Abstract
Lignans are biologically active compounds widely distributed, recognized, and identified in seeds, fruits, and vegetables. Lignans have several intriguing bioactivities, including anti-inflammatory, antioxidant, and anticancer activities. Nrf2 controls the expression of many cytoprotective genes. Activation of Nrf2 is a promising therapeutic approach for treating and preventing diseases resulting from oxidative injury and inflammation. Lignans have been demonstrated to stimulate Nrf2 signaling in a variety of in vitro and experimental animal models. The review summarizes the findings of fourteen lignans (Schisandrin A, Schisandrin B, Schisandrian C, Magnolol, Honokiol, Sesamin, Sesamol, Sauchinone, Pinoresinol, Phyllanthin, Nectandrin B, Isoeucommin A, Arctigenin, Lariciresinol) as antioxidative and anti-inflammatory agents, affirming how Nrf2 activation affects their pharmacological effects. Therefore, lignans may offer therapeutic candidates for the treatment and prevention of various diseases and may contribute to the development of effective Nrf2 modulators.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recent studies have focused on identifying polyphenols and their derivatives in various biofluids concerning possible health-promoting characteristics (Rothwell et al. 2016). Polyphenols are secondary metabolites in a wide range of vegetables and fruits (González-Vallinas et al. 2013). Because of their antioxidative characteristics, polyphenols are known to prevent disease, slow its progression, and even support the healing process (Ramos 2008; González-Vallinas et al. 2013).
Chemistry and appearance of lignans
Lignons are a group of secondary metabolites found in plants first identified by Haworth as polyphenols (Teponno et al. 2016; Haworth 1942). Due to their steroid-analogous chemical structure, lignans are recognized as phytoestrogens and play a role in the prevention and treatment of diseases (Rodríguez-García et al. 2019; Santini et al. 2017). Lignans also have a variety of biochemical properties, such as anti-inflammatory (Pietrofesa et al. 2016; Mohamed et al. 2022), antioxidant (H. Lu and Liu 1992), antitumor (Capilla et al. 2001), and neuroprotective (Q. Wang et al. 2019) properties.
Lignans are present in over 70 plant groups. Numerous lignan ingredients exist in the Lauraceae, Annonaceae, Orchidaceae, Berberidaceae, and Schisandraceae families (Pan et al. 2009; Kaplan 1942; X. Q. Wu et al. 2019c; J. Zhang et al. 2014). Vegetables and fruits, beans, whole grain grains, and oilseeds are the main sources of dietary lignans (Landete 2012; Thompson et al. 2006). Sesame and flax seeds are the most abundant sources of lignans in food plant components (Coulman et al. 2005).
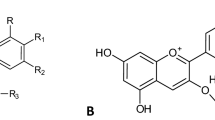
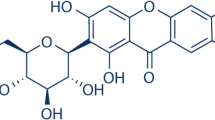
Lignan is composed of two phenylpropanoid C6-C3 units connected by extra ether, lactone, or carbon bonds at the β and β’ carbons (Lewis and Davin 1999). Lignans are classified as diphenolic compounds and are derived from the biosynthesis route of shikimic acid (Imai et al. 2006). There are two types of lignans: lignan and neolignan. They are distinguished by the existence or absence of a phenylpropanoid 8,8′-bond between their monomers, as well as by the smaller number and more restricted evolutionary distribution of lignans (Gottlieb 1972). Lignans are categorized based on the type of extra side groups they contain, which can be either aliphatic or aromatic. Furthermore, four families of linear lignans can be distinguished based on their ability to incorporate oxygen into the framework, namely, lignans derived from butane, butanolides, monoepoxylignans, tetrahydrofuran derivatives, bisepoxylignans, and derivatives of 3,7-dioxabicyclo (3.3.0)-octane derivatives. A C-7/C-6" linkage allows for further cyclization, which leads to the creation of a sizable class of molecules known as cyclolignans (Freudenberg and Weinges 1961). Secoisolariciresinol (Seco), syringaresinol (Syr), matairesinol (Mat), lariciresinol (Lari), pinoresinol (Pin), sesamin (Ses), medioresinol (Med), 7′-hydroxymatairesinol, and isolariciresinol are among the diphenolic chemical compounds that produce lignans. Furofuran is categorized as Pin, Med, Syr, Lari, and Ses; dibenzylbutyrolactone is assigned to Mat; 9,9′-dihydroxydibenzylbutane is assigned to Seco; and 9,9′-dihydroxyaryltetralin is assigned to Isolariciresinola (Umezawa 2003). They are mostly unbound in nature, although a few are glycosides. The biological functions of lignans come in a wide variety of structurally distinct types (Teponno et al. 2016; Pan et al. 2009).
Pharmacokinetics of lignans
Lignans are present as both aglycones and glycosides in plants (Smeds et al. 2007). Lignan glycosides are converted by gut flora into enterolignans (enterolactone and enterodiol), which are then absorbed by the gastrointestinal tract and mainly undergo glucuronidation and sulfation in the liver and enterocytes (Hoikkala et al. 2003; Axelson and Setchell 1981). Following oral administration of flaxseed to rats, the majority of the lignan metabolites (other than SDG) were found in the portal vein in their conjugated form (Axelson and Setchell 1981). However, SDG must be deglucosylated in the intestines or enterocytes before conjugation in the enterocytes (SP Borriello et al. 1985a). Additionally, after conjugation, flaxseed and associated lignans are primarily transported through the blood and stored mainly in the gut, liver, prostate, brain, and lung (Murray et al. 2007; Mukker 2013). Furthermore, enterolignans can be found in a variety of body fluids, including plasma, saliva, and prostatic fluid (Pamies et al. 2011).
The two primary ways lignan metabolites are eliminated in different animals are urine and feces. The consumption of flaxseed increases the number of conjugated enterolignans excreted in the feces (Bach Knudsen et al. 2003). The increased enterolignans in feces may be due to enterohepatic circulation or insufficient absorption. The bile excretes lignan glucuronides, which are subsequently deglucuronidated by bacterial-glucuronidase activity (Jeff Sfakianos et al. 1997a; J. Sfakianos et al. 1997b). However, the majority of the lignans excreted in the urine are eliminated as enterolignan glucuronide, while only a small quantity is eliminated as sulfates and aglycones (Adlercreutz et al. 1995; Axelson and Setchell 1980) (Fig. 1). Several factors influence the hydrolysis required to liberate lignans from sugars, produce enterolignans, and make these compounds bioavailable among individuals due to consumption patterns, altered microbiota, and antibiotic use (Kilkkinen et al. 2001; S. P. Borriello et al. 1985b; Kilkkinen et al. 2002). The pharmacokinetics of specific lignans are provided as a supplementary file (Supplementary 1).
Pharmacodynamic lignans
Since lignans are phenolic and phytoestrogen substances, numerous studies have investigated their therapeutic potential through various pathways (J. Sfakianos et al. 1997b; Jang et al. 2022). The antioxidant effect has been well-established as an important pathway for the protective and disease-prevention properties of lignans (Kitts et al. 1999). Lignans increase the amounts of catalase (CAT), superoxide dismutase (SOD), and glutathione (GSH), which serve as antioxidants in tissues and protect cells from oxidative damage caused by reactive oxygen species (ROS) (S. P. Ip and Ko 1996b; You and Cho 2021; Nagappan et al. 2018). In addition, the upregulation of antioxidant signals such as heme oxygenase-1 (HO-1), nuclear factor erythroid 2-related factor 2 (Nrf2), and Kelch-like ECH-associated protein 1 (Keap1) by lignans has also been reported (Jiang et al. 2016; Côrtes et al. 2012; V. K. Bajpai et al. 2017b). Furthermore, the anti-inflammatory effect of lignans plays an important role in organ protection. It has been reported that dietary lignans and metabolites regulate inflammation by lowering proinflammatory mediators and suppressing the nuclear factor-κB (NF-κB), MAPK, and JAK/STAT3 signaling pathways (V. K. Bajpai et al. 2018; H. Q. Wang et al. 2022). Lignans also have antiangiogenic, antiproliferative, and anticancer effects in various cancers by regulating matrix metalloproteinases, m-TOR, EGRF, VEGF, and steroid receptor coactivator-3 (Dabrosin et al. 2002; Rauf et al. 2018). Because of their estrogenic potential, lignans have an anti-menopausal effect and decrease the risk of breast cancer (Velentzis et al. 2009).
In addition, a clinical study revealed that consuming lignans over the long term had significant effects on reducing women’s and men’s risk of coronary heart disease over the long term (Hu et al. 2021). This result is in accordance with the effects of lignans on heart disease associated with menopause. Foods high in lignans have been shown to lower lipid oxidation, total cholesterol, and triglyceride levels, which can help to avoid cardiovascular disease and lessen hepatic inflammation caused by a high-fat diet (Nakamura et al. 2020; Xiao et al. 2021). Moreover, lignans have antiosteoporosis (Choi et al. 2014), antifungal (K. M. Li et al. 2019), anti-asthmatic (Iwasaki et al. 1996), and antiviral (Charlton 1998) effects.
Nrf2 signaling pathway
Nrf2 signaling pathway and oxidative stress
Oxidative stress initiates and progresses several diseases (Sies et al. 2017; Gorrini et al. 2013; Z. Chen and Zhong 2014; Luc et al. 2019). Generally, ROS refers to oxygen-containing molecules that have reactive characteristics. They include nonradical compounds such as hydrogen peroxide (H2O2) as well as free radicals such as superoxide (O•2) and hydroxyl (HO•). These molecules are primarily generated from the oxygen used in different metabolic processes that primarily originate in the endoplasmic reticulum (ER), peroxisomes, and mitochondria (Finkel 2012; Handy and Loscalzo 2012). Since varying ROS levels can cause various biological reactions, modulating intracellular ROS levels is essential for maintaining cellular equilibrium (Cairns et al. 2011; Sena and Chandel 2012). Additionally, ROS can serve as signaling molecules that activate NF-κB signaling and proinflammatory mediators (Gloire et al. 2006). However, biological components such as DNA, proteins, and lipids are damaged by excessive ROS generation. This circumstance results in oxidative stress (Gulcin et al. 2010; Altay et al. 2019).
Antioxidants protect biological systems from the damaging effects of ROS and free radicals (Köse et al. 2015). It was discovered in 1994 that the transcription factor Nrf2 regulates the expression of the beta-globin genes. Thus, it plays a critical role in regulating the production of antioxidants within cells (Moi et al. 1994; Sporn and Liby 2012).
The most significant modulator of Nrf2 signaling is the E3 ligase adaptor Keap1 (Hayes and Dinkova-Kostova 2014; Suzuki et al. 2013). Under normal circumstances, the Keap1-Cullin 3 (CUL3) E3 ligase complex and glycogen synthase kinase 3 (GSK-3) inactivate Nrf2 (Hoeflich et al. 2000). When there is oxidative stress, Keap1 is oxidized, making it incapable of binding to Nrf2. This triggers Nrf2 to become stabilized and enter the nucleus (Cuadrado et al. 2019, 2018). In response to Nrf2 translocation and binding to the antioxidant response element (ARE) transcription factor, antioxidant-related genes such as HO-1, NAD(P)H dehydrogenase quinone 1 (NQO1), and γ-glutamyl cysteine ligase modulatory (γ-GCS) are expressed (Radjendirane Venugopal and Jaiswal 1996; R. Venugopal and Jaiswal 1998). The increase in antioxidant enzymes, including superoxide dismutase, catalase, and glutathione, resulted in the cells re-establishing the oxidative/antioxidative balance (Taguchi et al. 2011; Meister 1983). Glutathione is an important antioxidant in human cells, produced by γ-GCS, ubiquinone, and tocopherols, which are effective antioxidants because they are produced in reduced forms by NQO1. HO-1 protects cells from ROS and raises ferritin levels to perform an essential antioxidant role (Consoli et al. 2021).
Nrf2 signaling pathway and inflammation
In addition to upregulating antioxidant gene expression, Nrf2 has a cytoprotective effect by controlling oxidative stress-induced inflammation (J. Ren et al. 2020). NF-κB is a pleiotropic factor that controls several processes, such as cell growth, development, survival, and proliferation, as well as immunity and inflammation (Abdel Moneim 2016). Nrf2 inhibits inflammation by inhibiting NF-κB and releasing proinflammatory cytokines (Q. Ma et al. 2003; W. Li et al. 2008). Nrf2 overexpression suppressed NF-κB activity, which decreased inflammatory cytokine levels in brain, liver, lung, and kidney models (Bhandari et al. 2021; Zeng et al. 2017; Dai et al. 2021; Aly et al. 2017; Hong et al. 2022). It has been shown that the Nrf2 target gene HO-1 blocks the transcription of adhesion molecules by NF-κB, potentially by reducing the amount of free intracellular iron in endothelial cells (Soares et al. 2004). While NF-κB signaling can control Nrf2-mediated antioxidant gene expression via overexpression of the canonical NF-κB component p65, increasing nuclear Keap1 levels results in reduced Nrf2/ARE signaling (M. Yu et al. 2011). Furthermore, it was shown that activating Nrf2 inhibited NF-κB/STAT3 signaling and reduced inflammation (Gong et al. 2020; Hou et al. 2022), and Nrf2 and STAT3 functioned together to control SLC7A11 throughout ferroptosis (Qiang et al. 2020). In addition, Nrf2 was stimulated as an adaptive defense against oxidative stress-induced NLRP3 inflammasome activation initiated by cholesterol crystals (Freigang et al. 2011). As a result of the interaction between Nrf2/keap1 and inflammatory signals such as NF-κB, STAT3, and the NLRP3 inflammasome, Nrf2 activation fundamentally enhances cytoprotection against cellular damaging stimuli, which induce oxidative stress and inflammation (Fig. 2).
