Abstract
Statins represent the cornerstone of pharmacotherapy for the prevention of atherosclerotic cardiovascular disease. These medications not only reduce low-density lipoprotein cholesterol (LDL-C) via inhibition of 3-hydroxy-3-methylglutarate attached to CoA reductase, the key rate-limiting step in the cholesterol biosynthetic pathway, but also upregulate expression of the low-density lipoprotein receptor, improving serum clearance. Given LDL-C is a causal risk factor for the development of atherosclerosis, these complementary mechanisms largely explain why statin therapy leads to reductions in major adverse cardiovascular events. However, decades of basic and clinical research have suggested that statins may exert other effects independent of LDL-C lowering, termed pleiotropic effects, which have become a topic of debate among the scientific community. While some literature suggests statins may improve plaque stability, reduce inflammation and thrombosis, decrease oxidative stress, and improve endothelial function and vascular tone, other studies have suggested potential harmful pleiotropic effects related to increased risk of muscle-related side effects, diabetes, hemorrhagic stroke, and cognitive decline. Furthermore, the introduction of newer, non-statin LDL-C lowering therapies, including ezetimibe, proprotein convertase subtilisin/Kexin Type 9, and bempedoic acid, have challenged the statin pleiotropy theory. This review aims to provide a historical background on the development of statins, explore the mechanistic underpinnings of statin pleiotropy, review the available literature, and provide up to date examples that suggest statins may exert effects outside of LDL-C lowering and the cardiovascular system.
Similar content being viewed by others
Introduction
Atherosclerotic cardiovascular disease (ASCVD) is the leading cause of death and disability in the United States, regardless of sex and race/ethnicity (Arnett et al. 2019; Tsao et al. 2022). However, tremendous advances in our understanding and management of atherosclerosis over the prior decades have led to significant improvements in morbidity and mortality from cardiovascular disease, with death rates from ASCVD declining since the early 1980s largely due to risk factor control and implementation of low-density lipoprotein cholesterol (LDL-C) lowering statin therapy (Tsao et al. 2022). However, data from several large studies have uncovered other potential beneficial cardiovascular aspects independent of LDL-C lowering, referred to as statin ‘pleiotropic’ effects. The purpose of this document is to explore potential pleiotropic effects of statin therapy in the context of the present literature.
Atherogenesis and the fatty streak
The accumulation of atherogenic lipoproteins into the arterial wall initiates a series of specific cell reactions resulting in atherosclerosis. When triggered, activated endothelial cells that line the arterial lumen guide the recruitment of blood leukocytes. When exposed to an atherogenic environment, endothelial cells express leukocyte adhesion molecules and chemokines that facilitate the attachment of monocytes and lymphocytes to the intimal surface. Mononuclear phagocytes can multiply at the site of lesion initiation, and engulf lipids to become foam cells, the trademark of atherosclerotic lesions (Libby 2021). This leads to an inflammatory cascade inducing smooth muscle proliferation and migration into the intima, forming the earliest stages of atherosclerotic plaque, which constitutes a Type I lesion (Stary et al. 1994).
Type II lesions consist of layers of lipid-laden foam cells and smooth muscle cells that aggregate forming the first grossly visible sign of atherosclerosis, the fatty streak (Stary et al. 1994). Evidence of aortic fatty streaks dates back to World War I and the Korean War, uncovered from autopsy studies of young men that died in the field. These observations stimulated the medical community and prompted our understanding that atherosclerosis begins in childhood (Berenson et al. 1998; Mönckeberg 1915). The revolutionary Bogalusa Heart Study, which assessed young individuals 2–39 years of age that had an autopsy, found that all individuals studied had evidence of fatty streaks in the aorta, and half of children 2–15 years of age had fatty streaks in their coronary arteries (Berenson et al. 1998).
Total and LDL-cholesterol
The relationship between cholesterol and heart disease was proposed as early as 1938, when Norwegian physician Carl Muller described families with high plasma cholesterol levels that were transmitted in an autosomal dominant fashion, leading to early cardiovascular disease and death (Müller 1938). This disease was named familial hypercholesterolemia (FH). These individuals carried a 20-fold increase in heart attack risk by middle age. Then, in 1951, cardiologists from Massachusetts General Hospital made the observation that heart attacks were more common among individuals with high blood cholesterol, among other now well regarded risk factors (Gertler et al. 1951). A few years later, Ancel Keys launched one of the earliest large epidemiological cohorts called the Seven Countries Study, which demonstrated that serum cholesterol increased in proportion to total dietary fat intake and saturated fatty acid intake, and that heart attack incidence was associated with serum cholesterol levels in a linear fashion (Feinleib 1981; Goldstein and Brown 2015). This concept was then cemented in the landmark Framingham Heart Study, which firmly established the relationship between high serum cholesterol and incident coronary heart disease (Kannel et al. 1961).
The invention of the ultracentrifuge ignited the era of LDL-C, when John Gofman utilized this technology in 1955 to separate lipoproteins according to density (Gofman et al. 2007). LDL-C and high-density lipoprotein cholesterol (HDL-C) were identified, and Gofman went on to discover that heart attacks were more common among individuals with high LDL-C, and less common among individuals with high HDL-C.
Cholesterol biosynthesis and statin therapy
Once the connection between LDL-C and ASCVD was solidified in the 1950s, an intense effort was undertaken by a group of biochemists to understand cholesterol biosynthesis. The identification of the 6-carbon compound 3-hydroxy-3-methylglutarate attached to CoA (HMG CoA) as an important compound committed entirely to the synthesis of cholesterol and other isoprenoids led to the discovery of HMG CoA reductase as the rate-limiting step in the cholesterol pathway (Bucher et al. 1960). Then, in 1972, Michael Brown and Joseph Goldstein began to study mediators of the synthetic cholesterol pathway after meeting young siblings found to have homozygous familial hypercholesterolemia (FH) (Goldstein and Brown 2015). They obtained skin biopsies from patients with homozygous FH and controls and cultured fibroblasts to better understand how these cells utilize cholesterol to maintain the integrity of their cell membranes. In the controls, they discovered that cholesterol was obtained from two sources: endogenous synthesis from the aforementioned biosynthetic pathway, and from receptor mediated uptake and lysosomal hydrolysis of LDL particles. Additionally, these two processes worked in harmony. When cellular levels of cholesterol were high, LDL receptors and HMG CoA reductase levels decreased. When cholesterol levels were low, LDL receptors and HMG CoA reductase levels increased (Brown and Goldstein 1986). This was in sharp contrast to the fibroblasts cultured from homozygous FH patients, which were found to have defective LDL receptors and HMG CoA reductase activity 100-fold above normal (Goldstein and Brown 1973).
Akira Endo, a Japanese biochemist working at the Sankyo Company in Tokyo, was the first to identify an inhibitor of HMG CoA reductase. This compound, named compactin, was isolated from Penicillium citrinum mold, and is widely regarded as the first statin (Endo 2010). Soon afterwards, Alfred Alberts and colleagues discovered mevinolin (later named Mevacor or lovastatin) (Alberts et al. 1980), another fungal HMG CoA reductase inhibitor, which was shown to increase LDL receptor activity and decrease plasma LDL in dogs treated with this compound (Kovanen et al. 1981). Human studies demonstrating similar LDL-C lowering followed (Vega and Grundy 1991), which led to the commercialization of the first statin approved for human use in 1987, lovastatin, produced by Merck. Finally, in 1994, Merck’s second-generation statin, simvastatin, was studied in the Scandinavian Simvastatin Survival Study (4S), which established that this medication reduced heart attacks and prolonged life in a population at high risk of ASCVD, when compared with placebo (Group 1994).
Randomized control trial evidence for statin pleiotropy
Several randomized-controlled trials have offered credence to the statin pleiotropy hypothesis, as summarized in Table 1. As mentioned, the 4S program was one of the first large trials to demonstrate a linear relationship between LDL-C reduction and cardiovascular event rates (Group 1994) This relationship was further promoted in the Cholesterol Treatment Trialists meta-analysis, which suggests that a 1 mmol/L reduction in LDL-C (roughly equivalent to 39 mg/dL) is associated with a 21% decrease in 5-year incidence of major adverse cardiovascular events (Baigent et al. 2005). Several other large studies, including cholesterol and recurrent events (CARE) (Sacks et al. 1996), heart progression study (HPS) (Heart Protection Study Collaborative Group 2002), long-term intervention with pravastatin in ischemic disease (LIPID) (Tonkin et al. 1998), and treating to new targets (TNT) (LaRosa et al. 2005), helped firmly establish the widely held notion that the magnitude of clinical benefit observed with statin therapy is proportional to the absolute reduction in LDL-C.
