, Bayer, BMS, Esaï, Exonhit, Fabre, Ipsen, Janssen-Cilag, Lilly, Lundbeck, Novartis, MSD, Merz, Pfizer, Roche, Sanofi-Aventis, Servier, Schwartz Pharma, Specia, Warner–Lambert, and Wyeth.
Hanon O received speaking and consulting fees from AstraZeneca, Bayer, BMS, Boehringer, Esaï, Exonhit, Janssen-Cilag, Lundbeck, Novartis, Pfizer, Sanofi-Aventis, and Servier.
Pasquier F is an investigator for Pfizer, Piramal, Roche, Lilly, Astra Zeneca, Noscira, Pharnext, Forum Pharmaceutical, and GE Healthcare and received consulting fees from Lilly, Novartis, Nuticia, and Sanofi.
Benattar-Zibi L has no conflict of interest.
Piedvache C has no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
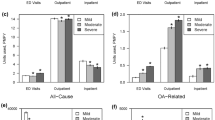
Supplementary Figure 1
(GIF 209 kb)
Supplementary table 1
(DOC 67 kb)
Supplementary table 2
(DOC 57 kb)
Supplementary online table 3
(DOC 30 kb)
Supplementary table 4
(DOC 27 kb)
Supplementary table 5
(DOC 97 kb)
Rights and permissions
About this article
Cite this article
Lazkani, A., Delespierre, T., Bauduceau, B. et al. Healthcare costs associated with elderly chronic pain patients in primary care. Eur J Clin Pharmacol 71, 939–947 (2015). https://doi.org/10.1007/s00228-015-1871-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-015-1871-6