Proposed dual antioxidant and anti-inflammatory effects of lignans by activating Nrf2 signaling pathway. This figure depicts the crosstalk between Nrf2, NF-κB, PI3K, and MAPK signaling and how lignans exert antioxidant and anti-inflammatory effects on modulating these signals and reducing oxidative stress. Increased reactive metabolites, free radicals, and ER stress raise Ca + 2 levels, leading to mitochondrial malfunction and an imbalance in the antioxidant and oxidative stress systems. Increased extracellular stressors and an imbalance in the intracellular antioxidant-oxidative stress system led to an increase in ROS generation, which in turn caused lipid peroxidation, protein oxidation, DNA damage, and the activation of inflammatory signals such as NF-κB, PI3K, and MAPK signaling. In response to the activation of ILRs, TNFRs, and TLRs, as well as elevated ROS levels, normal cells phosphorylate IKK, which activates IKK-B, and the P38, P65 complex, which activates NF-κB. Furthermore, ROS and activation of IL-1β receptor promote P38\MAPK\ERK\JNK signaling, which also activates NF-κB and NLRP-3 inflammasome. ROS and GPCR stimulate PI3K, then activates JAK/STAT3 signaling and NF-κB. Activated NF-κB migrates and translocate into the nucleus, where it binds with P65 and RelA at the binding site on DNA, activating the transcription of inflammatory genes such as cytokines, VCAM-1, ICAM, COX-1, ILs, and MMPs genes. Increased inflammatory gene transcription leads to increased levels of chemokines and cytokines such TNF-α, IL-1β, 1L-6, IL-18, TGF-β, and INF-γ. These cytokines promote inflammation, immunological response, and cell death. On the other hand, the CUL3-E3, Nrf2, Keap1 complex has two ways: it is still connected and results in Nrf2 degradation or it is detached to free active Nrf2, which is how lignans modify this signal. PI3K/AKT/GSK3B signaling reduces Nrf2 activation, whereas active Nrf2 also inhibits NF-κB. The active Nrf2 translocate to the nucleus and binds to ARE on DNA, activating the transcription of HMOX1, G6PD, GCLC, and TXN genes, increasing the levels of antioxidant proteins such as HO-1, GSH, SOD, CAT, and NADPH. These antioxidants prevent cell damage by inhibiting ROS and oxidative stress, which in turn prevents the production of inflammatory cytokines. Abbreviations: ROS; reactive oxygen species, ER; endoplasmic reticulum, ILRs; interleukin receptors; TNFRs, tumor necrosis factor receptors, TLRs Toll like receptors, IL-1; Interleukin-1, MAPK; mitogen-activated protein kinase, JNK; c-Jun N-terminal kinase, ERK; extracellular signal-regulated kinases, IKK; IkappaB kinase, NF-κB; nuclear factor-kappa B, JAK; Janus kinase, STAT3; signal transducer and activator of transcription 3, NLRP-3; NLR family pyrin domain containing-3, TGF-β; tumor growth factor betta, INF-γ; interferon gamma, COX; cyclooxygenase, ICAM; intercellular adhesion molecule, MMP; matrix metalloproteinase, GPCR; G protein coupled receptors, PI3K; phosphoinositide 3-kinase, AKT; protein kinase B, GSK-3β; glycogen synthase kinase 3-betta, Nrf2; nuclear factor erythroid 2-related factor 2, Keep1; Kelch-like ECH-associated protein 1, CUL3-E3; Cullin 3-E3, ARE; antioxidant response element, HO-1; heam oxygenase-1, GSH, reduced glutathione, CAT; catalase, SOD; superoxide dismutase, NADPH; nicotinamide adenine dinucleotide phosphate, G6PD; glucose-6 phosphate dehydrogenase, GCLC; glutamate cysteine ligase catalytic
However, additional methods for Nrf2 activation have been identified, and these involve kinase pathways such as those of mitogen-activated protein kinases (MAPK) (Rong Yu et al. 1999), phosphatidylinositol-3 kinase (Zheng et al. 2009; Keon Wook Kang et al. 2002), and atypical protein kinase(s) C (Numazawa et al. 2003). Additionally, Nrf2-regulated genes, such as inflammatory regulating and antifibrotic genes, were identified (Hybertson et al. 2011). Therefore, agents that upregulate Nrf2 and its activator will be suggested for further research to treat disorders accompanied by oxidant-antioxidant dysregulation and oxidative stress-induced inflammatory responses.
Neuroprotective effects of lignans and Nrf2 activation
Several studies reported that Nrf2 activation has a key role in the neuroprotective effects of lignans. Magnolol exhibits a neuroprotective effect in an experimental autoimmune encephalomyelitis model of multiple sclerosis mice. Magnolol treatment significantly decreased oxidative stress, evidenced by decreasing MDA, NO, and MPO while raising the levels of antioxidant enzymes in the brain and spinal cord and reducing inflammatory cell infiltration and proinflammatory cytokines mediated by upregulating the expression of Nrf2 (Bibi et al. 2022). Likewise, magnolol reduced depressive-like behaviors, inhibited proinflammatory cytokines, and increased anti-inflammatory cytokines in chronic unpredictable mild stress-induced depression by upregulating Nrf2 and HO-1 and increasing Nrf2 nuclear translocation (Tao et al. 2021). Also, the protective effects of sesamin on oxidative stress-related neurodegenerative diseases in rat pheochromocytoma PC12 cells were mediated by upregulating HO-1 expression, improving Nrf2 nuclear translocation (Hamada et al. 2011). Additionally, sesamol has an advantageous effect on the liver-brain axis, making it a potential neuroprotective treatment throughout the aging process. Sesamol treatment restored cellular redox equilibrium, protected against mitochondrial dysfunction, and increased antioxidant enzymes in H2O2-treated SH-SY5Y cells by activating Nrf2 and upregulating HO-1 and NQO1(Bo Ren et al. 2018).
Hepatoprotective effects of lignans and Nrf2 activation
Jiang et al. observed that Schisandrin B (Sch B) could remarkably protect the liver from APAP-induced hepatotoxicity, mainly by activating the Nrf2/ARE signal. Sch B administration increased the expression of Nrf2 downstream GCLC, NQO1, and Nrf2 nuclear accumulation (Jiang et al. 2016). Moreover, Sch B has been shown to treat CCl4-induced liver fibrosis via the Nrf2-ARE and TGF-β/Smad signals. Sch B dramatically reduced collagen accumulation and oxidative stress and inhibited HSC activation by disrupting the TGF-β/Smad signaling pathway (Qingshan Chen et al. 2017). Also, nectandrin B can protect hepatocytes from oxidative stress by activating the Nrf2/ARE pathway, regulated by ERK phosphorylation, and by inactivating GSK-3β in an AMPK-dependent manner (Jae-Sook Song et al. 2016).
Renoprotective effects of lignans and Nrf2 activation
Huang et al. reported that isoeucommin A derived from Eucommia ulmoides Oliv regulated the Nrf2/HO-1 signaling pathway in high-glucose-stimulated human renal mesangial cells and protected renal tubular epithelial cells from H2O2-stimulated oxidative injury. Isoeucommin A might mitigate kidney damage by enhancing the expression of SOD, glutathione, HO-1, and Nrf2 while significantly lowering the levels of TNF-α, IL-1β, IL-6, and MDA by stimulating the Nrf2/HO-1 signal (Qi Huang et al. 2021a).
Cardioprotective effects of lignans and Nrf2 activation
According to Han et al., Sch B prevents oxidative stress-induced cardiovascular diseases by enhancing Nrf2 expression and significantly decreases angiotensin II-induced oxidative stress, mitochondrial membrane-potential depolarization, and mortality in rat aortic endothelial cells (Han et al. 2018).
The modulatory effect of lignans on Nrf2
Schisandra chinensis
Schisandra chinensis Turcz (S. chinensis) and Schisandra sphenanthera family Schisandraceae are extensively dispersed in China, Japan, and Korea and are recognized for their five-flavor fruits (Hancke et al. 1999; S. Huang et al. 2021b). Schisandra fruit is a common herbal supplement in both Western phytotherapy and traditional Chinese medicine, and it is used to increase disease and stress tolerance, as well as physical performance (Szopa et al. 2017; Nowak et al. 2019; S. Huang et al. 2021b). Schisandra fruit extracts provide a wide variety of therapeutic advantages in both normal and pathological circumstances, including antioxidant, anti-inflammatory, anticancer, antibacterial, antiviral, hepatoprotective, cardioprotective, and hypoglycemic properties (Hancke et al. 1999; Nowak et al. 2019; Szopa et al. 2017; Szopa and Ekiert 2012). S. chinensis biologically active compounds have been reported to upregulate antioxidant enzymes while downregulating proinflammatory cytokines and inhibiting apoptosis (Oh et al. 2010; Chiu et al. 2008; Na Chen et al. 2008). Furthermore, ethanolic extract from S. chinensis fruit may directly scavenge ROS, lowering the growth inhibition of C2C12 cells induced by H2O2 alleviation and neutralizing ROS generated by phorbol myristate acetate-stimulated human polymorphonuclear leukocytes (Ji Sook Kang et al. 2014; Xiaojie Li et al. 1990).
Schisandrin A
Schisandrin A is a dibenzocyclooctadiene derivative derived from S. chinensis and S. sphenanthera. It has been demonstrated to have anti-inflammatory, antioxidant, renoprotective, and neuroprotective properties (Gui et al. 2020; Chuwen Li et al. 2018; Huyke et al. 2007). Schisandrin A, in general, increased the expression of Nrf2, HO-1, and Bcl-2 while decreasing the expression of Keap1, Bax, and caspase-3. This increased the level of GSH while diminishing the amount of MDA (Huijiao Lin et al. 2021).
Shisandrin A activates the Nrf2/HO-1 pathway by inhibiting the MAPK/PI3K/Akt pathway, thus protecting RAW 264.7 cells from LPS-induced inflammation and oxidative stress. Furthermore, schisandrin A effectively increased Nrf2 and HO-1 expression, decreased the LPS-stimulated increase in intracellular ROS, and inhibited macrophage infiltration (Kwon et al. 2018). In this context, Xu et al. observed that Sch A protects against LPS-induced mastitis by activating the Nrf2 signaling pathway and triggering autophagy via the AMPK-ULK1 signaling pathway while reducing the mTOR signaling system. Furthermore, Sch A reduced LPS-induced decreases in proinflammatory and mTOR phosphorylation while activating AMP-activated protein kinase (AMPK) and unc-51-like kinase 1 (ULK1) in murine mammary epithelial cells (Xu et al. 2020). Ni et al. reported that Sch modulates Nrf2 to prevent RANKL-induced ROS in vitro and in vivo to protect against OVX-induced bone loss. Sch promotes Nrf2 expression by inhibiting Nrf2 degradation and suppressing P65 phosphorylation, nuclear translocation, and degradation of IB (Ni et al. 2020).
Schisandrin B
Schisandrin B (Sch B) is an active dibenzooctadiene lignan found in the fruit of S. chinensis that has antitumor (Zhen Liu et al. 2012), anti-inflammatory (Checker et al. 2012), antioxidant (Siu-Po Ip and Ko 1996a), and neuroprotective (Giridharan et al. 2015) activities. Chen et al. demonstrated that Sch B treatment protects the lungs by increasing Nrf2 activation while decreasing the NF-κB pathway in OVA-induced airway hyperresponsiveness. It also reduced IgE levels, reduced pathological damage, and regulated inflammatory responses (Yaqin Chen et al. 2021). Similarly, Jia et al. reported that Sch B attenuated CS-induced pulmonary inflammation in mice by inhibiting NF-κB activation and increasing Nrf2 and HO-1 expression. Also, Sch B decreased TNF-α, IL-1β, IL-6, MPO, and MDA levels, while it increased antioxidants SOD and GSH (Jia et al. 2017).
Jiang et al. observed that Sch B can remarkably protect the liver from APAP-induced hepatotoxicity, mainly by activating the Nrf2/ARE signal. Sch B administration increased the expression of Nrf2 downstream GCLC, NQO1, and Nrf2 nuclear accumulation (Jiang et al. 2016). Moreover, Sch B has been shown to treat CCl4-induced liver fibrosis via the Nrf2-ARE and TGF-β/Smad signals. Sch B dramatically reduced collagen accumulation and oxidative stress and inhibited HSC activation by disrupting the TGF-β/Smad signaling pathway (Qingshan Chen et al. 2017). The hepatoprotective effects of Sch B include upregulation of CYP450 activity and Nrf2, NQO-1, and GST expression.