The mechanistic properties of statin therapy may not exclusively explain the outcomes observed in many large randomized-controlled trials. For example, a meta-analysis of 33 trials demonstrated that several non-statin therapies that increase LDL receptor activity have similar LDL-C lowering and cardiovascular benefits when compared with statins (Silverman et al. 2016). Trials with non-statin therapies often require more time to derive cardiovascular benefits. While the time to benefit is largely within 5 years for the majority of statin trials, the lipid research clinic-coronary primary prevention trial (LRC-CPPT; cholestyramine), (The Lipid Metabolism-Atherosclerosis Brach NHLBI 1984) program on the surgical control of hyperlipidemias (POSCH; partial ileal loop bypass surgery) (Buchwald et al. 1990), and ezetimibe added to statin therapy after acute coronary syndromes (IMPROVE-IT; ezetimibe in addition to simvastatin) trial (Cannon et al. 2015) demonstrated benefit within 7.4, 9.7, and 7.0 years, respectively. In fact, the Myocardial Ischemia Reduction with Aggressive Cholesterol Lowering (MIRACL) study demonstrated measurable clinical benefit at 16 weeks (Schwartz et al. 2001), while the Pravastatin or Atorvastatin Evaluation and Infection Therapy–Thrombolysis in Myocardial Infarction 22 (PROVE IT–TIMI 22) trial (Cannon et al. 2004) demonstrated benefit at 30 days. This rapid time to cardiovascular benefit may not be fully explained by the LDL-C lowering properties of statin therapy.
Further pleiotropic effects may be mediated by changes in inflammation of the cardiovascular system. A large body of clinical research indicates that inflammation is a fundamental component of atherogenesis and development of ischemic cardiovascular disease (Libby and Hansson 2019). The inflammatory cytokine C-reactive protein (CRP) is a sensitive biomarker of risk for CVD (Ridker et al. 2018), now serving as a risk enhancer in American College of Cardiology/American Heart Association (ACC/AHA) guidelines (Grundy et al. 2018), and can be modulated by statin therapy. In the Pravastatin Inflammation/CRP Evaluation (PRINCE) trial, pravastatin lowered CRP at 12 and 24 weeks from drug initiation, in a largely LDL-C independent fashion (Albert et al. 2001). These results were consistent with data from the CARE trial (Ridker et al. 1998), and MIRACL trial (Schwartz et al. 2001), which used atorvastatin. Then, the rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein (CRP) (JUPITER) trial found that rosuvastatin reduced LDL-C and high-sensitivity CRP by 50% and 37%, respectively (Ridker et al. 2008). This translated to significant reductions in the primary composite cardiovascular endpoint and all cause-mortality, despite baseline LDL-C levels that were relatively well controlled (mean LDL-C 108 mg/dL in both rosuvastatin and placebo arms) (Ridker et al. 2008). Other large randomized-controlled trials have been undertaken to understand if targeted anti-inflammatory medications reduce CVD, with mixed results. While the Canakinumab Anti-inflammatory Thrombosis Outcome Study (CANTOS) (Ridker et al. 2017), Low-Dose Colchicine (LoDoCo) trial (Nidorf et al. 2020), and Colchicine Cardiovascular Outcomes (COLCOT) Trial (Tardif et al. 2019) demonstrated reductions in cardiovascular outcomes, the Cardiovascular Inflammation Reduction Trial (CIRT) failed to reduce cardiovascular events among patients treated with methotrexate (Ridker et al. 2019). While some postulate that CIRT was a negative trial, because it failed to show a reduction in CRP, Mendelian randomization studies have shown that CRP may not be a causal factor in the development of CVD (Collaboration et al. 2011). These disparate findings highlight the lack of clarity that remains on the complex relationship between statin therapy, CRP, inflammation, and ASCVD.
Several of the aforementioned large randomized-controlled trials also found that statins reduce the primary incidence of stroke (2002; Group 1994; LaRosa et al. 2005; Sacks et al. 1996), suggesting pleiotropic effects beyond coronary heart disease. This is particularly noteworthy given data from observational studies have not shown an association between LDL-C and stroke (Bots et al. 2002; Leppälä et al. 1999; Shahar et al. 2003). The Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL) trial confirmed this relationship in a secondary prevention of stroke population, which demonstrated a 16% reduction in stroke among patients in the atorvastatin arm (Amarenco et al. 2006).
Furthermore, evidence from the Atorvastatin for Reduction of MYocardial Dysrhythmia After cardiac surgery (ARMYDA-3) clinical trial showed that treatment with atorvastatin initiated 7 days prior to surgery lowers the risk of post-operative atrial fibrillation, and subsequently shortens hospital stay when compared with placebo (Patti et al. 2006). However, these results were not substantiated in the Statin Therapy in Cardiac Surgery (STICS) trial, which demonstrated that patients taking perioperative statin therapy did not prevent post-operative atrial fibrillation among those undergoing elective surgery (Zheng et al. 2016). Given these disparate results, one cannot conclude with certainty that statins are beneficial in preventing atrial fibrillation after cardiac surgery, though we cannot exclude the possibility of statin pleiotropy either. Thus, further investigation is warranted.
Possible mechanisms of statin pleiotropy
Given the multitude of clinical trials that suggested health benefits of statins beyond LDL-C lowering, scientists have sought to better understand the mechanistic underpinnings to better explain trial results (Fig. 1).
Improved endothelial function and vascular tone
Endothelial injury, which can occur in the setting of hypercholesterolemia, constitutes one of the earliest step in the development of atherosclerotic cardiovascular disease. When the endothelium is injured and becomes dysfunctional, endothelium-derived nitric oxide (NO) is released, which mediates not only vasodilation, but also inhibits leukocyte adhesion and platelet aggregation, and decreases vascular smooth muscle proliferation (Janssens et al. 1998). Thus, NO is protective, and low levels of NO predict an increased risk of cardiovascular events (Liao et al. 1991).
Statins upregulate endothelial NO synthase (eNOS) and therefore increase NO bioavailability, through a variety of mechanisms and pathways (Oesterle and Liao 2019). For example, statins increase eNOS expression by prolonging eNOS mRNA half-life. This is mediated by inhibition of RhoA geranylgeranylation, modification of the cytoskeleton, and localization of the eNOS mRNA (Laufs and Liao 1998). Statins also reduce caveolin-1, an integral membrane protein which binds eNOS inhibiting its ability to NO (Plenz et al. 2004). There is also evidence that statin therapy can activate the phosphatidylinositol 3-kinase (PI3K)/protein kinase Akt pathway (Kureishi et al. 2000), which leads to increased eNOS and plays a role in the regulation of cellular survival, growth, and proliferation (Simoncini et al. 2000).
Statins also modulate the fibrinolytic system of vascular smooth muscle and endothelial cells (Bourcier and Libby 2000). In a rat model, statin therapy increased the expression of tissue-type plasminogen activator and inhibited the expression of PAI-1 (Essig et al. 1998), an endogenous inhibitor of tissue plasminogen activator, mediated in part through the (PI3K)/protein kinase Akt pathway (Mukai et al. 2007). Statins also inhibit the expression of prepro endothelin-1(Hernández-Perera et al. 2000) and reduce endoethelin and angiotensin subtype I receptor expression (Ichiki et al. 2001; Xu et al. 2002). These vasoconstricting agents, which may be elevated in patients with severe atherosclerosis (Lerman et al. 1991), counteract the vasodilation effects of NO and may contribute towards the development of atherosclerotic plaque.
Plaque stabilization
Several clinical trials using intravascular ultrasound (IVUS) technology helped establish the notion that statin therapy, particularly high-intensity statin therapy, may result in plaque stabilization and regression. In the Reversal of Atherosclerosis with Aggressive Lipid-Lowering (REVEAL) trial published in 2004, Nissen et al. showed that patients with coronary heart disease taking 80 mg of atorvastatin had no progression of atheroma volume at 18 months, though patients taking 40 mg of pravastatin showed progression of atherosclerosis (Nissen et al. 2004). Two years later, A Study to Evaluate the Effect of Rosuvastatin on Intravascular Ultrasound-Derived Coronary Atheroma Burden (ASTEROID) showed that 40 mg of rosuvastatin resulted in modest atherosclerotic plaque regression at 24 months of therapy (Nissen et al. 2006). These studies demonstrated the efficacy of high-intensity statin therapy on atheroma volume. Then, in 2011, Nicholls et al. published The Study of Coronary Atheroma by Intravascular Ultrasound: Effect of Rosuvastatin versus Atorvastatin (SATURN) trial, which sought to investigate which high-intensity statin achieved greater plaque stability. After 2 years of therapy, patients taking 40 mg of rosuvastatin had lower LDL-C compared with patients taking 80 mg of atorvastatin (62.6 vs. 70.2 mg/dL, respectively), a similar degree of plaque atheroma regression was observed (Nicholls et al. 2011).