Sch B can increase Nrf2-driven thioredoxin expression in alum-induced peritonitis. In RAW264.7 cells, Sch B inhibited LPS/ATP-induced ROS production, JNK1/2 activation, caspase 1 activation, IL-1β release, and LDH production (Leong and Ko 2015). Sch B also activates the Nrf2 signaling pathway to inhibit LPS-induced inflammation in activated human umbilical vein endothelial cells. Sch B inhibited LPS-induced TNF-α, IL-8, ICAM-1, and VCAM-1 expression. Furthermore, it increased the expression of Nrf2 and HO-1 while decreasing the expression of NF-κB (Qiuning Lin et al. 2017). Furthermore, Zhang et al. reported in 2021 that Sch B Sch B reduced colitis-related epithelial cell damage and mitochondrial damage caused by increased ROS by modulating AMPK/Nrf2-dependent signaling and by inhibiting the activity of the NLRP3 inflammasome (Weiwei Zhang et al. 2021a).
Additionally, Sch B promotes neuroprotection and cardioprotection by increasing the expression of the Nrf2 signaling pathway. According to Han et al., Sch B is a Keap1 inhibitor that may be applied to prevent oxidative stress-induced cardiovascular diseases by enhancing Nrf2 expression. Furthermore, Sch B significantly decreased angiotensin II-induced oxidative stress, mitochondrial membrane-potential depolarization, and mortality in rat aortic endothelial cells (Han et al. 2018). Wu et al. (2019a, b, c, d) also demonstrated that enhancing antioxidants via the Nrf2 pathway alleviates anxiety-like behavior (Ying Wu et al. 2019d).
However, Sch B has been studied in vitro as an antioxidant. Chiu et al. (2011) studied how Sch B influences MAPK and Nrf2 activation, glutathione response induction, and apoptotic protection in H9c2 cells. They reported that Sch B activates redox-sensitive ERK/Nrf2 signaling, which results in a glutathione antioxidant response and the prevention of hypoxia/reoxygenation-induced apoptosis (Chiu et al. 2011). It also activates Nrf2/ARE-mediated oxidative response genes such as GCLC, NQO1, and HO-1, accumulating Nrf2 in the nucleus in HK-2 cells exposed to cisplatin-induced oxidative stress (Mei Li et al. 2012). In addition, Dong et al. revealed that the Nrf2/ARE pathway is important in preventing BaP from damaging HTR cells. Sch B upregulated Nrf2, HO1, NQO1, and SOD (Dong et al. 2016). Furthermore, in 2021, Ding et al. studied the ability of Sch B to protect HaCaT cells from oxidative damage caused by tert-butyl hydroperoxide by enhancing the Nrf2 signaling pathway and, as a result, antioxidant enzymes. Sch B significantly reduced DNA damage, protein oxidation, lipid peroxidation, ROS, and cell death while decreasing mitochondrial membrane potential (MMP) and ATP levels (Ding et al. 2018).
Schisandrin C
Schisandrin C from S. chinensis has considerable therapeutic benefits due to its antioxidant and anti-inflammatory characteristics (Panossian and Wikman 2008; Chun et al. 2014). Han et al. revealed that Sch C treatment improves relaxation and lowers aortic oxidative stress in rats provided subcutaneous Ang II infusions, indicating that Sch C might be used to treat vascular endothelial deficits. They also revealed that Keap1, a negative regulator of Nrf2, is a target of Sch C utilizing an expression plasmid and molecular docking (Han et al. 2019).
Magnolol
Magnolol (2-(2-hydroxy-5-prop-2-enylphenyl)-4-prop-2-enylphenol), derived from the stem bark of Magnolia officinalis, is mostly used in Chinese medicine (Kachur and Suntres 2020). Magnolol is known to have a variety of advantageous pharmacological effects, including anti-inflammatory (Kwak et al. 2012; Weeks 2009), antioxidant (Yung-Hsiang Chen et al. 2009), antibacterial (You-Jin Kang et al. 2012), anti-osteoclastic (Yang et al. 2008), antianxiety (Tsai et al. 2010), antidiabetic (Jong Soon Kang et al. 2008), antiplatelet, and anticarcinogenic (Shih and Chou 2012) properties.
Bibi et al. reported that magnolol exhibits a neuroprotective effect in an experimental autoimmune encephalomyelitis model of multiple sclerosis mice. Magnolol treatment significantly decreased oxidative stress by reducing MDA, NO, and MPO while raising the levels of antioxidant enzymes in the brain and spinal cord. In addition, Magnolol enhances the antioxidant defense mechanism and reduces inflammatory cell infiltration and proinflammatory cytokines by upregulating the expression of Nrf2 and suppressing the expression of iNOS and cleaved caspase-3 (Bibi et al. 2022). Likewise, Tao et al. reported that magnolol reduced depressive-like behaviors, inhibited proinflammatory cytokines, and increased anti-inflammatory cytokines in chronic unpredictable mild stress-induced depression via Nrf2/HO-1/NLRP3 signaling. Magnolol increases the expression of Nrf2 and HO-1, increases Nrf2 nuclear translocation, lowers ROS levels, and decreases the expression of NLRP3, caspase-1, and inflammatory cytokines (Tao et al. 2021).
According to Lu et al. in 2020, magnolol may play a role in the mitigation of periodontitis by suppressing LPS-induced inflammation in macrophages through its activation of HO-1. Magnolol significantly stimulated the Nrf2/HO-1 cascade and the p38 MAPK pathway. Magnolol administration significantly reduced inflammatory responses, as revealed by suppressing proinflammatory cytokines and NF-κB activation, with a substantial increase in Nrf2 nuclear translocation and HO-1 activity (Sheng-Hua Lu et al. 2015). In addition, Liu et al. demonstrated that upregulation of Nrf2 signals improved wound healing and reduced inflammation in diabetic patients with periodontal disease. Magnolol increases the expression of Nrf2 and HO-1, diminishes the levels of IL-6 and IL-8, and attenuates the production of ROS caused by advanced glycation end products (Chia-Ming Liu et al. 2021).
Sesame oil
Sesame (Sesamum indicum L.) is an ancient oilseed crop prevalent in subtropical and tropical areas (Bedigian and Harlan 1986). Sesame oil has antioxidant and health-promoting characteristics due to tocopherols, tocotrienols, and lignans (Pathak et al. 2014; Namiki 2007). Sesame lignans are known for their beneficial effects, which include decreasing blood glucose and cholesterol levels, protecting against cancer and cardiovascular disease, and relieving postmenopausal symptoms (D. Wu et al. 2019a). Sesamin and sesamol are the two main lignans in sesame (Namiki 2007; Majdalawieh and Mansour 2019).
Sesamin
Sesamin 4-[(3S,6S)-3-(3,4-dihydroxyphenyl)-1,3,3a,4,6,6a-hexahydrofuro[3,4-c]furan-6-yl]benzene-1,2-diol has been studied extensively for its several potential functions, including hepatoprotective (Ide et al. 2001), antitumor (Hibasami et al. 2000), antihypertensive (Miyawaki et al. 2009), anti-inflammatory (K. Li et al. 2016), and antioxidant (Lei et al. 2012) properties. According to in vivo and in vitro studies by Wang et al. (2021a, b), sesamin significantly mitigates I/R-induced intestinal damage in rats by increasing the expression of Nrf2, HO-1, and NQO1 (Yilin Wang et al. 2021b). In 2019, Kong et al. reported that sesamin on chondrocytes stimulated by IL-1β from human osteoarthritis patients. They demonstrated that sesamin treatment significantly decreased IL-1β-induced PGE2, NO, and MMP13 production. Sesamin also promoted the expression of Nrf2 and HO-1 and inhibited IL-1β from phosphorylating NF-κB p65 and IκB (Kong et al. 2016). Additionally, Bai et al. (2019) investigated the preventive effect of sesamin against dextran-induced UC via the activation of Nrf2-targeted genes. Sesamin protects against UC, and this effect is related to activated AKT/ERK and improved Nrf2 signaling (Bai et al. 2019). Additionally, Hamada et al. observed the effect of sesamin on oxidative stress-related neurodegenerative diseases in rat pheochromocytoma PC12 cells through activating Nrf2/ARE signaling. Sesamin promoted HO-1 expression, improved Nrf2 nuclear translocation, and suppressed p38 MAPK activation and intracellular ROS concentrations (Hamada et al. 2011).
Sesamol
Sesamol (1,3-benzodioxol-5-ol) is a lignan with chemopreventive, antioxidant (Kanu et al. 2010), antibacterial, antifungal (Rao et al. 2013), anti-inflammatory (Chu et al. 2010), and neuroprotective (Kanu et al. 2010) properties. According to Ren et al. (2018), sesamol has an advantageous effect on the liver-brain axis, making it a potential neuroprotective treatment throughout the aging process. Sesamol treatment restored cellular redox equilibrium, protected against mitochondrial dysfunction, and increased antioxidant enzymes in H2O2-treated SH-SY5Y cells by activating Nrf2. Furthermore, sesamol notably decreased oxidative stress-induced cognitive impairments, lowered inflammatory cytokines, and upregulated HO-1 and NQO1(Bo Ren et al. 2018).
Saururus chinensis
S. chinensis dried stems have been used for centuries in China, Japan, and Korea and exhibit a variety of biological actions, including anti-inflammatory (Lee et al. 2006), antitumor (Hodges et al. 2004), antioxidant (Rajbhandari et al. 2001), hepatoprotective (Lishu Wang et al. 2009), anticancer (Do et al. 2013), cholesterol-lowering (Yun et al. 2007), and bone protective (Gao et al. 2018) activities. According to Jung et al., S chinensis lignans can potentially treat inflammation by modulating the Nrf2/HO-1 signal. S. chinensis lignans can inhibit the production of inflammatory cytokines in response to LPS. These lignans were also observed to significantly inhibit LPS-induced production of iNOS, COX-2, IL-6, and TNF-α. Furthermore, these lignans promote the nuclear translocation of Nrf2 and the expression and level of HO-1 (Jung et al. 2019).
The unique lignan Sauchinone isolated from Saururus chinensis (Saururaceae) has been shown to exhibit anti-inflammatory (Min et al. 2009), antioxidant (D. Zhou and He 2022), antiapoptotic (Hyun Song et al. 2003), and hepatoprotective (Sung and Kim 2000) characteristics. Kay et al. showed that sauchinone protects the liver from acetaminophen-induced toxicity by activating Nrf2, which is mediated by activated PKCδ, resulting in the inhibitory phosphorylation of GSK3. In addition, sauchinone upregulates Nrf2 expression and enhances the nuclear accumulation of Nrf2 and the production of the reporter gene for the ARE, glutamate-cysteine ligase, and NQO1 protein, all of which assist in restoring the glutathione content of the liver. Sauchinone treatment thereby improved Nrf2 phosphorylation while decreasing its interaction with Keap1. Furthermore, it inhibits GSK3 phosphorylation, activates PKC, and upregulates Nrf2 activity (Kay et al. 2011).
Pinoresinol
Pinoresinol diglucoside (PDG) is one of the principal lignans extracted from Eucommia ulmoides. According to a previous study, PDG has numerous pharmacological properties, including anti-inflammatory (During et al. 2012), antioxidant (Tebboub et al. 2018), antihypertensive (L. F. Luo et al. 2010), and tumor‐suppressive (Horn-Ross et al. 2003) properties. According to Zhang et al., PDG inhibits inflammatory and oxidative damage caused by I/R in a mouse model of middle cerebral artery obstruction. PDG treatment dramatically increased the activities of SOD, GSH-Px, and GSH and decreased lipid peroxidation while significantly decreasing the levels of the cytokines TNF-α, IL-1β, and IL-6 in mouse brain tissue. PDG may also promote Nrf2 and HO-1 expression and suppress NF-κB activation (Yi Zhang et al. 2021b).
Phyllanthin
In the plant extract of the Phyllanthus amarus family of the Euphorbiaceae, phyllanthin is a significant bioactive lignan component that has been extracted and has been shown to have antibacterial action (Adegoke et al. 2010). Phyllanthin has been shown to have anti-inflammatory (Harikrishnan et al. 2018), hepatoprotective (Krithika et al. 2015), antitumor (H. Wang et al. 2021a), antibacterial (Upadhyay et al. 2010), and antioxidant (Chirdchupunseree and Pramyothin 2010) properties.
Yuan et al. investigated how phyllanthin protects the ischemic brain, suggesting its use in treating CIR and associated damage. CIR inhibited the expression of Nrf2, AMPK, and NF-κB, indicating that it stimulates crosstalk between the NF-κB and Nrf2 pathways. However, it increased IL-10 levels in chemokines, lowered inflammatory cytokines, and increased antioxidative enzyme activity (Yuan et al. 2021). Additionally, Wu et al. demonstrated that phyllanthin and hypophyllanthin decreased the Th2 response in mice induced with OVA-induced asthma. A significant reduction in SOD, NO, GSH, and MDA was observed by PA, as well as a significant reduction in OVA-induced increases in IgE levels. As a result of PA treatment, there was a significant reduction in the levels of the Th2 cytokines IL-4 and IL-6, as well as immune-inflammatory markers such as IL-1β, TNF-α, and TGF-β, as well as Nrf2, HO-1, and iNOS, which were elevated (Wei Wu et al. 2019b).
Nectandrin B
Nutmeg is the dried extract of the Myristica fragrans Houtt plant and has long been used as a spice as a remedy for diarrhea (Nguyen et al. 2010; Van Gils and Cox 1994). It has also been shown to have anti-inflammatory, antihyperlipidemic, and antiatherosclerotic effects (Olajide et al. 1999; Ram et al. 1996). Nectandrin B is a nutmeg extract that exhibits antioxidant and anti-inflammatory properties as well as a powerful activating impact on AMPK signaling (Nguyen et al. 2010; Nakano et al. 2017). Also, nectandrin B can protect hepatocytes from oxidative stress by activating the Nrf2/ARE pathway, regulated by ERK phosphorylation, and by inactivating GSK-3β in an AMPK-dependent manner (Jae-Sook Song et al. 2016).
Isoeucommin A
Eucommia ulmoides Oliv contains a wide variety of bioactive compounds, including lignans, which possess powerful antioxidative and anti-inflammatory properties (Fujikawa et al. 2010; D. Luo et al. 2014). Huang et al. reported that isoeucommin A derived from Eucommia ulmoides Oliv regulated the Nrf2/HO-1 signaling pathway in high-glucose-stimulated human renal mesangial cells and protected renal tubular epithelial cells from H2O2-stimulated oxidative injury. Isoeucommin A might mitigate kidney damage by enhancing the expression of SOD, glutathione, HO-1, and Nrf2 while significantly lowering the levels of TNF-α, IL-1β, IL-6, and MDA by stimulating the Nrf2/HO-1 signaling process (Qi Huang et al. 2021a). As a result, diabetic nephropathy (DN) models in vitro and in vivo could be reduced due to reduced oxidative stress and inflammation.
Arctigenin
Arctigenin (AR) is an active compound found in Arctium lappa L (A lappa), a well-known medicinal herb and nutritional supplement in traditional medicine (Pharmacopoeia 2010). AR has attracted the interest of investigators due to its anti-inflammatory (Kou et al. 2011), antioxidant (Wen-zhou Zhang et al. 2015), antiviral (Kim et al. 2011), antidiabetic (Y. Zhou et al. 2023), and neuroprotective (Fan et al. 2012) actions. Salama et al. observed whether arctigenin might alleviate cadmium-induced nephrotoxicity by reducing ERS and targeting Nrf2 and NF-κB signaling. Arctigenin promoted the nuclear translocation of Nrf2 and enhanced the activity of the redox-regulating enzymes HO-1 and NQO1. Furthermore, arctigenin inhibited cadmium-induced nuclear translocation of NF-κB and the downstream proinflammatory cytokines TNF-α and IL-1β (Salama et al. 2021).
Lariciresinol
Isatis indigotica (Ban-Lan-Gen) is a prevalent, significant, and popular herbal medicine for the clinic as an antiviral plant (Ye et al. 2011). Lariciresinol is an antioxidant (Vivek K Bajpai et al. 2017a), antiviral (B. Zhou et al. 2017), anticancer (Z. J. Ma et al. 2016), and antidiabetic (Alam et al. 2022) lignan extract from Isatis indigotica. A study by Bajpai et al. showed that Lariciresinol inhibits ROS production in RAW 264.7 cells and promotes antioxidant enzyme transcription and translation via Nrf2-mediated HO-1 activation via the p38 signaling pathway. Furthermore, lariciresinol treatment increased the transcriptional and translational activity of Nrf2 and HO-1, which counteracted ROS formation (Vivek K Bajpai et al. 2017a).
In silico analysis of lignans binding to Keap1
A major objective of our research was to provide in silico evidence that lignans bind Keap1, thus potentially serving as Nrf2 activators. In molecular docking (MD), ligands are examined for their binding mechanisms, and their biological properties are confirmed. MD was used to predict ligand binding against targeted proteins at the molecular level using PyRx software (Dallakyan et al. 2015). To determine the binding affinity, the crystal structure of the Keap1 kelch domain was retrieved from PDB ID: 4L7B. As a result of a previous study, the amino acids that interact with the protein were identified (Jnoff et al. 2014). Using AutoDock Tools, all missing atoms were added, Kollman charges were added, and pdbqt files were generated as a result (Morris et al. 2009). The 2D structure of the ligands was sketched using Chamedraw ultra, and Chem3D Pro 12.0 was used to minimize energy and export the pdb files of the ligands (Cousins 2011). The grid box dimensions were set up using PyRx to accommodate all the residues in the protein’s binding pocket. PyRx was also used to produce the required data files. The Discovery Studio visualizer program was used to examine and display the ligand‒protein complexes (Biovia 2017). To validate the MD protocol, we performed redocking of the cocrystallized ligands into the active site of Keap1. According to previous literature, the root mean square deviation (RMSD) value for the redocked structure is < 2.0 Å (Yusuf et al. 2008). After the validation process, we docked our ligands into the active site of the target protein and selected the pose with the lowest binding energy as the optimal pose. The binding energies of the investigated compounds (Fig. 3) are displayed in the following table (Table 1).
The following table shows the binding features and the favorable interactions of the best-docked pose of the promising compounds with key amino acid residues of Keap1. In addition to their well-fitting properties around the binding pocket, these compounds are suitable candidates for drug development, but we selected the one with the highest binding affinity (Table 2). Sesamin bound to docked Keap1 with a binding energy of − 10.8 kcal/mol. As shown in Fig. 4, sesamin fits properly in the target protein binding pocket by forming a hydrogen bond with Asn387. Additionally, it forms two π-π and two π-sigma interactions with Tyr334, Tyr572, Arg415, and Ala556. Moreover, it forms C-H bonds with Gly364, Asn382, and Gly462 at distances of 3.33, 3.36, and 3.75 Å, respectively. Isoeucommin A binds well in the active site of the protein by forming hydrogen bonds with the key residues of the target protein. These amino acid residues are Ser383, Leu557, Ser602, and Val604. Additionally, it is an aromatic ring that forms one π-π interaction with Tyr572 at a distance of 4.15 Å and two π-sigma interactions with Arg415 and Ala556. Furthermore, it forms C-H bonds with Tyr334, Gly386, and Gly509 with bond lengths of 3.37, 3.53, and 3.43 Å, respectively. All these interactions allow isoeucommin A to bind with Keap1 in a stable manner. Sauchinone exhibits a binding energy value of − 10.2 kcal/mol with Keap1. Sauchinone interacts with seven active residues in the binding pocket of the target protein. These residues are Ser363, Arg415, Ser508, Ser555, Ala556, Tyr572, and Ser602. Two hydrogen bonds are formed between the oxygen atom of benzodioxole and Ser363 and Ser555 with bond lengths of 2.80 and 238 Å, respectively.
Docking models of sesamin, Isoeucommin A, and Sauchinone. A Superimposition of the re-docked (yellow) and co-crystallized (green) in the Keap1 active site. B Surface mapping and 3D plot of the promising docked compounds into Keap1. As shown in the figure, sesamin fits properly in the target protein binding pocket by forming a hydrogen bond with Asn387. Additionally, it forms two π-π and two π-sigma interactions with Tyr334, Tyr572, Arg415, and Ala556. Moreover, it forms C–H bonds with Gly364, Asn382, and Gly462. Isoeucommin A binds well in the active site of the protein by forming hydrogen bonds with the key residues of the target protein. These amino acid residues are Ser383, Leu557, Ser602, and Val604. Additionally, it is an aromatic ring that forms one π-π interaction with Tyr572 and two π-sigma interactions with Arg415 and Ala556. Furthermore, it forms C-H bonds with Tyr334, Gly386, and Gly509. All these interactions allow isoeucommin A to bind with Keap1 in a stable manner. Sauchinone interacts with seven active residues in the binding pocket of the target protein. These residues are Ser363, Arg415, Ser508, Ser555, Ala556, Tyr572, and Ser602. Two hydrogen bonds are formed between the oxygen atom of benzodioxole and Ser363 and Ser555
Future recommendation
The Nrf2 signaling pathway is essential for preventing oxidative stress and electrophile-induced cell damage. Numerous diseases and disorders have oxidative damage and excessive ROS generation as part of their etiology. Lignans comprise a fairly large class of organic substances with advantageous pharmacological characteristics. Various studies have shown that the therapeutic actions of certain lignans, both in vitro and in vivo, are mediated by Nrf2 activation. Thus, several of the pharmacological and biological actions of lignans may be explained by stimulation of the Nrf2 signaling pathway. Therefore, lignans are an excellent source for finding therapeutic candidates for the treatment/prevention of many disorders and potential leads in developing efficient Nrf2 modulators.
Data availability
No datasets were generated or analysed during the current study.
References
Abdel Moneim AE (2016) Indigofera oblongifolia prevents lead acetate-induced hepatotoxicity, oxidative stress, fibrosis and apoptosis in rats. PLoS ONE 11(7):e0158965. https://doi.org/10.1371/journal.pone.0158965
Adegoke A, Iberi P, Akinpelu D, Aiyegoro O, Mboto C (2010) Studies on phytochemical screening and antimicrobial potentials of Phyllanthus amarus against multiple antibiotic resistant bacteria. Int J Appl Res Nat Prod 3(3):6–12
Adlercreutz H, van der Wildt J, Kinzel J, Attalla H, Wähäla K, Mäkelä T et al (1995) Lignan and isoflavonoid conjugates in human urine. J Steroid Biochem Mol Biol 52(1):97–103
Alam MB, Ra JS, Lim JY, Song BR, Javed A, Lee SH (2022) Lariciresinol displays anti-diabetic activity through inhibition of α-glucosidase and activation and enhancement of insulin signaling. Mol Nutr Food Res 66(13):e2100751. https://doi.org/10.1002/mnfr.202100751
Altay A, Tohma H, Durmaz L, Taslimi P, Korkmaz M, Gulcin I et al (2019) Preliminary phytochemical analysis and evaluation of in vitro antioxidant, antiproliferative, antidiabetic, and anticholinergics effects of endemic Gypsophila taxa from Turkey. J Food Biochem 43(7):e12908. https://doi.org/10.1111/jfbc.12908
Aly MS, Galaly SR, Moustafa N, Mohammed HM, Khadrawy SM, Mahmoud AM (2017) Hesperidin protects against diethylnitrosamine/carbon tetrachloride-induced renal repercussions via up-regulation of Nrf2/HO-1 signaling and attenuation of oxidative stress. J Appl Pharm Sci 7(11):007–014
Axelson M, Setchell K (1980) Conjugation of lignans in human urine. FEBS Lett 122(1):49–53
Axelson M, Setchell K (1981) The excretion of lignans in rats—evidence for an intestinal bacterial source for this new group of compounds. FEBS Lett 123(2):337–342
Bach Knudsen KE, Serena A, Kjær AKB, Tetens I, Heinonen S-M, Nurmi T et al (2003) Rye bread in the diet of pigs enhances the formation of enterolactone and increases its levels in plasma, urine and feces. J Nutr 133(5):1368–1375
Bai X, Gou X, Cai P, Xu C, Cao L, Zhao Z et al (2019) Sesamin enhances Nrf2-mediated protective defense against oxidative stress and inflammation in colitis via AKT and ERK activation. Oxid Med Cell Longev 2019:2432416
Bajpai VK, Alam MB, Quan KT, Kwon K-R, Ju M-K, Choi H-J et al (2017a) Antioxidant efficacy and the upregulation of Nrf2-mediated HO-1 expression by (+)-lariciresinol, a lignan isolated from Rubia philippinensis, through the activation of p38. Sci Rep 7(1):1–10
Bajpai VK, Alam MB, Quan KT, Kwon KR, Ju MK, Choi HJ et al (2017b) Antioxidant efficacy and the upregulation of Nrf2-mediated HO-1 expression by (+)-lariciresinol, a lignan isolated from Rubia philippinensis, through the activation of p38. Sci Rep 7:46035. https://doi.org/10.1038/srep46035
Bajpai VK, Alam MB, Quan KT, Ju MK, Majumder R, Shukla S et al (2018) Attenuation of inflammatory responses by (+)-syringaresinol via MAP-Kinase-mediated suppression of NF-κB signaling in vitro and in vivo. Sci Rep 8(1):9216. https://doi.org/10.1038/s41598-018-27585-w
Bedigian D, Harlan JR (1986) Evidence for cultivation of sesame in the ancient world. Econ Bot 40:137–154
Bhandari R, Khanna G, Kaushik D, Kuhad A (2021) Divulging the Intricacies of Crosstalk Between NF-Kb and Nrf2-Keap1 Pathway in neurological complications of COVID-19. Mol Neurobiol 58(7):3347–3361. https://doi.org/10.1007/s12035-021-02344-7
Bibi T, Khan A, Khan AU, Shal B, Ali H, Seo EK et al (2022) Magnolol prevented brain injury through the modulation of Nrf2-dependent oxidative stress and apoptosis in PLP-induced mouse model of multiple sclerosis. Naunyn-Schmiedeberg’s Arch Pharmacol 395(6):717–733
Biovia DSJSD, CA, USA (2017) Discovery studio visualizer. 936. Accelrys software inc.