Newer technology, including optical coherence tomography (OCT), has enabled researchers the ability to utilize high resolution imaging for characterization of atherosclerotic plaque. The Effect of Atorvastatin Therapy on Fibrous Cap Thickness in Coronary Atherosclerotic Plaque as Assessed by Optical Coherence Tomography (EASY-FIT) Study utilized OCT to show that atorvastatin 20 mg resulted in a greater increase in fibrous cap thickness compared with atorvastatin 5 mg (Komukai et al. 2014). The Progression of AtheRosclerotic PlAque DetermIned by Computed TomoGraphic Angiography Imaging (PARADIGM) study used a non-invasive imaging technique, coronary computed tomography angiography, to demonstrate that individuals on statins had a slower rate of percent atheroma volume progression, increased plaque calcification, and reductions in other high-risk plaque features when compared with statin-naïve patients. Importantly, despite increases in calcification, there was no increase in stenosis severity among patients on statin therapy (Lee et al. 2018).
Anti-inflammatory
In addition to the clinical trial evidence suggesting a possible CRP mediated anti-inflammatory role on the relationship between statins and CVD, observations also align with in vitro and basic science evidence as well. In one study, simvastatin, atorvastatin, and lovastatin were shown to downregulate nuclear factor-kappa B (NF-kappaB), activator protein-1, and hypoxia-inducible factor-1alpha in endothelial and arterial smooth muscle cells, which play a role in downstream activity of pro-inflammatory cytokines, chemokines, adhesion molecules, and growth factors (Dichtl et al. 2003).
Statins also may play a role in the regulation of T-cell phenotype by blunting pro-inflammatory IL-17 helper T-cell differentiation (Kagami et al. 2009), and promoting the expression of FoxP3 regulatory T cells that induce immune tolerance (Kagami et al. 2009). Antigen presenting cells express major histocompatibility complex II, which is propagated in the presence of interferon-γ. Statins have been shown to reduce the expression of major histocompatibility complex II on antigen presenting cells, ultimately leading to decreased activation of T cells (Kavalipati et al. 2015). Moreover, statins also can bind to an allosteric site within β2-integrin function-associated antigen-1 protein, leading to its inhibition, which then decreases lymphocyte adhesion and impairs T-cell co-stimulation (Weitz-Schmidt et al. 2001).
Anti-thrombotic
During an acute coronary syndrome, intracoronary plaque ruptures leading to platelet aggregation and partial or complete occlusion of the artery, which then leads to ischemia and acute myocardial infarction. Interestingly, hypercholesterolemia is associated with increased platelet reactivity (Opper et al. 1995), potentially mediated by increases in platelet cytosolic calcium (Le Quan Sang et al. 1995), platelet α2-adrenergic receptor density (Baldassarre et al. 1997), and thromboxane A2 biosynthesis (Notarbartolo et al. 1995). Therefore, lowering LDL-C via statin therapy may lessen these pro-thrombotic characteristics.
In mice, atorvastatin therapy led to a reduction in platelet factor 4 and β-thromboglobulin, which are upregulated in states of platelet reactivity (Kaplan and Owen 1981; Laufs et al. 2000). Studies of fluvastatin, acting through PPARα and PPAR-γ, have demonstrated reduced platelet aggregation when compared with colestimide (Ali et al. 2009; Haramaki et al. 2007). Similarly, atorvastatin acutely decreases Nox2, Rac1, platelet phospholipase A2, protein kinase C, thromboxane A2, while increasing nitric oxide levels (Pignatelli et al. 2012). Another study utilizing several different statins demonstrated augmentation of Kruppel-like factor 2 activity, promotion of thrombomodulin expression, and enhancement of the protein C anticoagulation pathway (Sen-Banerjee et al. 2005).
These effects were corroborated clinically in observational studies and randomized-controlled trials. In the Heart and Estrogen/progestin Replacement Study, the risks for thromboembolic events were decreased by 50% among participants taking statins (Grady et al. 2000). Another study showed that statin use was associated with a 22% relative risk reduction in the risk of deep vein thrombosis (Ray et al. 2001). In the JUPITER trial, patients taking rosuvastatin experienced less thromboembolism compared with the control group (Glynn et al. 2009). Given hypercholesterolemia is not a particularly strong risk factor for venous thromboembolism, it remains unlikely this outcome was driven by LDL-C reduction alone (Oesterle et al. 2017).
Decreased oxidative stress
Oxidation of LDL particles in the vascular endothelium constitute one of the key initial drivers of atherosclerotic plaque formation. Both in vitro and ex vivo evidence suggests that statins have direct antioxidant properties (Aviram et al. 1998a; Suzumura et al. 1999). Atorvastatin hydroxy-metabolites, for example, inhibit oxidation of LDL, HDL, and VLDL particles, which suggests an antioxidant effect may also contribute to halt progression of atherosclerosis, independent of LDL-C lowering (Aviram et al. 1998b). These metabolites, which represent roughly 70% of active atorvastatin, accomplish this by scavenging free radicals. Another possible mechanism may be attributable to statins capacity to decrease the ability of macrophages to oxidize lipoproteins (Giroux et al. 1993), via decreasing the activity of macrophage CD36, a receptor for oxidized LDL (Fuhrman et al. 2002).
Additionally, the ability of statins to inhibit the production L-Mevalonate from 3-hydoxy-3-methylglutaryl-CoA in the cholesterol biosynthetic pathway also leads to inhibition of downstream production of Rac1 (Oesterle et al. 2017). This G protein member of the Rho GTPase subfamily activates nicotinamide adenine dinucleotide phosphate (NADPH) oxidase and also mediates the production of reactive oxygen species (ROS) (Takemoto et al. 2001), which can contribute to endothelial dysfunction, inflammation, and oxidation of LDL particles, which all contribute towards the development of atherosclerosis (Miller et al. 2010; Nowak et al. 2017). Irrespective of ROS, statins have demonstrated an ability to attenuate downstream deleterious effects of Rac1 and NADPH oxidase activity which may partially explain how these mediates decrease oxidative stress and inhibit atherosclerosis.
Potential negative non-cardiovascular pleiotropic effects
Statin-associated muscle symptoms
Several off-target, negative side effects have commonly been associated with statin therapy, which also contributes to the notion of statin pleiotropy (Fig. 2). Statin intolerance, a clinical syndrome comprising a variety of statin-associated muscle symptoms (SAMS) and signs pertaining to multiple organ systems, is common and can lead to discontinuation in up to 53% of patients (Lin et al. 2016). The most frequent side effects pertain to skeletal muscle-related symptoms (myalgia) which commonly include muscle aches, soreness, and cramping, though myopathy, myositis, and rhabdomyolysis may also occur in rare cases (Cheeley et al. 2022). The diagnosis of SAMS is subjective; however, organizations like the National Lipid Association have proposed a scoring system based on regional distribution, temporal patterns, and symptoms related to initiation and withdrawal of the medication (Rosenson et al. 2014).
Risk factors for SAMS include female sex, advanced age, lower body mass index, hypothyroidism, vitamin D deficiency, physical disability, and high statin doses (Schech et al. 2007). Roughly 75% of statins are metabolized by the cytochrome P450 (CYP) system in the liver; atorvastatin, simvastatin, and lovastatin use the 3A4 isoenzyme for metabolism (Guengerich 2008). Thus, medications that also use CYP3A4 can increase statin concentrations by competing for catabolism, thereby precipitating SAMS. Grapefruit juice and other tropical juices such as pomegranate and starfruit contain CYP3A4 as well, which may lead to increased systemic statin concentrations (Sorokin et al. 2006). Alternatively, fluvastatin, pitavastatin, and rosuvastatin are metabolized predominantly by CYP2C9, with lesser contributions from CYP3A4 (fluvastatin), CYP2C8 (fluvastatin, pitavastatin), and CYP2C19 (rosuvastatin) (Thompson Paul et al. 2016). Given fewer medications depend on non-CYP3A4 metabolism, there is less risk of drug interactions and subsequent SAMS.
Although the exact pathophysiology SAMS is poorly understood, in vitro studies suggest that reductions in intracellular cholesterol may facilitate cell membrane instability and lysis (Bouitbir et al. 2020). Statins also adversely impact sarcoplasmic reticulum calcium handling (Lotteau et al. 2019), and genetic variants with a missense mutation of leukocyte immunoglobulin-like receptor subfamily B and T521C polymorphism of organic anion transport protein 1B1 can predispose certain individuals to SAMS (Link et al. 2008; Siddiqui et al. 2017). Statin therapy also inhibit the ubiquinone pathway involved in mitochondrial electron transport, thereby decreasing energy production and increasing intracellular levels of reactive oxygen species (Baigent et al. 2010). Interestingly, studies have suggested that supplementation with coenzyme Q10 (i.e., ubiquinone) can reverse mitochondrial dysfunction induced by statins in mice (Muraki et al. 2012). This observation, which has been substantiated in human studies (Qu et al. 2018), led to the notion that coenzyme Q10 may be a viable therapy for SAMS. However, the data have been inconsistent (Banach et al. 2015; Schaefer et al. 2004), and no convincing evidence has emerged on the ability of coenzyme Q10 to mitigate SAMS.