Borriello S, Setchell K, Axelson M, Lawson A (1985a) Production and metabolism of lignans by the human faecal flora. J Appl Bacteriol 58(1):37–43
Borriello SP, Setchell KD, Axelson M, Lawson AM (1985b) Production and metabolism of lignans by the human faecal flora. J Appl Bacteriol 58(1):37–43. https://doi.org/10.1111/j.1365-2672.1985.tb01427.x
Cairns RA, Harris IS, Mak TW (2011) Regulation of cancer cell metabolism. Nat Rev Cancer 11(2):85–95. https://doi.org/10.1038/nrc2981
Capilla AS, Sánchez I, Caignard DH, Renard P, Pujol MD (2001) Antitumor agents. Synthesis and biological evaluation of new compounds related to podophyllotoxin, containing the 2,3-dihydro-1,4-benzodioxin system. Eur J Med Chem 36(4), 389–93. https://doi.org/10.1016/s0223-5234(01)01231-4
Charlton JL (1998) Antiviral activity of lignans. J Nat Prod 61(11):1447–1451. https://doi.org/10.1021/np980136z
Checker R, Patwardhan RS, Sharma D, Menon J, Thoh M, Bhilwade HN et al (2012) Schisandrin B exhibits anti-inflammatory activity through modulation of the redox-sensitive transcription factors Nrf2 and NF-κB. Free Radical Biol Med 53(7):1421–1430
Chen Z, Zhong C (2014) Oxidative stress in Alzheimer’s disease. Neurosci Bull 30(2):271–281. https://doi.org/10.1007/s12264-013-1423-y
Chen N, Chiu PY, Ko KM (2008) Schisandrin B enhances cerebral mitochondrial antioxidant status and structural integrity, and protects against cerebral ischemia/reperfusion injury in rats. Biol Pharm Bull 31(7):1387–1391
Chen Y-H, Lin F-Y, Liu P-L, Huang Y-T, Chiu J-H, Chang Y-C et al (2009) Antioxidative and hepatoprotective effects of magnolol on acetaminophen-induced liver damage in rats. Arch Pharmacal Res 32(2):221–228
Chen Q, Zhang H, Cao Y, Li Y, Sun S, Zhang J et al (2017) Schisandrin B attenuates CCl4-induced liver fibrosis in rats by regulation of Nrf2-ARE and TGF-β/Smad signaling pathways. Drug Des Dev Ther 11:2179
Chen Y, Kong Y, Wang Q, Chen J, Chen H, Xie H et al (2021) Schisandrin B attenuates airway inflammation by regulating the NF-κB/Nrf2 signaling pathway in mouse models of asthma. J Immunol Res 2021:8029963
Chirdchupunseree H, Pramyothin P (2010) Protective activity of phyllanthin in ethanol-treated primary culture of rat hepatocytes. J Ethnopharmacol 128(1):172–176
Chiu PY, Luk KF, Leung HY, Ng KM, Ko KM (2008) Schisandrin B stereoisomers protect against hypoxia/reoxygenation-induced apoptosis and inhibit associated changes in Ca2+-induced mitochondrial permeability transition and mitochondrial membrane potential in H9c2 cardiomyocytes. Life Sci 82(21–22):1092–1101
Chiu PY, Chen N, Leong PK, Leung HY, Ko KM (2011) Schisandrin B elicits a glutathione antioxidant response and protects against apoptosis via the redox-sensitive ERK/Nrf2 pathway in H9c2 cells. Mol Cell Biochem 350(1):237–250
Choi SW, Park KI, Yeon JT, Ryu BJ, Kim KJ, Kim SH (2014) Anti-osteoclastogenic activity of matairesinol via suppression of p38/ERK-NFATc1 signaling axis. BMC Complement Altern Med 14:35. https://doi.org/10.1186/1472-6882-14-35
Chu P-Y, Chien S-P, Hsu D-Z, Liu M-Y (2010) Protective effect of sesamol on the pulmonary inflammatory response and lung injury in endotoxemic rats. Food Chem Toxicol 48(7):1821–1826
Chun JN, Kim S-Y, Park E-J, Kwon EJ, Bae D-J, Kim I-S et al (2014) Schisandrin B suppresses TGFβ1-induced stress fiber formation by inhibiting myosin light chain phosphorylation. J Ethnopharmacol 152(2):364–371
Consoli V, Sorrenti V, Grosso S, Vanella L (2021) Heme Oxygenase-1 Signaling and Redox Homeostasis in Physiopathological Conditions. Biomolecules 11(4). https://doi.org/10.3390/biom11040589
Côrtes C, Palin MF, Gagnon N, Benchaar C, Lacasse P, Petit HV (2012) Mammary gene expression and activity of antioxidant enzymes and concentration of the mammalian lignan enterolactone in milk and plasma of dairy cows fed flax lignans and infused with flax oil in the abomasum. Br J Nutr 108(8):1390–1398. https://doi.org/10.1017/s0007114511006829
Coulman KD, Liu Z, Hum WQ, Michaelides J, Thompson LU (2005) Whole sesame seed is as rich a source of mammalian lignan precursors as whole flaxseed. Nutr Cancer 52(2):156–165
Cousins KR (2011) Computer Review of ChemDraw Ultra 12.0. J Am Chem Soc 133(21):8388–8388. https://doi.org/10.1021/ja204075s
Cuadrado A, Manda G, Hassan A, Alcaraz MJ, Barbas C, Daiber A et al (2018) Transcription factor NRF2 as a therapeutic target for chronic diseases: a systems medicine approach. Pharmacol Rev 70(2):348–383
Cuadrado A, Rojo AI, Wells G, Hayes JD, Cousin SP, Rumsey WL et al (2019) Therapeutic targeting of the NRF2 and KEAP1 partnership in chronic diseases. Nat Rev Drug Discovery 18(4):295–317
Dabrosin C, Chen J, Wang L, Thompson LU (2002) Flaxseed inhibits metastasis and decreases extracellular vascular endothelial growth factor in human breast cancer xenografts. Cancer Lett 185(1):31–37
Dai JM, Guo WN, Tan YZ, Niu KW, Zhang JJ, Liu CL et al (2021) Wogonin alleviates liver injury in sepsis through Nrf2-mediated NF-κB signalling suppression. J Cell Mol Med 25(12):5782–5798. https://doi.org/10.1111/jcmm.16604
Dallakyan S, Olson AJ (2015) Small-molecule library screening by docking with PyRx. Chemical biology: methods and protocols, pp 243–250
Ding M, Shu P, Gao S, Wang F, Gao Y, Chen Y et al (2018) Schisandrin B protects human keratinocyte-derived HaCaT cells from tert-butyl hydroperoxide-induced oxidative damage through activating the Nrf2 signaling pathway. Int J Mol Med 42(6):3571–3581
Do HL, Kim DH, Oh IY, Kim SY, Lim YY, Kim HM et al (2013) Inhibitory effects of Saururi chinensis extracts on melanin biosynthesis in B16F10 melanoma cells. Biol Pharm Bull 36(5):772–779
Dong Q, Hou H, Wu J, Chen Y (2016) The N rf2-ARE pathway is associated with S chisandrin b attenuating benzo (a) pyrene-Induced HTR cells damages in vitro. Environ Toxicol 31(11):1439–1449
During A, Debouche C, Raas T, Larondelle Y (2012) Among plant lignans, pinoresinol has the strongest antiinflammatory properties in human intestinal Caco-2 cells. J Nutr 142(10):1798–1805. https://doi.org/10.3945/jn.112.162453
Fan T, Jiang WL, Zhu J, Zhang YF (2012) Arctigenin protects focal cerebral ischemia-reperfusion rats through inhibiting neuroinflammation. Biol Pharm Bull 35(11):2004–2009
Finkel T (2012) Signal transduction by mitochondrial oxidants. J Biol Chem 287(7):4434–4440. https://doi.org/10.1074/jbc.R111.271999
Freigang S, Ampenberger F, Spohn G, Heer S, Shamshiev AT, Kisielow J et al (2011) Nrf2 is essential for cholesterol crystal-induced inflammasome activation and exacerbation of atherosclerosis. Eur J Immunol 41(7):2040–2051. https://doi.org/10.1002/eji.201041316
Freudenberg K, Weinges K (1961) Systematik und nomenklatur der lignane. Tetrahedron 15(1–4):115–128
Fujikawa T, Hirata T, Wada A, Kawamura N, Yamaguchi Y, Fujimura K et al (2010) Chronic administration of Eucommia leaf stimulates metabolic function of rats across several organs. Br J Nutr 104(12):1868–1877. https://doi.org/10.1017/s0007114510002965
Gao Y, Zhao H, Li Y (2018) Sauchinone prevents IL-1β-induced inflammatory response in human chondrocytes. J Biochem Mol Toxicol 32(3):e22033
Giridharan VV, Thandavarayan RA, Arumugam S, Mizuno M, Nawa H, Suzuki K et al (2015) Schisandrin B ameliorates ICV-infused amyloid β induced oxidative stress and neuronal dysfunction through inhibiting RAGE/NF-κB/MAPK and up-regulating HSP/Beclin expression. PLoS ONE 10(11):e0142483
Gloire G, Legrand-Poels S, Piette J (2006) NF-kappaB activation by reactive oxygen species: fifteen years later. Biochem Pharmacol 72(11):1493–1505. https://doi.org/10.1016/j.bcp.2006.04.011
Gong H, Tai H, Huang N, Xiao P, Mo C, Wang X et al (2020) Nrf2-SHP cascade-mediated STAT3 inactivation contributes to AMPK-driven protection against endotoxic inflammation. Front Immunol 11:414. https://doi.org/10.3389/fimmu.2020.00414
González-Vallinas M, González-Castejón M, Rodríguez-Casado A, Ramírez de Molina A (2013) Dietary phytochemicals in cancer prevention and therapy: a complementary approach with promising perspectives. Nutr Rev 71(9):585–599. https://doi.org/10.1111/nure.12051
Gorrini C, Harris IS, Mak TW (2013) Modulation of oxidative stress as an anticancer strategy. Nat Rev Drug Discov 12(12):931–947. https://doi.org/10.1038/nrd4002
Gottlieb O (1972) Chemosystematics of the Lauraceae. Phytochemistry 11(5):1537–1570
Gui Y, Yang Y, Xu D, Tao S, Li J (2020) Schisantherin A attenuates sepsis-induced acute kidney injury by suppressing inflammation via regulating the NRF2 pathway. Life Sci 258:118161
Gulcin I, Kirecci E, Akkemik E, Topal F, Hisar O (2010) Antioxidant, antibacterial, and anticandidal activities of an aquatic plant: duckweed (Lemna minor L. Lemnaceae). Turkish Journal of Biology 34(2):175–188
Hamada N, Tanaka A, Fujita Y, Itoh T, Ono Y, Kitagawa Y et al (2011) Involvement of heme oxygenase-1 induction via Nrf2/ARE activation in protection against H2O2-induced PC12 cell death by a metabolite of sesamin contained in sesame seeds. Bioorg Med Chem 19(6):1959–1965
Han J, Shi X, Zheng Z, Zhang B, Shi F, Jiang L et al (2018) Schisandrin B protects against angiotensin II-induced endotheliocyte deficits by targeting Keap1 and activating Nrf2 pathway. Drug Des Dev Ther 12:3985
Han J, Shi X, Du Y, Shi F, Zhang B, Zheng Z et al (2019) Schisandrin C targets Keap1 and attenuates oxidative stress by activating Nrf2 pathway in Ang II-challenged vascular endothelium. Phytother Res 33(3):779–790
Hancke J, Burgos R, Ahumada F (1999) Schisandra chinensis (Turcz.) baill. Fitoterapia 70(5):451–471
Handy DE, Loscalzo J (2012) Redox regulation of mitochondrial function. Antioxid Redox Signal 16(11):1323–1367. https://doi.org/10.1089/ars.2011.4123
Harikrishnan H, Jantan I, Haque MA, Kumolosasi E (2018) Phyllanthin from Phyllanthus amarus inhibits LPS-induced proinflammatory responses in U937 macrophages via downregulation of NF-κB/MAPK/PI3K-Akt signaling pathways. Phytother Res 32(12):2510–2519. https://doi.org/10.1002/ptr.6190
Haworth R (1942) The chemistry of the lignan group of natural products. J Chem Soc, pp 448–456. https://doi.org/10.1039/jr9420000448
Hayes JD, Dinkova-Kostova AT (2014) The Nrf2 regulatory network provides an interface between redox and intermediary metabolism. Trends Biochem Sci 39(4):199–218
Hibasami H, Fujikawa T, Takeda H, Nishibe S, Satoh T, Fujisawa T et al (2000) Induction of apoptosis by Acanthopanax senticosus HARMS and its component, sesamin in human stomach cancer KATO III cells. Oncol Rep 7(6):1213–1219
Hodges TW, Hossain CF, Kim Y-P, Zhou Y-D, Nagle DG (2004) Molecular-targeted antitumor agents: the Saururus c ernuus dineolignans manassantin B and 4-O-demethylmanassantin B are potent inhibitors of hypoxia-activated HIF-1. J Nat Prod 67(5):767–771