Managing patients with SAMS can be challenging, though several strategies may help facilitate adherence. When symptoms arise, the medication should be stopped until symptom resolution. Measurement of creatinine kinase and liver function tests should be obtained to exclude end organ damage. Patients can then be re-challenged with a lower dose of the same statin, or alternative statins can be trialed. Statins with longer half-lives, such as rosuvastatin, atorvastatin, and pitavastatin, can also be given every other day or less frequently (Keating et al. 2013; Thompson Paul et al. 2016). Data suggest that ≤ 10 mg rosuvastatin given twice weekly reduces LDL-C by 26%. Contributing factors, such as vitamin D deficiency and hypothyroidism, should be excluded and treated, and a thorough medication reconciliation should be done to identify medications with significant statin interactions. Furthermore, it is possible that a considerable proportion of patients that experience SAMS may be due to the “nocebo effect,” a phenomenon in which negative expectations about medicine or a treatment manifest as real symptoms, which is associated with early discontinuation (Nielsen and Nordestgaard 2015). The innovative Self-Assessment Method for Statin Side-effects Or Nocebo (SAMPSON) trial was designed to test the nocebo effect of SAMS among statin users, and found that in participants who had discontinued statin therapy because of side effects, 90% of the symptom burden elicited by the statin was also elicited by placebo. With this knowledge in hand, 50% of participants previously diagnosed with SAMS were able to re-start their statin 6 months after the conclusion of the trial (Howard et al. 2021). Thus, similar strategies could be utilized in clinical practice to mitigate SAMS.
Cognitive impairment and hemorrhagic stroke
In 2012, the US Food and Drug Administration issued a black box warning regarding an association between statin use and cognitive impairment, based on several small studies conducted in the 1990s and early 2000s (Schultz et al. 2018). These side effects may have been driven by the ability of some statins (i.e., lipophilic statins) to cross the blood–brain barrier, leading to the potential for neurotoxicity and cognitive impairment. Additionally, genes encoding cytochrome P450 enzymes, mitochondrial enzymes, and influx and efflux transporters may explain differential cognitive side effects among individuals on statins (Canestaro et al. 2014). Conversely, statins also have been shown to reduce neuro-inflammation and amyloid β in animal models of Alzheimer’s disease, which support the concept that statins may also have beneficial effects on cognitive function.
Despite early concerns, contemporary data from randomized-controlled trials and meta-analyses found no clear, consistent association between statins and cognitive side effects (Adhikari et al. 2021; Giugliano et al. 2017; Zhou et al. 2021). In fact, the Heart and Estrogen/progestin Replacement Study and Cardiovascular Health Study both showed that statin use was associated with a reduction in cognitive decline among older adults (Bernick et al. 2005; Yaffe et al. 2002). Beneficial cognitive effects were also observed in a meta-analysis of 7 observational studies, concluding that statin use not only reduced the risk of cognitive decline, but also Alzheimer’s disease (Etminan et al. 2003; Sparks et al. 2008). Given significant heterogeneity in study results, the 2013 ACC/AHA Cholesterol Guidelines concluded that the evidence suggests no adverse effect on cognitive changes or risk of dementia among individuals on statin therapy (Stone et al. 2014). At present, 2 large ongoing randomized-controlled trials are underway to assess the cognitive effects of statin use, specifically among older adults. The Pragmatic Evaluation of Events and Benefits of Lipid-Lowering in Older Adults (PREVENTABLE) trial aims to enroll 20,000 primary prevention patients ≥ 75 years of age, and will be randomized to atorvastatin 40 mg daily or placebo. The primary outcome is incident dementia and physical disability. The Clinical Trial of Statin Therapy for Reducing Events in the Elderly (STAREE) trial will assess the efficacy of atorvastatin 40 mg versus placebo among 18,000 patients ≥ 70 years of age, and will assess incident death or development of dementia as well as cardiovascular events. These trials should help provide clarity to important questions surrounding the cognitive effects related to statin use among older adults.
Another neurological concern was unearthed from the SPARCL trial, mentioned previously. Despite atorvastatin lowering the incidence of overall stroke and cardiovascular events, there was a small increase in incident hemorrhagic stroke (Amarenco et al. 2006). Some hypothesized that this may have been driven by statin’s antithrombotic, fibrinolytic pleiotropic effects (Violi et al. 2013). However, a study by Ribe et al. used data from a large Danish registry of > 55,000 individuals found no evidence that statins increase the risk of intracerebral hemorrhage over 10 years of follow-up (Ribe et al. 2020). Current ACC/AHA cholesterol guidelines note that this potential side effect is “unfounded” (Grundy et al. 2018).
Diabetes mellitus
Diabetes mellitus is a potent risk factor for the development of ASCVD, such that guidelines suggest at least a moderate intensity statin among individuals 40–75 years of age, regardless of their 10-year ASCVD risk score (Grundy et al. 2018). However, both clinical trial and observational data have suggested a link between statin use and incident diabetes, causing concern among both clinicians and patients. In the JUPITER trial, glycated hemoglobin concentrations were higher among those on rosuvastatin, and a small increase in incident diabetes mellitus was observed (3.0% vs 2.4%, p = 0.01) when compared with placebo (Ridker et al. 2008, 2012). Several other large-scale cardiovascular clinical trials have either demonstrated a null or modest positive association with statin use, with meta-analyses suggesting a statistically significant increased risk (Rajpathak et al. 2009; Sattar et al. 2010a). These relationships appear to be time and dose dependent, with both cumulative dosing and higher potency statins showing stronger relationships (Ko et al. 2019). Additionally, incident diabetes was also more common among those with other risk factors, including overweight and obesity, impaired fasting glucose, and metabolic syndrome (Waters et al. 2011, 2013). Although mechanisms remain unclear, it is possible that individuals already predisposed to diabetes may cross the threshold to overt disease. However, the annual risk of new onset diabetes among those treated with statins is roughly 0.1% (Sattar et al. 2010b), and the absolute risk reduction in major adverse cardiovascular events is roughly 0.42% annually (Cholesterol Treatment Trialists 2012). Therefore, the cardiovascular benefits far outweigh the risk of incident diabetes, and this concern should not be considered a contraindication to statin therapy and should not lead to statin discontinuation (Grundy et al. 2018).
Challenges to the hypothesis: non-statin lipid lowering therapy
Although statins remain first line in reducing LDL-C and cardiovascular events among those at risk, several non-statin lipid lowering agents have become increasing common in clinical care. The IMPROVE-IT trial helped cement the “lower is better” LDL-C hypothesis, which demonstrated that ezetimibe added to simvastatin further reduced major adverse cardiovascular events compared with simvastatin alone (Cannon et al. 2015). Once the efficacy of ezetimibe was established, investigators sought to compare ezetimibe with statins to evaluate if comparable pleiotropic effects could be uncovered. Landmesser et al. showed that simvastatin improves endothelial function independent of LDL-C lowering, though this benefit was not observed among patients treated with ezetimibe (Landmesser et al. 2005). Several other small studies have also documented similar findings (Fichtlscherer et al. 2006; Liu et al. 2009; Matsue et al. 2013). However, results have not been completely uniform. Pesaro et al. showed no difference in markers of inflammation when comparing individuals on ezetimibe/simvastatin vs simvastatin monotherapy (Pesaro et al. 2012). A similar study showed no difference in endothelial function with the addition of ezetimibe to simvastatin (Westerink et al. 2013). While these two studies suggest that non-LDL-C dependent effects can be achieved with ezetimibe, heterogeneous groups with small sample sizes limit interpretability and comparison.
The discovery of proprotein convertase subtilisin/kexin 9 (PCSK9) and its role in cholesterol metabolism have led to the development of 2 monoclonal antibodies directed against this protein, with evidence demonstrating these medications not only reduce LDL-C, but also major adverse cardiovascular events with added to statin therapy (Sabatine et al. 2017; Schwartz et al. 2018). PCSK9 inhibitors are now FDA approved to reduce risk among patients with established ASCVD and familial hypercholesterolemia, when added to a maximally tolerated statin. Interestingly, multiple preclinical studies have uncovered a myriad of potential pleiotropic anti-atherosclerotic effects of PCSK9i. Mounting evidence indicates that PCSK9 inhibition blunts pro-inflammatory pathways, attenuates cholesterol plaque oxidative stress and inflammation, and reduces platelet reactivity possibly decreasing thromboses (Karagiannis et al. 2018). When evaluating effects of PCSK9 inhibitors in larger randomized-controlled clinical outcomes trials, features of statin efficacy including time to benefit, plaque regression, and stroke reduction were comparable with the statin trials (Yu and Liao 2022). Thus, the literature suggests that PCSK9 inhibitors may also exhibit pleiotropic effects via multiple pathways outside of LDL-C lowering.
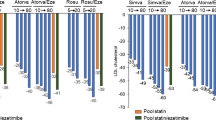
Bempedoic acid is a non-statin LDL-C lowering therapy that targets cholesterol biosynthesis in hepatocytes. While statins inhibits HMG CoA reductase, bempedoic acid inhibits ATP-citrate lyase, which is two step upstream from HMG CoA reductase in the same pathway. Given bempedoic acid is administered as a prodrug that requires activation by enzymes only found in the liver, as opposed to muscle, this medication does not result in increased muscle-related side effects when compared with placebo (Laufs et al. 2019). This medication lowers LDL-C by up to 29% (Ballantyne et al. 2018; Goldberg et al. 2019; Laufs et al. 2019; Ray et al. 2019), and the ongoing Cholesterol Lowering via Bempedoic acid, an ACL-Inhibiting Regimen (CLEAR) Outcomes trial will elucidate whether bempedoic acid results in reductions in major adverse cardiovascular events (Nicholls et al. 2021). Each of the CLEAR series of trials measured the effect of bempedoic acid on high-sensitivity CRP, and evidence from CLEAR Wisdom (Goldberg et al. 2019), Harmony (Ray et al. 2019), Serenity (Laufs et al. 2019), and Tranquility (Ballantyne et al. 2018) all demonstrating significant reductions in this inflammatory marker. Thus, bempedoic may exhibit anti-inflammatory properties, akin to statin therapy which was observed in the JUPITER trial. Furthermore, a pooled analysis of the aforementioned 4 CLEAR trials showed that new onset and worsening diabetes was less frequent among individuals taking bempedoic acid compared with placebo (Bays et al. 2020), which differs from what has previously been observed with statins.
Recent developments in statin pleiotropy
Gut microbiome
Several recent studies have suggested a link between statins and the gut microbiome. In 2020, Vieira-Silva et al. demonstrated that statin therapy modifies microbiome diversification. In this study, a cohort of statin-naive patients with a microbiome enriched with Bacteroides, which is associated with systemic inflammation, was highly prevalent among individuals with obesity and correlates with BMI. Interestingly, matched overweight and obese patients on statin therapy were found to have lower rates of Bacteroides predominant gut microbiomes when compared with their statin-naïve counterparts (Vieira-Silva et al. 2020). This led to the speculation that statin therapy may influence the gut microbiome and counteract a downstream pro-inflammatory environment which can be found in individuals with overweight and obesity. Alternatively, statins anti-inflammatory properties may be exerted on the host, which consequently allows the establishment of a more favorable gut microbiome (Reichel and Knauf 2021). Another study published in 2022 found that LDL-C lowering and insulin resistance differed among statin users with different gut microbiomes, suggesting that responses to statin therapy may, in part, be due to differences in metabolism via the microbiome (Wilmanski et al. 2022).
Preeclampsia
Interesting data have recently emerged on a potential beneficial effect of statins in preventing preeclampsia, an important cause of maternal morbidity and mortality. Preeclampsia and ASCVD share similar risk factors, and both are characterized by inflammation and endothelial dysfunction (Roberts and Redman 1993). Mouse models with overexpression of soluble fms-like tyrosine kinase-1 result in preeclampsia like conditions (Bergmann et al. 2010), and elevations in this protein have been observed in women prior to the clinical development of preeclampsia (Levine et al. 2004, 2006). Importantly, lowering soluble fms-like tyrosine kinase-1 reverses pathological features of preeclampsia (Bergmann et al. 2010), and evidence suggests that statins can inhibit cytokine-mediated release of soluble fms-like tyrosine kinase-1 (Cudmore et al. 2007). To test this hypothesis, Döbert et al. randomized women at high risk of term preeclampsia to pravastatin 20 mg versus placebo, and observed no reduction in the incidence of preeclampsia despite good adherence to the medication. Additionally, there was no significant between-group differences in soluble fms-like tyrosine kinase-1 concentrations (Döbert et al. 2021). Although some have postulated that these negative results may have been due to the low potency or short duration of statin use (Wei et al. 2021), this study suggests that statins may not have pleiotropic beneficial effects among women at risk for preeclampsia.
COVID-19
The coronavirus 2019 (COVID-19) pandemic has ignited a firestorm of research in an attempt to find novel therapies that may mitigate its devastating effects on morbidity and mortality. In severe cases, infection from the severe acute respiratory syndrome coronavirus 2 (SARS-CoV 2) can result in severe acute respiratory distress syndrome (ARDS), due to an exaggerated inflammatory response, which may be fatal (Li and Ma 2020). Furthermore, infection with SARS-CoV 2 can also lead to serious cardiovascular complications (Hansson and Libby 2006), including stroke, venous thromboembolism, myocardial injury, myocarditis, pericarditis, arrhythmias, cardiomyopathy and heart failure, cardiogenic shock, and cardiac arrest (Xie et al. 2022). SARS-CoV 2 binds to angiotensin converting enzyme 2 (ACE2) on the surface of lung cells which mediates entry and subsequent infection (Li et al. 2003; Tai et al. 2020), in addition to serving as a regulatory enzyme in the renin-angiotensin system. Since ACE2 breaks down the pro-inflammatory angiotensin II, it has been postulated that low levels of ACE2 may be associated with at least some of the inflammatory effects induced by SARS-CoV 2 infection (Long et al. 2020). Given statins increase ACE2 levels, some believe that these medications may have a beneficial role in improving outcomes among those with COVID-19. One observational study using data from the AHA’s COVID-19 cardiovascular disease registry found that patients taking a statin prior to hospitalization for COVID-19 had a 16% lower odds of death compared with those not on a statin (Daniels et al. 2021). Several meta-analyses have demonstrated similar benefits among statin users, with literature suggesting reductions in the risk of fatal or severe disease (Kow and Hasan 2020), progression to severe illness or death (Onorato et al. 2021), and reductions in hard clinical outcomes (Scheen 2021). Although these welcome pleiotropic effects from statin use seem to benefit COVID-19-related outcomes, these studies are observational in nature and causality cannot be confirmed. However, ongoing randomized-controlled trials will help further elaborate on the role of statins in SARS-CoV 2 infection (Torres-Peña et al. 2021).
Conclusion
While it is clear that the LDL-C lowering properties of statins largely explain the cardiovascular benefits attributable to this life saving class of medications, decades of basic and clinical research have suggested unique off-target pleiotropic effects not fully explained by their principle mechanism of action. While favorable properties on endothelial function, platelets, vascular smooth muscle, and inflammation have been demonstrated in preclinical studies, these effects have not consistently translated in large-scale randomized-controlled trials, while several non-statin therapies have shown similar off-target effects. Although controversy remains regarding the concept of statin pleiotropy, the cardioprotective effects are unequivocal. Several novel lipid lowering medications in the pipeline will help further elucidate if these non-LDL-C lowering properties are unique to statin therapy.
Data availability
Data sharing not applicable to this article as no datasets were generated during the current study.