Hoeflich KP, Luo J, Rubie EA, Tsao M-S, Jin O, Woodgett JR (2000) Requirement for glycogen synthase kinase-3β in cell survival and NF-κB activation. Nature 406(6791):86–90
Hoikkala AA, Schiavoni E, Wähälä K (2003) Analysis of phyto-oestrogens in biological matrices. Br J Nutr 89(Suppl 1):S5-18. https://doi.org/10.1079/bjn2002791
Hong H, Lou S, Zheng F, Gao H, Wang N, Tian S et al (2022) Hydnocarpin D attenuates lipopolysaccharide-induced acute lung injury via MAPK/NF-κB and Keap1/Nrf2/HO-1 pathway. Phytomedicine 101:154143. https://doi.org/10.1016/j.phymed.2022.154143
Horn-Ross PL, John EM, Canchola AJ, Stewart SL, Lee MM (2003) Phytoestrogen intake and endometrial cancer risk. J Natl Cancer Inst 95(15):1158–1164. https://doi.org/10.1093/jnci/djg015
Hou T, Yang M, Yan K, Fan X, Ci X, Peng L (2022) Amentoflavone ameliorates carrageenan-induced pleurisy and lung injury by inhibiting the NF-κB/STAT3 pathways via Nrf2 activation. Front Pharmacol 13:763608. https://doi.org/10.3389/fphar.2022.763608
Hu Y, Li Y, Sampson L, Wang M, Manson JE, Rimm E et al (2021) Lignan intake and risk of coronary heart disease. J Am Coll Cardiol 78(7):666–678. https://doi.org/10.1016/j.jacc.2021.05.049
Huang Q, Ouyang DS, Liu Q (2021a) Isoeucommin A attenuates kidney injury in diabetic nephropathy through the Nrf2/HO-1 pathway. FEBS Open Bio 11(8):2350–2363
Huang S, Zhang D, Li Y, Fan H, Liu Y, Huang W et al (2021b) Schisandra sphenanthera: a comprehensive review of its botany, phytochemistry, pharmacology, and clinical applications. Am J Chin Med 49(7):1577–1622. https://doi.org/10.1142/s0192415x21500749
Huyke C, Engel K, Simon-Haarhaus B, Quirin K-W, Schempp CM (2007) Composition and biological activity of different extracts from Schisandra sphenanthera and Schisandra chinensis. Planta Med 73(10):1116–1126
Hybertson BM, Gao B, Bose SK, McCord JM (2011) Oxidative stress in health and disease: the therapeutic potential of Nrf2 activation. Mol Aspects Med 32(4):234–246. https://doi.org/10.1016/j.mam.2011.10.006
Ide T, Ashakumary L, Takahashi Y, Kushiro M, Fukuda N, Sugano M (2001) Sesamin, a sesame lignan, decreases fatty acid synthesis in rat liver accompanying the down-regulation of sterol regulatory element binding protein-1. Biochim Biophys Acta 1534(1):1–13
Imai T, Nomura M, Fukushima K (2006) Evidence for involvement of the phenylpropanoid pathway in the biosynthesis of the norlignan agatharesinol. J Plant Physiol 163(5):483–487. https://doi.org/10.1016/j.jplph.2005.08.009
Ip S-P, Ko K-M (1996a) The crucial antioxidant action of schisandrin B in protecting against carbon tetrachloride hepatotoxicity in mice: a comparative study with butylated hydroxytoluene. Biochem Pharmacol 52(11):1687–1693
Ip SP, Ko KM (1996b) The crucial antioxidant action of schisandrin B in protecting against carbon tetrachloride hepatotoxicity in mice: a comparative study with butylated hydroxytoluene. Biochem Pharmacol 52(11):1687–1693. https://doi.org/10.1016/s0006-2952(96)00517-5
Iwasaki T, Kondo K, Kuroda T, Moritani Y, Yamagata S, Sugiura M et al (1996) Novel selective PDE IV inhibitors as antiasthmatic agents. Synthesis and biological activities of a series of 1-aryl-2,3-bis(hydroxymethyl)naphthalene lignans. J Med Chem 39(14), 2696–704. https://doi.org/10.1021/jm9509096.
Jang WY, Kim MY, Cho JY (2022) Antioxidant, anti-inflammatory, anti-menopausal, and anti-cancer effects of lignans and their metabolites. Int J Mol Sci 23(24). https://doi.org/10.3390/ijms232415482
Jia R, Zhang H, Yang Z, Zhao H, Liu F, Wang H et al (2017) Protective effects of Schisandrin B on cigarette smoke-induced airway injury in mice through Nrf2 pathway. Int Immunopharmacol 53:11–16
Jiang Y-M, Wang Y, Tan H-S, Yu T, Fan X-M, Chen P et al (2016) Schisandrol B protects against acetaminophen-induced acute hepatotoxicity in mice via activation of the NRF2/ARE signaling pathway. Acta Pharmacol Sin 37(3):382–389
Jnoff E, Albrecht C, Barker JJ, Barker O, Beaumont E, Bromidge S et al (2014) Binding mode and structure–activity relationships around direct inhibitors of the Nrf2–Keap1 complex 9(4), 699–705. https://doi.org/10.1002/cmdc.201300525
Jung YW, Lee BM, Ha MT, Tran MH, Kim JA, Lee S et al (2019) Lignans from Saururus chinensis exhibit anti-inflammatory activity by influencing the Nrf2/HO-1 activation pathway. Arch Pharmacal Res 42(4):332–343
Kachur K, Suntres Z (2020) The antibacterial properties of phenolic isomers, carvacrol and thymol. Crit Rev Food Sci Nutr 60(18):3042–3053
Kang KW, Lee SJ, Park JW, Kim SG (2002) Phosphatidylinositol 3-kinase regulates nuclear translocation of NF-E2-related factor 2 through actin rearrangement in response to oxidative stress. Mol Pharmacol 62(5):1001–1010
Kang JS, Lee KH, Han MH, Lee H, Ahn JM, Han SB et al (2008) Antiinflammatory activity of methanol extract isolated from stem bark of Magnolia kobus. Phytother Res 22(7):883–888
Kang Y-J, Park HJ, Chung H-J, Min H-Y, Park EJ, Lee MA et al (2012) Wnt/β-catenin signaling mediates the antitumor activity of magnolol in colorectal cancer cells. Mol Pharmacol 82(2):168–177
Kang JS, Han MH, Kim G-Y, Kim CM, Kim BW, Hwang HJ et al (2014) Nrf2-mediated HO-1 induction contributes to antioxidant capacity of a Schisandrae Fructus ethanol extract in C2C12 myoblasts. Nutrients 6(12):5667–5678
Kanu PJ, Bahsoon JZ, Kanu JB, Kandeh J (2010) Nutraceutical importance of sesame seed and oil: a review of the contribution of their lignans. Sierra Leone J Biomed Res 2(1):4–16
Kaplan I (1942) Condylomata acuminate. New Orleans Med Surg J 94:388–390
Kay HY, Kim YW, Ryu DH, Sung SH, Hwang SJ, Kim SG (2011) Nrf2-mediated liver protection by sauchinone, an antioxidant lignan, from acetaminophen toxicity through the PKCδ-GSK3β pathway. Br J Pharmacol 163(8):1653–1665
Kilkkinen A, Stumpf K, Pietinen P, Valsta LM, Tapanainen H, Adlercreutz H (2001) Determinants of serum enterolactone concentration. Am J Clin Nutr 73(6):1094–1100. https://doi.org/10.1093/ajcn/73.6.1094
Kilkkinen A, Pietinen P, Klaukka T, Virtamo J, Korhonen P, Adlercreutz H (2002) Use of oral antimicrobials decreases serum enterolactone concentration. Am J Epidemiol 155(5):472–477. https://doi.org/10.1093/aje/155.5.472
Kim Y, Hollenbaugh JA, Kim D-H, Kim B (2011) Novel PI3K/Akt inhibitors screened by the cytoprotective function of human immunodeficiency virus type 1 Tat. PLoS ONE 6(7):e21781
Kitts D, Yuan Y, Wijewickreme A, Thompson L (1999) Antioxidant activity of the flaxseed lignan secoisolariciresinol diglycoside and its mammalian lignan metabolites enterodiol and enterolactone. Mol Cell Biochem 202(1):91–100
Kong P, Chen G, Jiang A, Wang Y, Song C, Zhuang J et al (2016) Sesamin inhibits IL-1β-stimulated inflammatory response in human osteoarthritis chondrocytes by activating Nrf2 signaling pathway. Oncotarget 7(50):83720
Köse LP, Gülcin I, Gören AC, Namiesnik J, Martinez-Ayala AL, Gorinstein S (2015) LC–MS/MS analysis, antioxidant and anticholinergic properties of galanga (Alpinia officinarum Hance) rhizomes. Ind Crops Prod 74:712–721
Kou X, Qi S, Dai W, Luo L, Yin Z (2011) Arctigenin inhibits lipopolysaccharide-induced iNOS expression in RAW264. 7 cells through suppressing JAK-STAT signal pathway. Int Immunopharmacol 11(8):1095–1102
Krithika R, Jyothilakshmi V, Prashantha K, Verma RJ (2015) Mechanism of protective effect of phyllanthin against carbon tetrachloride-induced hepatotoxicity and experimental liver fibrosis in mice. Toxicol Mech Methods 25(9):708–717. https://doi.org/10.3109/15376516.2015.1077361
Kwak EJ, Lee YS, Choi EM (2012) Effect of magnolol on the function of osteoblastic MC3T3-E1 cells. Mediat Inflamm 2012:829650
Kwon DH, Cha H-J, Choi EO, Leem S-H, Kim G-Y, Moon S-K et al (2018) Schisandrin A suppresses lipopolysaccharide-induced inflammation and oxidative stress in RAW 264.7 macrophages by suppressing the NF-κB, MAPKs and PI3K/Akt pathways and activating Nrf2/HO-1 signaling. Int J Mol Med 41(1):264–274
Landete J (2012) Plant and mammalian lignans: a review of source, intake, metabolism, intestinal bacteria and health. Food Res Int 46(1):410–424
Lee E, Haa K, Yook JM, Jin MH, Seo CS, Son KH et al (2006) Anti-asthmatic activity of an ethanol extract from Saururus chinensis. Biol Pharm Bull 29(2):211–215
Lei H, Han J, Wang Q, Guo S, Sun H, Zhang X (2012) Effects of sesamin on streptozotocin (STZ)-induced NIT-1 pancreatic β-cell damage. Int J Mol Sci 13(12):16961–16970
Leong PK, Ko KM (2015) Schisandrin B induces an N rf2-mediated thioredoxin expression and suppresses the activation of inflammasome in vitro and in vivo. BioFactors 41(5):314–323
Lewis N, Davin L (1999) Comprehensive natural products chemistry. In: Barton D (ed). Newnes, pp 639–712
Li X, Zhao B, Liu G, Xin W (1990) Scavenging effects on active oxygen radicals by schizandrins with different structures and configurations. Free Radical Biol Med 9(2):99–104
Li W, Khor TO, Xu C, Shen G, Jeong WS, Yu S et al (2008) Activation of Nrf2-antioxidant signaling attenuates NFkappaB-inflammatory response and elicits apoptosis. Biochem Pharmacol 76(11):1485–1489. https://doi.org/10.1016/j.bcp.2008.07.017
Li K, Li Y, Xu B, Mao L, Zhao J (2016) Sesamin inhibits lipopolysaccharide-induced inflammation and extracellular matrix catabolism in rat intervertebral disc. Connect Tissue Res 57(5):347–359. https://doi.org/10.1080/03008207.2016.1182998
Li C, Chen T, Zhou H, Zhang C, Feng Y, Tang F et al (2018) Schisantherin A attenuates neuroinflammation in activated microglia: role of Nrf2 activation through ERK phosphorylation. Cell Physiol Biochem 47(5):1769–1784
Li KM, Dong X, Ma YN, Wu ZH, Yan YM, Cheng YX (2019) Antifungal coumarins and lignans from Artemisia annua. Fitoterapia 134:323–328. https://doi.org/10.1016/j.fitote.2019.02.022
Li M, Jin J, Li J, Guan C-W, Wang W-W, Qiu Y-W et al (2012) Schisandrin B protects against nephrotoxicity induced by cisplatin in HK-2 cells via Nrf2-ARE activation. Yao Xue Xue Bao 47(11):1434–1439
Lin Q, Qin X, Shi M, Qin Z, Meng Y, Qin Z et al (2017) Schisandrin B inhibits LPS-induced inflammatory response in human umbilical vein endothelial cells by activating Nrf2. Int Immunopharmacol 49:142–147
Lin H, Zhang X, Liu J, Yuan L, Liu J, Wang C et al (2021) Schisantherin A improves learning and memory abilities partly through regulating the Nrf2/Keap1/ARE signaling pathway in chronic fatigue mice. Exp Ther Med 21(4):1–9
Liu Z, Zhang B, Liu K, Ding Z, Hu X (2012) Schisandrin B attenuates cancer invasion and metastasis via inhibiting epithelial-mesenchymal transition. PLoS ONE 7(7):e40480
Liu C-M, Chen S-H, Liao Y-W, Yu C-H, Yu C-C, Hsieh P-L (2021) Magnolol ameliorates the accumulation of reactive oxidative stress and inflammation in diabetic periodontitis. J Formos Med Assoc 120(7):1452–1458