References
Adhikari A, Tripathy S, Chuzi S, Peterson J, Stone NJ (2021) Association between statin use and cognitive function: a systematic review of randomized clinical trials and observational studies. J Clin Lipidol 15(1):22-32.e12. https://doi.org/10.1016/j.jacl.2020.10.007
Alberts AW, Chen J, Kuron G et al (1980) Mevinolin: a highly potent competitive inhibitor of hydroxymethylglutaryl-coenzyme A reductase and a cholesterol-lowering agent. Proc Natl Acad Sci USA 77(7):3957–3961. https://doi.org/10.1073/pnas.77.7.3957
Albert MA, Danielson E, Rifai N, Ridker PM, Investigators ftP, (2001) Effect of statin therapy on C-reactive protein levels the pravastatin inflammation/CRP evaluation (PRINCE): a randomized trial and cohort study. JAMA 286(1):64–70. https://doi.org/10.1001/jama.286.1.64
Ali FY, Armstrong PCJ, Dhanji A-RA et al (2009) Antiplatelet actions of statins and fibrates are mediated by PPARs. Arterioscler Thromb Vasc Biol 29(5):706–711. https://doi.org/10.1161/ATVBAHA.108.183160
Amarenco P, Bogousslavsky J, Callahan A 3rd et al (2006) High-dose atorvastatin after stroke or transient ischemic attack. N Engl J Med 355(6):549–559. https://doi.org/10.1056/NEJMoa061894
Arnett DK, Blumenthal RS, Albert MA et al (2019) 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. Circulation 140(11):e596–e646. https://doi.org/10.1161/CIR.0000000000000678
Aviram M, Hussein O, Rosenblat M, Schlezinger S, Hayek T, Keidar S (1998a) Interactions of platelets, macrophages, and lipoproteins in hypercholesterolemia: antiatherogenic effects of HMG-CoA reductase inhibitor therapy. J Cardiovasc Pharmacol 31(1):39–45
Aviram M, Rosenblat M, Bisgaier CL, Newton RS (1998b) Atorvastatin and gemfibrozil metabolites, but not the parent drugs, are potent antioxidants against lipoprotein oxidation. Atherosclerosis 138(2):271–280. https://doi.org/10.1016/S0021-9150(98)00032-X
Baigent C, Keech A, Kearney PM et al (2005) Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet 366(9493):1267–1278. https://doi.org/10.1016/S0140-6736(05)67394-1
Baigent C, Blackwell L, Emberson J et al (2010) Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet 376(9753):1670–1681. https://doi.org/10.1016/s0140-6736(10)61350-5
Baldassarre D, Mores N, Colli S, Pazzucconi F, Sirtori CR, Tremoli E (1997) Platelet alpha 2-adrenergic receptors in hypercholesterolemia: relationship between binding studies and epinephrine-induced platelet aggregation. Clin Pharmacol Ther 61(6):684–691. https://doi.org/10.1016/s0009-9236(97)90104-1
Ballantyne CM, Banach M, Mancini GBJ et al (2018) Efficacy and safety of bempedoic acid added to ezetimibe in statin-intolerant patients with hypercholesterolemia: a randomized, placebo-controlled study. Atherosclerosis 277:195–203. https://doi.org/10.1016/j.atherosclerosis.2018.06.002
Banach M, Serban C, Sahebkar A et al (2015) Effects of coenzyme Q10 on statin-induced myopathy: a meta-analysis of randomized controlled trials. Mayo Clin Proc 90(1):24–34. https://doi.org/10.1016/j.mayocp.2014.08.021
Bays HE, Banach M, Catapano AL et al (2020) Bempedoic acid safety analysis: pooled data from four phase 3 clinical trials. J Clin Lipidol 14(5):649-659.e6. https://doi.org/10.1016/j.jacl.2020.08.009
Berenson GS, Srinivasan SR, Bao W, Newman WP 3rd, Tracy RE, Wattigney WA (1998) Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults. The Bogalusa Heart Study. N Engl J Med 338(23):1650–1656. https://doi.org/10.1056/nejm199806043382302
Bergmann A, Ahmad S, Cudmore M et al (2010) Reduction of circulating soluble Flt-1 alleviates preeclampsia-like symptoms in a mouse model. J Cell Mol Med 14(6b):1857–1867. https://doi.org/10.1111/j.1582-4934.2009.00820.x
Bernick C, Katz R, Smith NL et al (2005) Statins and cognitive function in the elderly. Cardiovasc Health Study 65(9):1388–1394. https://doi.org/10.1212/01.wnl.0000182897.18229.ec
Bots ML, Elwood PC, Nikitin Y et al (2002) Total and HDL cholesterol and risk of stroke. EUROSTROKE: a collaborative study among research centres in Europe. J Epidemiol Community Health 56(Suppl 1):i19-24. https://doi.org/10.1136/jech.56.suppl_1.i19
Bouitbir J, Sanvee GM, Panajatovic MV, Singh F, Krähenbühl S (2020) Mechanisms of statin-associated skeletal muscle-associated symptoms. Pharmacol Res 154:104201. https://doi.org/10.1016/j.phrs.2019.03.010
Bourcier T, Libby P (2000) HMG CoA reductase inhibitors reduce plasminogen activator inhibitor-1 expression by human vascular smooth muscle and endothelial cells. Arterioscler Thromb Vasc Biol 20(2):556–562. https://doi.org/10.1161/01.atv.20.2.556
Brown MS, Goldstein JL (1986) A receptor-mediated pathway for cholesterol homeostasis. Science 232(4746):34–47
Bucher NL, Overath P, Lynen F (1960) beta-Hydroxy-beta-methyl-glutaryl coenzyme A reductase, cleavage and condensing enzymes in relation to cholesterol formation in rat liver. Biochim Biophys Acta 40:491–501. https://doi.org/10.1016/0006-3002(60)91390-1
Buchwald H, Varco RL, Matts JP et al (1990) Effect of partial ileal bypass surgery on mortality and morbidity from coronary heart disease in patients with hypercholesterolemia. N Engl J Med 323(14):946–955. https://doi.org/10.1056/nejm199010043231404
Canestaro WJ, Austin MA, Thummel KE (2014) Genetic factors affecting statin concentrations and subsequent myopathy: a HuGENet systematic review. Genet Med 16(11):810–819. https://doi.org/10.1038/gim.2014.41
Cannon CP, Braunwald E, McCabe CH et al (2004) Intensive versus moderate lipid lowering with statins after acute coronary syndromes. N Engl J Med 350(15):1495–1504. https://doi.org/10.1056/NEJMoa040583
Cannon CP, Blazing MA, Giugliano RP et al (2015) Ezetimibe added to statin therapy after acute coronary syndromes. N Engl J Med 372(25):2387–2397. https://doi.org/10.1056/NEJMoa1410489
Cheeley MK, Saseen JJ, Agarwala A et al (2022) NLA scientific statement on statin intolerance: a new definition and key considerations for ASCVD risk reduction in the statin intolerant patient. J Clin Lipidol. https://doi.org/10.1016/j.jacl.2022.05.068
Cholesterol Treatment Trialists C (2012) The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: meta-analysis of individual data from 27 randomised trials. Lancet 380(9841):581–590. https://doi.org/10.1016/S0140-6736(12)60367-5
Collaboration CRPCHDG, Wensley F, Gao P et al (2011) Association between C reactive protein and coronary heart disease: mendelian randomisation analysis based on individual participant data. BMJ (clin Res Ed) 342:d548–d548. https://doi.org/10.1136/bmj.d548
Cudmore M, Ahmad S, Al-Ani B et al (2007) Negative regulation of soluble Flt-1 and soluble endoglin release by heme oxygenase-1. Circulation 115(13):1789–1797. https://doi.org/10.1161/CIRCULATIONAHA.106.660134
Daniels LB, Ren J, Kumar K et al (2021) Relation of prior statin and anti-hypertensive use to severity of disease among patients hospitalized with COVID-19: findings from the American Heart Association’s COVID-19 Cardiovascular Disease Registry. PLoS ONE 16(7):e0254635. https://doi.org/10.1371/journal.pone.0254635
Dichtl W, Dulak J, Frick M et al (2003) HMG-CoA reductase inhibitors regulate inflammatory transcription factors in human endothelial and vascular smooth muscle cells. Arterioscler Thromb Vasc Biol 23(1):58–63. https://doi.org/10.1161/01.atv.0000043456.48735.20
Döbert M, Varouxaki AN, Mu AC et al (2021) Pravastatin versus placebo in pregnancies at high risk of term preeclampsia. Circulation 144(9):670–679. https://doi.org/10.1161/CIRCULATIONAHA.121.053963
Endo A (2010) A historical perspective on the discovery of statins. Proc Jpn Acad Ser B Phys Biol Sci 86(5):484–493. https://doi.org/10.2183/pjab.86.484
Essig M, Nguyen G, Prié D, Escoubet B, Sraer JD, Friedlander G (1998) 3-Hydroxy-3-methylglutaryl coenzyme A reductase inhibitors increase fibrinolytic activity in rat aortic endothelial cells. Role of geranylgeranylation and Rho proteins. Circ Res 83(7):683–690. https://doi.org/10.1161/01.res.83.7.683
Etminan M, Gill S, Samii A (2003) The role of lipid-lowering drugs in cognitive function: a meta-analysis of observational studies. Pharmacother J Hum Pharmacol Drug Ther 23(6):726–730. https://doi.org/10.1592/phco.23.6.726.32184
Feinleib M (1981) Seven countries: a multivariate analysis of death and coronary heart disease. JAMA 245(5):511–512. https://doi.org/10.1001/jama.1981.03310300063026
Fichtlscherer S, Schmidt-Lucke C, Bojunga S et al (2006) Differential effects of short-term lipid lowering with ezetimibe and statins on endothelial function in patients with CAD: clinical evidence for ‘pleiotropic’ functions of statin therapy. Eur Heart J 27(10):1182–1190. https://doi.org/10.1093/eurheartj/ehi881
Fuhrman B, Koren L, Volkova N, Keidar S, Hayek T, Aviram M (2002) Atorvastatin therapy in hypercholesterolemic patients suppresses cellular uptake of oxidized-LDL by differentiating monocytes. Atherosclerosis 164(1):179–185. https://doi.org/10.1016/S0021-9150(02)00063-1
Gertler MM, Garn SM, White PD (1951) Young candidates for coronary heart disease. J Am Med Assoc 147(7):621–625. https://doi.org/10.1001/jama.1951.03670240005002
Giroux LM, Davignon J, Naruszewicz M (1993) Simvastatin inhibits the oxidation of low-density lipoproteins by activated human monocyte-derived macrophages. Biochim Biophys Acta (BBA) Lipids Lipid Metab 1165(3):335–338. https://doi.org/10.1016/0005-2760(93)90145-Y
Giugliano RP, Pedersen TR, Park JG et al (2017) Clinical efficacy and safety of achieving very low LDL-cholesterol concentrations with the PCSK9 inhibitor evolocumab: a prespecified secondary analysis of the FOURIER trial. Lancet 390(10106):1962–1971. https://doi.org/10.1016/S0140-6736(17)32290-0
Glynn RJ, Danielson E, Fonseca FAH et al (2009) A randomized trial of rosuvastatin in the prevention of venous thromboembolism. N Engl J Med 360(18):1851–1861. https://doi.org/10.1056/NEJMoa0900241
Gofman JW, Delalla O, Glazier F et al (2007) The serum lipoprotein transport system in health, metabolic disorders, atherosclerosis and coronary heart disease. J Clin Lipidol 1(2):104–141. https://doi.org/10.1016/j.jacl.2007.03.001
Goldberg AC, Leiter LA, Stroes ESG et al (2019) Effect of bempedoic acid vs placebo added to maximally tolerated statins on low-density lipoprotein cholesterol in patients at high risk for cardiovascular disease: the CLEAR wisdom randomized clinical trial. JAMA 322(18):1780–1788. https://doi.org/10.1001/jama.2019.16585
Goldstein JL, Brown MS (1973) Familial hypercholesterolemia: identification of a defect in the regulation of 3-hydroxy-3-methylglutaryl coenzyme A reductase activity associated with overproduction of cholesterol. Proc Natl Acad Sci USA 70(10):2804–2808. https://doi.org/10.1073/pnas.70.10.2804
Goldstein JL, Brown MS (2015) A century of cholesterol and coronaries: from plaques to genes to statins. Cell 161(1):161–172. https://doi.org/10.1016/j.cell.2015.01.036
Grady D, Wenger NK, Herrington D et al (2000) Postmenopausal hormone therapy increases risk for venous thromboembolic disease: the heart and estrogen/progestin replacement study. Ann Intern Med 132(9):689–696. https://doi.org/10.7326/0003-4819-132-9-200005020-00002%m10787361
Group SSSS (1994) Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S). Lancet 344(8934):1383–1389
Grundy SM, Stone NJ, Bailey AL et al (2018) 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol. Circulation. https://doi.org/10.1161/cir.0000000000000625
Guengerich FP (2008) Cytochrome P450 and chemical toxicology. Chem Res Toxicol 21(1):70–83. https://doi.org/10.1021/tx700079z
Hansson GK, Libby P (2006) The immune response in atherosclerosis: a double-edged sword. Nat Rev Immunol 6(7):508–519. https://doi.org/10.1038/nri1882
Haramaki N, Ikeda H, Takenaka K et al (2007) Fluvastatin alters platelet aggregability in patients with hypercholesterolemia. Arterioscler Thromb Vasc Biol 27(6):1471–1477. https://doi.org/10.1161/ATVBAHA.106.128793
Heart Protection Study Collaborative Group (2002) MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomised placebo-controlled trial. Lancet 360(9326):7–22. https://doi.org/10.1016/s0140-6736(02)09327-3
Hernández-Perera O, Pérez-Sala D, Soria E, Lamas S (2000) Involvement of Rho GTPases in the transcriptional inhibition of preproendothelin-1 gene expression by simvastatin in vascular endothelial cells. Circ Res 87(7):616–622. https://doi.org/10.1161/01.res.87.7.616
Howard JP, Wood FA, Finegold JA et al (2021) Side effect patterns in a crossover trial of statin, placebo, and no treatment. J Am Coll Cardiol 78(12):1210–1222. https://doi.org/10.1016/j.jacc.2021.07.022
Ichiki T, Takeda K, Tokunou T et al (2001) Downregulation of angiotensin II type 1 receptor by hydrophobic 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitors in vascular smooth muscle cells. Arterioscler Thromb Vasc Biol 21(12):1896–1901. https://doi.org/10.1161/hq1201.099430
Janssens S, Flaherty D, Nong Z et al (1998) Human endothelial nitric oxide synthase gene transfer inhibits vascular smooth muscle cell proliferation and neointima formation after balloon injury in rats. Circulation 97(13):1274–1281. https://doi.org/10.1161/01.cir.97.13.1274
Kagami S, Owada T, Kanari H et al (2009) Protein geranylgeranylation regulates the balance between Th17 cells and Foxp3+ regulatory T cells. Int Immunol 21(6):679–689. https://doi.org/10.1093/intimm/dxp037
Kannel WB, Dawber TR, Kagan A, Revotskie N, Stokes J 3rd (1961) Factors of risk in the development of coronary heart disease—six year follow-up experience. The Framingham Study. Ann Intern Med 55:33–50. https://doi.org/10.7326/0003-4819-55-1-33
Kaplan KL, Owen J (1981) Plasma levels of beta-thromboglobulin and platelet factor 4 as indices of platelet activation in vivo. Blood 57(2):199–202
Karagiannis AD, Liu M, Toth PP et al (2018) Pleiotropic anti-atherosclerotic effects of PCSK9 inhibitors from molecular biology to clinical translation. Curr Atheroscler Rep 20(4):20. https://doi.org/10.1007/s11883-018-0718-x
Kavalipati N, Shah J, Ramakrishan A, Vasnawala H (2015) Pleiotropic effects of statins. Indian J Endocrinol Metab 19(5):554–562. https://doi.org/10.4103/2230-8210.163106
Keating AJ, Campbell KB, Guyton JR (2013) Intermittent nondaily dosing strategies in patients with previous statin-induced myopathy. Ann Pharmacother 47(3):398–404. https://doi.org/10.1345/aph.1R509
Ko MJ, Jo AJ, Kim YJ et al (2019) Time- and dose-dependent association of statin use with risk of clinically relevant new-onset diabetes mellitus in primary prevention: a nationwide observational cohort study. J Am Heart Assoc 8(8):e011320. https://doi.org/10.1161/JAHA.118.011320
Komukai K, Kubo T, Kitabata H et al (2014) Effect of atorvastatin therapy on fibrous cap thickness in coronary atherosclerotic plaque as assessed by optical coherence tomography: the EASY-FIT study. J Am Coll Cardiol 64(21):2207–2217. https://doi.org/10.1016/j.jacc.2014.08.045
Kovanen PT, Bilheimer DW, Goldstein JL, Jaramillo JJ, Brown MS (1981) Regulatory role for hepatic low density lipoprotein receptors in vivo in the dog. Proc Natl Acad Sci USA 78(2):1194–1198. https://doi.org/10.1073/pnas.78.2.1194
Kow CS, Hasan SS (2020) Meta-analysis of effect of statins in patients with COVID-19. Am J Cardiol 134:153–155. https://doi.org/10.1016/j.amjcard.2020.08.004
Kureishi Y, Luo Z, Shiojima I et al (2000) The HMG-CoA reductase inhibitor simvastatin activates the protein kinase Akt and promotes angiogenesis in normocholesterolemic animals. Nat Med 6(9):1004–1010. https://doi.org/10.1038/79510
Landmesser U, Bahlmann F, Mueller M et al (2005) Simvastatin versus ezetimibe. Circulation 111(18):2356–2363. https://doi.org/10.1161/01.CIR.0000164260.82417.3F
LaRosa JC, Grundy SM, Waters DD et al (2005) Intensive lipid lowering with atorvastatin in patients with stable coronary disease. N Engl J Med 352(14):1425–1435. https://doi.org/10.1056/NEJMoa050461
Laufs U, Liao JK (1998) Post-transcriptional regulation of endothelial nitric oxide synthase mRNA stability by Rho GTPase. J Biol Chem 273(37):24266–24271. https://doi.org/10.1074/jbc.273.37.24266
Laufs U, Gertz K, Huang P et al (2000) Atorvastatin upregulates type III nitric oxide synthase in thrombocytes, decreases platelet activation, and protects from cerebral ischemia in normocholesterolemic mice. Stroke 31(10):2442–2449. https://doi.org/10.1161/01.str.31.10.2442
Laufs U, Banach M, Mancini GBJ et al (2019a) Efficacy and safety of bempedoic acid in patients with hypercholesterolemia and statin intolerance. J Am Heart Assoc 8(7):e011662. https://doi.org/10.1161/jaha.118.011662
Lee S-E, Chang H-J, Sung JM et al (2018) Effects of statins on coronary atherosclerotic plaques: the PARADIGM study. JACC Cardiovasc Imaging 11(10):1475–1484. https://doi.org/10.1016/j.jcmg.2018.04.015