Lu S-H, Hsu W-L, Chen T-H, Chou T-C (2015) Activation of Nrf2/HO-1signaling pathway involves the anti-inflammatory activity of magnolol in Porphyromonas gingivalis lipopolysaccharide-stimulated mouse RAW 264.7 macrophages. Int Immunopharmacol 29(2):770–778
Lu H, Liu GT (1992) Anti-oxidant activity of dibenzocyclooctene lignans isolated from Schisandraceae. Planta Med 58(4):311–313. https://doi.org/10.1055/s-2006-961473
Luc K, Schramm-Luc A, Guzik TJ, Mikolajczyk T P (2019) Oxidative stress and inflammatory markers in prediabetes and diabetes. J Physiol Pharmacol 70(6). https://doi.org/10.26402/jpp.2019.6.01
Luo D, Or TC, Yang CL, Lau AS (2014) Anti-inflammatory activity of iridoid and catechol derivatives from Eucommia ulmoides Oliver. ACS Chem Neurosci 5(9):855–866. https://doi.org/10.1021/cn5001205
Luo LF, Wu WH, Zhou YJ, Yan J, Yang GP, Ouyang DS (2010) Antihypertensive effect of Eucommia ulmoides Oliv. extracts in spontaneously hypertensive rats. J Ethnopharmacol 129(2):238–43. https://doi.org/10.1016/j.jep.2010.03.019
Ma Q, Kinneer K, Ye J, Chen BJ (2003) Inhibition of nuclear factor kappaB by phenolic antioxidants: interplay between antioxidant signaling and inflammatory cytokine expression. Mol Pharmacol 64(2):211–219. https://doi.org/10.1124/mol.64.2.211
Ma ZJ, Wang XX, Su G, Yang JJ, Zhu YJ, Wu YW et al (2016) Proteomic analysis of apoptosis induction by lariciresinol in human HepG2 cells. Chem Biol Interact 256:209–219. https://doi.org/10.1016/j.cbi.2016.07.011
Majdalawieh AF, Mansour ZR (2019) Sesamol, a major lignan in sesame seeds (Sesamum indicum): anti-cancer properties and mechanisms of action. Eur J Pharmacol 855:75–89. https://doi.org/10.1016/j.ejphar.2019.05.008
Meister A (1983) Selective modification of glutathione metabolism. Science 220(4596):472–477. https://doi.org/10.1126/science.6836290
Min HJ, Won HY, Kim YC, Sung SH, Byun MR, Hwang JH et al (2009) Suppression of Th2-driven, allergen-induced airway inflammation by sauchinone. Biochem Biophys Res Commun 385(2):204–209. https://doi.org/10.1016/j.bbrc.2009.05.039
Miyawaki T, Aono H, Toyoda-Ono Y, Maeda H, Kiso Y, Moriyama K (2009) Antihypertensive effects of sesamin in humans. J Nutr Sci Vitaminol 55(1):87–91
Mohamed NM, Ahmed MAM, Khan SI, Fronczek FR, Mohammed AF, Ross SA (2022) Anti-inflammatory and cytotoxic specialised metabolites from the leaves of Glandularia × hybrida. Phytochemistry 195:113054. https://doi.org/10.1016/j.phytochem.2021.113054
Moi P, Chan K, Asunis I, Cao A, Kan YW (1994) Isolation of NF-E2-related factor 2 (Nrf2), a NF-E2-like basic leucine zipper transcriptional activator that binds to the tandem NF-E2/AP1 repeat of the beta-globin locus control region. Proc Natl Acad Sci 91(21):9926–9930
Morris GM, Huey R, Lindstrom W, Sanner MF, Belew RK, Goodsell DS et al (2009) AutoDock4 and AutoDockTools4: automated docking with selective receptor flexibility. J Comput Chem 30(16):2785–2791. https://doi.org/10.1002/jcc.21256
Mukker J (2013) Pharmacokinetic and pharmacodynamic studies on flaxseed lignans. University of Saskatchewan Saskatoon, SK, Canada
Murray T, Kang J, Astheimer L, Price WE (2007) Tissue distribution of lignans in rats in response to diet, dose− response, and competition with isoflavones. J Agric Food Chem 55(12):4907–4912
Nagappan A, Jung DY, Kim J-H, Lee H, Jung MH (2018) Gomisin N alleviates ethanol-induced liver injury through ameliorating lipid metabolism and oxidative stress. Int J Mol Sci 19(9):2601
Nakamura Y, Okumura H, Ono Y, Kitagawa Y, Rogi T, Shibata H (2020) Sesame lignans reduce LDL oxidative susceptibility by downregulating the platelet-activating factor acetylhydrolase. Eur Rev Med Pharmacol Sci 24(4), 2151–2161. https://doi.org/10.26355/eurrev_202002_20395.
Nakano Y, Nasu M, Kano M, Kameoka H, Okuyama T, Nishizawa M et al (2017) Lignans from guaiac resin decrease nitric oxide production in interleukin 1β-treated hepatocytes. J Nat Med 71(1):190–197
Namiki M (2007) Nutraceutical functions of sesame: a review. Crit Rev Food Sci Nutr 47(7):651–673. https://doi.org/10.1080/10408390600919114
Nguyen PH, Le TVT, Kang HW, Chae J, Kim SK, Kwon K-I et al (2010) AMP-activated protein kinase (AMPK) activators from Myristica fragrans (nutmeg) and their anti-obesity effect. Bioorg Med Chem Lett 20(14):4128–4131
Ni S, Qian Z, Yuan Y, Li D, Zhong Z, Ghorbani F et al (2020) Schisandrin A restrains osteoclastogenesis by inhibiting reactive oxygen species and activating Nrf2 signalling. Cell Prolif 53(10):e12882
Nowak A, Zakłos-Szyda M, Błasiak J, Nowak A, Zhang Z, Zhang, B (2019) Potential of Schisandra chinensis (Turcz.) Baill. in human health and nutrition: a review of current knowledge and therapeutic perspectives. Nutrients 11(2):333
Numazawa S, Ishikawa M, Yoshida A, Tanaka S, Yoshida T (2003) Atypical protein kinase C mediates activation of NF-E2-related factor 2 in response to oxidative stress. Am J Physiol Cell Physiol 285(2):C334–C342
Oh S-Y, Kim YH, Bae DS, Um BH, Pan C-H, Kim CY et al (2010) Anti-inflammatory effects of gomisin N, gomisin J, and schisandrin C isolated from the fruit of Schisandra chinensis. Biosci Biotechnol Biochem 74(2):285–291
Olajide OA, Ajayi FF, Ekhelar AI, Awe SO, Makinde JM, Alada AA (1999) Biological effects of Myristica fragrans (nutmeg) extract. Phytother Res 13(4):344–345
Pamies D, Martínez CE, Sogorb MA, Vilanova E (2011) Mechanism-based models in reproductive and developmental toxicology. Reproductive and developmental toxicology (pp. 135–146). Elsevier
Pan JY, Chen SL, Yang MH, Wu J, Sinkkonen J, Zou K (2009) An update on lignans: natural products and synthesis. Nat Prod Rep 26(10):1251–1292. https://doi.org/10.1039/b910940d
Panossian A, Wikman G (2008) Pharmacology of Schisandra chinensis Bail.: an overview of Russian research and uses in medicine. J Ethnopharmacol 118(2):183–212
Pathak N, Rai AK, Kumari R, Bhat KV (2014) Value addition in sesame: a perspective on bioactive components for enhancing utility and profitability. Pharmacogn Rev 8(16):147–155. https://doi.org/10.4103/0973-7847.134249
Pharmacopoeia C (2010) ‘Commission. Pharmacopoeia of the People’s Republic of China’. Beijing: China Medical Science Press
Pietrofesa RA, Velalopoulou A, Arguiri E, Menges CW, Testa JR, Hwang WT et al (2016) Flaxseed lignans enriched in secoisolariciresinol diglucoside prevent acute asbestos-induced peritoneal inflammation in mice. Carcinogenesis 37(2):177–187. https://doi.org/10.1093/carcin/bgv174
Qiang Z, Dong H, Xia Y, Chai D, Hu R, Jiang H (2020) Nrf2 and STAT3 alleviates ferroptosis-mediated IIR-ALI by regulating SLC7A11. Oxid Med Cell Longev 2020:5146982. https://doi.org/10.1155/2020/5146982
Rajbhandari I, Takamatsu S, Nagle DG (2001) A new dehydrogeranylgeraniol antioxidant from Saururus c ernuus that inhibits intracellular reactive oxygen species (ROS)-catalyzed oxidation within HL-60 cells. J Nat Prod 64(6):693–695
Ram A, Lauria P, Gupta R, Sharma V (1996) Hypolipidaemic effect of Myristica fragrans fruit extract in rabbits. J Ethnopharmacol 55(1):49–53
Ramos S (2008) Cancer chemoprevention and chemotherapy: dietary polyphenols and signalling pathways. Mol Nutr Food Res 52(5):507–526. https://doi.org/10.1002/mnfr.200700326
Rao AS, Nayanatara A, Anand K, Poojary D, Pai SR (2013) Effect of antibacterial and antifungal activities of Sesamum indicum. World J Pharm Res 2(5):1676–1680
Rauf A, Patel S, Imran M, Maalik A, Arshad MU, Saeed F et al (2018) Honokiol: an anticancer lignan. Biomed Pharmacother 107:555–562. https://doi.org/10.1016/j.biopha.2018.08.054
Ren B, Yuan T, Diao Z, Zhang C, Liu Z, Liu X (2018) Protective effects of sesamol on systemic oxidative stress-induced cognitive impairments via regulation of Nrf2/Keap1 pathway. Food Funct 9(11):5912–5924
Ren J, Su D, Li L, Cai H, Zhang M, Zhai J et al (2020) Anti-inflammatory effects of Aureusidin in LPS-stimulated RAW264.7 macrophages via suppressing NF-κB and activating ROS- and MAPKs-dependent Nrf2/HO-1 signaling pathways. Toxicol Appl Pharmacol 387, 114846. https://doi.org/10.1016/j.taap.2019.114846
Rodríguez-García C, Sánchez-Quesada C, Toledo E, Delgado-Rodríguez M, Gaforio JJ (2019) Naturally lignan-rich foods: a dietary tool for health promotion? Molecules 24(5). https://doi.org/10.3390/molecules24050917
Rothwell JA, Urpi-Sarda M, Boto-Ordoñez M, Llorach R, Farran-Codina A, Barupal DK et al (2016) Systematic analysis of the polyphenol metabolome using the Phenol-Explorer database. Mol Nutr Food Res 60(1):203–211. https://doi.org/10.1002/mnfr.201500435
Salama SA, Mohamadin AM, Abdel-Bakky MS (2021) Arctigenin alleviates cadmium-induced nephrotoxicity: targeting endoplasmic reticulum stress, Nrf2 signaling, and the associated inflammatory response. Life Sci 287:120121
Santini A, Tenore GC, Novellino E (2017) Nutraceuticals: a paradigm of proactive medicine. Eur J Pharm Sci 96:53–61. https://doi.org/10.1016/j.ejps.2016.09.003
Sena LA, Chandel NS (2012) Physiological roles of mitochondrial reactive oxygen species. Mol Cell 48(2):158–167. https://doi.org/10.1016/j.molcel.2012.09.025
Sfakianos J, Coward L, Kirk M, Barnes S (1997a) Intestinal uptake and biliary excretion of the isoflavone genistein in rats. J Nutr 127(7):1260–1268
Sfakianos J, Coward L, Kirk M, Barnes S (1997b) Intestinal uptake and biliary excretion of the isoflavone genistein in rats. J Nutr 127(7):1260–1268. https://doi.org/10.1093/jn/127.7.1260
Shih C-Y, Chou T-C (2012) The antiplatelet activity of magnolol is mediated by PPAR-β/γ. Biochem Pharmacol 84(6):793–803
Sies H, Berndt C, Jones DP (2017) Oxidative stress. Annu Rev Biochem 86:715–748. https://doi.org/10.1146/annurev-biochem-061516-045037
Smeds AI, Eklund PC, Sjöholm RE, Willför SM, Nishibe S, Deyama T et al (2007) Quantification of a broad spectrum of lignans in cereals, oilseeds, and nuts. J Agric Food Chem 55(4):1337–1346. https://doi.org/10.1021/jf0629134
Soares MP, Seldon MP, Gregoire IP, Vassilevskaia T, Berberat PO, Yu J et al (2004) Heme oxygenase-1 modulates the expression of adhesion molecules associated with endothelial cell activation. J Immunol 172(6):3553–3563. https://doi.org/10.4049/jimmunol.172.6.3553
Song H, Kim YC, Moon A (2003) Sauchinone, a lignan from Saururus chinensis, inhibits staurosporine-induced apoptosis in C6 rat glioma cells. Biol Pharm Bull 26(10):1428–1430
Song J-S, Kim E-K, Choi Y-W, Oh WK, Kim Y-M (2016) Hepatocyte-protective effect of nectandrin B, a nutmeg lignan, against oxidative stress: Role of Nrf2 activation through ERK phosphorylation and AMPK-dependent inhibition of GSK-3β. Toxicol Appl Pharmacol 307:138–149
Sporn MB, Liby KT (2012) NRF2 and cancer: the good, the bad and the importance of context. Nat Rev Cancer 12(8):564–571. https://doi.org/10.1038/nrc3278
Sung SH, Kim YC (2000) Hepatoprotective diastereomeric lignans from Saururus chinensis herbs. J Nat Prod 63(7):1019–1021
Suzuki T, Motohashi H, Yamamoto M (2013) Toward clinical application of the Keap1–Nrf2 pathway. Trends Pharmacol Sci 34(6):340–346
Szopa A, Ekiert H (2012) In vitro cultures of Schisandra chinensis (Turcz.) Baill.(Chinese magnolia vine)—a potential biotechnological rich source of therapeutically important phenolic acids. Appl Biochem Biotechnol 166(8):1941–1948
Szopa A, Ekiert R, Ekiert H (2017) Current knowledge of Schisandra chinensis (Turcz.) Baill.(Chinese magnolia vine) as a medicinal plant species: a review on the bioactive components, pharmacological properties, analytical and biotechnological studies. Phytochem Rev16(2):195–218
Taguchi K, Motohashi H, Yamamoto M (2011) Molecular mechanisms of the Keap1–Nrf2 pathway in stress response and cancer evolution. Genes Cells 16(2):123–140. https://doi.org/10.1111/j.1365-2443.2010.01473.x
Tao W, Hu Y, Chen Z, Dai Y, Hu Y, Qi M (2021) Magnolol attenuates depressive-like behaviors by polarizing microglia towards the M2 phenotype through the regulation of Nrf2/HO-1/NLRP3 signaling pathway. Phytomedicine 91:153692
Tebboub O, Cotugno R, Oke-Altuntas F, Bouheroum M, Demirtas Í, D’Ambola M et al (2018). Antioxidant potential of herbal preparations and components from Galactites elegans (All.) Nyman ex Soldano. Evid Based Complement Alternat Med 2018
Teponno RB, Kusari S, Spiteller M (2016) Recent advances in research on lignans and neolignans. Nat Prod Rep 33(9):1044–1092. https://doi.org/10.1039/c6np00021e
Thompson LU, Boucher BA, Liu Z, Cotterchio M, Kreiger N (2006) Phytoestrogen content of foods consumed in Canada, including isoflavones, lignans, and coumestan. Nutr Cancer 54(2):184–201
Tsai Y-C, Cheng P-Y, Kung C-W, Peng Y-J, Ke T-H, Wang J-J et al (2010) Beneficial effects of magnolol in a rodent model of endotoxin shock. Eur J Pharmacol 641(1):67–73
Umezawa T (2003) Diversity in lignan biosynthesis. Phytochem Rev 2(3):371–390
Upadhyay B, Dhaker AK, Kumar A (2010) Ethnomedicinal and ethnopharmaco-statistical studies of Eastern Rajasthan. India J Ethnopharmacol 129(1):64–86
Van Gils C, Cox PA (1994) Ethnobotany of nutmeg in the Spice Islands. J Ethnopharmacol 42(2):117–124
Velentzis LS, Cantwell MM, Cardwell C, Keshtgar MR, Leathem AJ, Woodside JV (2009) Lignans and breast cancer risk in pre- and post-menopausal women: meta-analyses of observational studies. Br J Cancer 100(9):1492–1498. https://doi.org/10.1038/sj.bjc.6605003
Venugopal R, Jaiswal AK (1996) Nrf1 and Nrf2 positively and c-Fos and Fra1 negatively regulate the human antioxidant response element-mediated expression of NAD (P) H: quinone oxidoreductase1 gene. Proc Natl Acad Sci 93(25):14960–14965
Venugopal R, Jaiswal AK (1998) Nrf2 and Nrf1 in association with Jun proteins regulate antioxidant response element-mediated expression and coordinated induction of genes encoding detoxifying enzymes. Oncogene 17(24):3145–3156. https://doi.org/10.1038/sj.onc.1202237
Wang L, Cheng D, Wang H, Di L, Zhou X, Xu T et al (2009) The hepatoprotective and antifibrotic effects of Saururus chinensis against carbon tetrachloride induced hepatic fibrosis in rats. J Ethnopharmacol 126(3):487–491
Wang Q, Jia M, Zhao Y, Hui Y, Pan J, Yu H et al (2019) Supplementation of sesamin alleviates stress-induced behavioral and psychological disorders via reshaping the gut microbiota structure. J Agric Food Chem 67(45):12441–12451. https://doi.org/10.1021/acs.jafc.9b03652
Wang H, Chinnathambi A, Alahmadi TA, Alharbi SA, Veeraraghavan VP, Krishna Mohan S et al (2021a) Phyllanthin inhibits MOLT-4 leukemic cancer cell growth and induces apoptosis through the inhibition of AKT and JNK signaling pathway. J Biochem Mol Toxicol 35(6):1–10. https://doi.org/10.1002/jbt.22758
Wang HQ, Wan Z, Zhang Q, Su T, Yu D, Wang F et al (2022) Schisandrin B targets cannabinoid 2 receptor in Kupffer cell to ameliorate CCl(4)-induced liver fibrosis by suppressing NF-κB and p38 MAPK pathway. Phytomedicine 98:153960. https://doi.org/10.1016/j.phymed.2022.153960
Wang Y, Wen J, Almoiliqy M, Wang Y, Liu Z, Yang X et al (2021b). Sesamin protects against and ameliorates rat intestinal ischemia/reperfusion injury with involvement of activating Nrf2/HO-1/NQO1 signaling pathway. Oxid Med Cell longev 2021
Weeks BS (2009) Formulations of dietary supplements and herbal extracts for relaxation and anxiolytic action: Relarian. Med Sci Monit 15(11):RA256–62.
Wu W, Li Y, Jiao Z, Zhang L, Wang X, Qin R (2019b) Phyllanthin and hypophyllanthin from Phyllanthus amarus ameliorates immune-inflammatory response in ovalbumin-induced asthma: role of IgE, Nrf2, iNOs, TNF-α, and IL’s. Immunopharmacol Immunotoxicol 41(1):55–67
Wu Y, Li Z-C, Yao L-Q, Li M, Tang M (2019d) Schisandrin B alleviates acute oxidative stress via modulation of the Nrf2/Keap1-mediated antioxidant pathway. Appl Physiol Nutr Metab 44(1):1–6
Wu D, Wang XP, Zhang W (2019a) Sesamolin exerts anti-proliferative and apoptotic effect on human colorectal cancer cells via inhibition of JAK2/STAT3 signaling pathway. Cell Mol Biol (Noisy-le-grand) 65(6);96–100
Wu XQ, Li W, Chen JX, Zhai JW, Xu HY, Ni L et al (2019c) Chemical constituents and biological activity profiles on Pleione (Orchidaceae). Molecules 24(17). https://doi.org/10.3390/molecules24173195
Xiao H-H, Lu L, Poon CC-W, Chan C-O, Wang L-J, Zhu Y-X et al (2021) The lignan-rich fraction from Sambucus Williamsii Hance ameliorates dyslipidemia and insulin resistance and modulates gut microbiota composition in ovariectomized rats. Biomed Pharmacother 137:111372
Xu D, Liu J, Ma H, Guo W, Wang J, Kan X et al (2020) Schisandrin A protects against lipopolysaccharide-induced mastitis through activating Nrf2 signaling pathway and inducing autophagy. Int Immunopharmacol 78:105983
Yang T-C, Zhang S-W, Sun L-N, Wang H, Ren A-M (2008) Magnolol attenuates sepsis-induced gastrointestinal dysmotility in rats by modulating inflammatory mediators. World J Gastroenterol: WJG 14(48):7353
Ye W, Li X, Cheng J (2011) Screening of eleven chemical constituents from Radix isatidis for antiviral activity. Afr J Pharm Pharmacol 5(16):1932–1936
You L, Cho JY (2021) The regulatory role of Korean ginseng in skin cells. J Ginseng Res 45(3):363–370. https://doi.org/10.1016/j.jgr.2020.08.004
Yu R, Lei W, Mandlekar S, Weber MJ, Der CJ, Wu J et al (1999) Role of a mitogen-activated protein kinase pathway in the induction of phase II detoxifying enzymes by chemicals. J Biol Chem 274(39):27545–27552
Yu M, Li H, Liu Q, Liu F, Tang L, Li C et al (2011) Nuclear factor p65 interacts with Keap1 to repress the Nrf2-ARE pathway. Cell Signal 23(5):883–892. https://doi.org/10.1016/j.cellsig.2011.01.014
Yuan H, Yang Q, Yang B, Xu H, Nasif O, Muruganantham S et al (2021) Phyllanthin averts oxidative stress and neuroinflammation in cerebral ischemic-reperfusion injury through modulation of the NF-κB and AMPK/Nrf2 pathways. J Environ Pathol Toxicol Oncol 40(1):85–97
Yun YR, Kim MJ, Kwon MJ, Kim HJ, Song YB, Song KB et al (2007) Lipid-lowering effect of hot water-soluble extracts of Saururus chinensis Bail on rats fed high fat diets. J Med Food 10(2):316–322
Yusuf D, Davis AM, Kleywegt GJ, Schmitt S (2008) An alternative method for the evaluation of docking performance: RSR vs RMSD. J Chem Inf Model 48(7):1411–1422. https://doi.org/10.1021/ci800084x
Zeng J, Chen Y, Ding R, Feng L, Fu Z, Yang S et al (2017) Isoliquiritigenin alleviates early brain injury after experimental intracerebral hemorrhage via suppressing ROS- and/or NF-κB-mediated NLRP3 inflammasome activation by promoting Nrf2 antioxidant pathway. J Neuroinflammation 14(1):119. https://doi.org/10.1186/s12974-017-0895-5
Zhang J, Chen J, Liang Z, Zhao C (2014) New lignans and their biological activities. Chem Biodivers 11(1):1–54. https://doi.org/10.1002/cbdv.201100433
Zhang W-Z, Jiang Z-K, He B-X, Liu X-B (2015) Arctigenin protects against lipopolysaccharide-induced pulmonary oxidative stress and inflammation in a mouse model via suppression of MAPK, HO-1, and iNOS signaling. Inflammation 38(4):1406–1414
Zhang W, Wang W, Shen C, Wang X, Pu Z, Yin Q (2021a) Network pharmacology for systematic understanding of Schisandrin B reduces the epithelial cells injury of colitis through regulating pyroptosis by AMPK/Nrf2/NLRP3 inflammasome. Aging (albany NY) 13(19):23193
Zhang Y, Lei Y, Yao X, Yi J, Feng G (2021b) Pinoresinol diglucoside alleviates ischemia/reperfusion-induced brain injury by modulating neuroinflammation and oxidative stress. Chem Biol Drug Des 98(6):986–996
Zheng J, Chen Y, Pat B, Dell’Italia LA, Tillson M, Dillon AR et al (2009) Microarray identifies extensive downregulation of noncollagen extracellular matrix and profibrotic growth factor genes in chronic isolated mitral regurgitation in the dog. Circulation 119(15):2086–2095
Zhou D, He L (2022) Sauchinone inhibits hypoxia-induced invasion and epithelial-mesenchymal transition in osteosarcoma cells via inactivation of the sonic hedgehog pathway. J Recept Signal Transduct Res 42(2):173–179. https://doi.org/10.1080/10799893.2021.1881556
Zhou B, Li J, Liang X, Yang Z, Jiang Z (2017) Transcriptome profiling of influenza A virus-infected lung epithelial (A549) cells with lariciresinol-4-β-D-glucopyranoside treatment. PLoS ONE 12(3):e0173058. https://doi.org/10.1371/journal.pone.0173058
Zhou Y, Liu L, Xiang R, Bu X, Qin G, Dai J et al (2023) Arctigenin mitigates insulin resistance by modulating the IRS2/GLUT4 pathway via TLR4 in type 2 diabetes mellitus mice. Int Immunopharmacol 114:109529. https://doi.org/10.1016/j.intimp.2022.109529
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB).
Author information
Authors and Affiliations
Contributions
Conceptulization: E. H and S.R Methodology: M.A., I.I and N. M. Software: I.I and E. A. Validation: E.A and H.A Formal Analysis: I.I and M.B. Investigation: M. A. and N. M. Resources: H. A. and M. B. Data curation: I.I. and S.R. Writing original Draft: M.A. and I.I. Writing, review and editing: H. A. and E. A. Visualization: E .A and H.A. Supervision: E .H and S.R Project administration: E.H. and S.R. The authors confirm that no paper mill and artificial intelligence was used.
Corresponding author
Ethics declarations
Ethical approval
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hassanein, E.H.M., Althagafy, H.S., Baraka, M.A. et al. The promising antioxidant effects of lignans: Nrf2 activation comes into view. Naunyn-Schmiedeberg's Arch Pharmacol (2024). https://doi.org/10.1007/s00210-024-03102-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00210-024-03102-x