Leppälä JM, Virtamo J, Fogelholm R, Albanes D, Heinonen OP (1999) Different risk factors for different stroke subtypes: association of blood pressure, cholesterol, and antioxidants. Stroke 30(12):2535–2540. https://doi.org/10.1161/01.str.30.12.2535
Le-Quan-Sang KH, Levenson J, Megnien JL, Simon A, Devynck MA (1995) Platelet cytosolic Ca2+ and membrane dynamics in patients with primary hypercholesterolemia. Effects of pravastatin. Arterioscler Thromb Vasc Biol 15(6):759–764. https://doi.org/10.1161/01.atv.15.6.759
Lerman A, Edwards BS, Hallett JW, Heublein DM, Sandberg SM, Burnett JC Jr (1991) Circulating and tissue endothelin immunoreactivity in advanced atherosclerosis. N Engl J Med 325(14):997–1001. https://doi.org/10.1056/nejm199110033251404
Levine RJ, Maynard SE, Qian C et al (2004) Circulating angiogenic factors and the risk of preeclampsia. N Engl J Med 350(7):672–683. https://doi.org/10.1056/NEJMoa031884
Levine RJ, Lam C, Qian C et al (2006) Soluble endoglin and other circulating antiangiogenic factors in preeclampsia. N Engl J Med 355(10):992–1005. https://doi.org/10.1056/NEJMoa055352
Li X, Ma X (2020) Acute respiratory failure in COVID-19: is it “typical” ARDS? Crit Care 24(1):198. https://doi.org/10.1186/s13054-020-02911-9
Li W, Moore MJ, Vasilieva N et al (2003) Angiotensin-converting enzyme 2 is a functional receptor for the SARS coronavirus. Nature 426(6965):450–454. https://doi.org/10.1038/nature02145
Liao JK, Bettmann MA, Sandor T, Tucker JI, Coleman SM, Creager MA (1991) Differential impairment of vasodilator responsiveness of peripheral resistance and conduit vessels in humans with atherosclerosis. Circ Res 68(4):1027–1034. https://doi.org/10.1161/01.res.68.4.1027
Libby P (2021) The changing landscape of atherosclerosis. Nature 592(7855):524–533. https://doi.org/10.1038/s41586-021-03392-8
Libby P, Hansson GK (2019) From focal lipid storage to systemic inflammation: JACC review topic of the week. J Am Coll Cardiol 74(12):1594–1607. https://doi.org/10.1016/j.jacc.2019.07.061
Lin I, Sung J, Sanchez RJ et al (2016) Patterns of statin use in a real-world population of patients at high cardiovascular risk. J Manag Care Spec Pharm 22(6):685–698. https://doi.org/10.18553/jmcp.2016.22.6.685
Link E, Parish S, Armitage J et al (2008) SLCO1B1 variants and statin-induced myopathy—a genomewide study. N Engl J Med 359(8):789–799. https://doi.org/10.1056/NEJMoa0801936
Lipid Metabolism-Atherogenesis Brach, NHLBI (1984) The lipid research clinics coronary primary prevention trial results: I. Reduction in incidence of coronary heart disease. JAMA 251(3):351–364
Liu P-Y, Liu Y-W, Lin L-J, Chen J-H, Liao JK (2009) Evidence for statin pleiotropy in humans. Circulation 119(1):131–138. https://doi.org/10.1161/CIRCULATIONAHA.108.813311
Long B, Brady WJ, Koyfman A, Gottlieb M (2020) Cardiovascular complications in COVID-19. Am J Emerg Med 38(7):1504–1507. https://doi.org/10.1016/j.ajem.2020.04.048
Lotteau S, Ivarsson N, Yang Z et al (2019) A mechanism for statin-induced susceptibility to myopathy. JACC Basic Transl Sci 4(4):509–523. https://doi.org/10.1016/j.jacbts.2019.03.012
Matsue Y, Matsumura A, Suzuki M, Hashimoto Y, Yoshida M (2013) Differences in action of atorvastatin and ezetimibe in lowering low-density lipoprotein cholesterol and effect on endothelial function—randomized controlled trial–. Circ J 77(7):1791–1798. https://doi.org/10.1253/circj.CJ-13-0033
Miller YI, Choi S-H, Fang L, Tsimikas S (2010) Lipoprotein modification and macrophage uptake: role of pathologic cholesterol transport in atherogenesis. In: Harris JR (ed) Cholesterol binding and cholesterol transport proteins: structure and function in health and disease. Springer Netherlands, Dordrecht, pp 229–251
Mönckeberg J (1915) Über die Atherosklerose der Kombattanten (nach Obduktionsbefunden). Zentralbl Herz Gefasskrankheiten 7:7–10
Mukai Y, Wang CY, Rikitake Y, Liao JK (2007) Phosphatidylinositol 3-kinase/protein kinase Akt negatively regulates plasminogen activator inhibitor type 1 expression in vascular endothelial cells. Am J Physiol Heart Circ Physiol 292(4):H1937–H1942. https://doi.org/10.1152/ajpheart.00868.2006
Müller C (1938) Xanthomata, hypercholesterolemia, angina pectoris. Acta Med Scand 95(S89):75–84
Muraki A, Miyashita K, Mitsuishi M, Tamaki M, Tanaka K, Itoh H (2012) Coenzyme Q10 reverses mitochondrial dysfunction in atorvastatin-treated mice and increases exercise endurance. J Appl Physiol 113(3):479–486
Nicholls SJ, Ballantyne CM, Barter PJ et al (2011) Effect of two intensive statin regimens on progression of coronary disease. N Engl J Med 365(22):2078–2087. https://doi.org/10.1056/NEJMoa1110874
Nicholls S, Lincoff AM, Bays HE et al (2021) Rationale and design of the CLEAR-outcomes trial: evaluating the effect of bempedoic acid on cardiovascular events in patients with statin intolerance. Am Heart J 235:104–112. https://doi.org/10.1016/j.ahj.2020.10.060
Nidorf SM, Fiolet ATL, Mosterd A et al (2020) Colchicine in patients with chronic coronary disease. N Engl J Med 383(19):1838–1847. https://doi.org/10.1056/NEJMoa2021372
Nielsen SF, Nordestgaard BG (2015) Negative statin-related news stories decrease statin persistence and increase myocardial infarction and cardiovascular mortality: a nationwide prospective cohort study. Eur Heart J 37(11):908–916. https://doi.org/10.1093/eurheartj/ehv641
Nissen SE, Tuzcu EM, Schoenhagen P et al (2004) Effect of intensive compared with moderate lipid-lowering therapy on progression of coronary atherosclerosis: a randomized controlled trial. JAMA 291(9):1071–1080. https://doi.org/10.1001/jama.291.9.1071
Nissen SE, Nicholls SJ, Sipahi I et al (2006) Effect of very high-intensity statin therapy on regression of coronary atherosclerosis: the ASTEROID trial. JAMA 295(13):1556–1565. https://doi.org/10.1001/jama.295.13.jpc60002
Notarbartolo A, Davì G, Averna M et al (1995) Inhibition of thromboxane biosynthesis and platelet function by simvastatin in type IIa hypercholesterolemia. Arterioscler Thromb Vasc Biol 15(2):247–251. https://doi.org/10.1161/01.atv.15.2.247
Nowak WN, Deng J, Ruan XZ, Xu Q (2017) Reactive oxygen species generation and atherosclerosis. Arterioscler Thromb Vasc Biol 37(5):e41–e52. https://doi.org/10.1161/ATVBAHA.117.309228
Oesterle A, Liao JK (2019) The pleiotropic effects of statins—from coronary artery disease and stroke to atrial fibrillation and ventricular tachyarrhythmia. Curr Vasc Pharmacol 17(3):222–232. https://doi.org/10.2174/1570161116666180817155058
Oesterle A, Laufs U, Liao JK (2017) Pleiotropic effects of statins on the cardiovascular system. Circ Res 120(1):229–243. https://doi.org/10.1161/circresaha.116.308537
Onorato D, Pucci M, Carpene G, Henry BM, Sanchis-Gomar F, Lippi G (2021) Protective effects of statins administration in European and North American patients infected with COVID-19: a meta-analysis. Semin Thromb Hemost 47(4):392–399. https://doi.org/10.1055/s-0040-1722307
Opper C, Clement C, Schwarz H et al (1995) Increased number of high sensitive platelets in hypercholesterolemia, cardiovascular diseases, and after incubation with cholesterol. Atherosclerosis 113(2):211–217. https://doi.org/10.1016/0021-9150(94)05448-r
Patti G, Chello M, Candura D et al (2006) Randomized trial of atorvastatin for reduction of postoperative atrial fibrillation in patients undergoing cardiac surgery. Circulation 114(14):1455–1461. https://doi.org/10.1161/CIRCULATIONAHA.106.621763
Pesaro AEP, Serrano CV, Fernandes JL et al (2012) Pleiotropic effects of ezetimibe/simvastatin vs. high dose simvastatin. Int J Cardiol 158(3):400–404. https://doi.org/10.1016/j.ijcard.2011.01.062
Pignatelli P, Carnevale R, Pastori D et al (2012) Immediate antioxidant and antiplatelet effect of atorvastatin via inhibition of Nox2. Circulation 126(1):92–103. https://doi.org/10.1161/CIRCULATIONAHA.112.095554
Plenz GA, Hofnagel O, Robenek H (2004) Differential modulation of caveolin-1 expression in cells of the vasculature by statins. Circulation 109(2):e7-8. https://doi.org/10.1161/01.Cir.0000111128.83347.7a. (author reply e7–8)
Qu H, Guo M, Chai H, Wang W, Zy G, Dz S (2018) Effects of coenzyme Q10 on statin-induced myopathy: an updated meta-analysis of randomized controlled trials. J Am Heart Assoc 7(19):e009835. https://doi.org/10.1161/JAHA.118.009835
Rajpathak SN, Kumbhani DJ, Crandall J, Barzilai N, Alderman M, Ridker PM (2009) Statin therapy and risk of developing type 2 diabetes: a meta-analysis. Diabetes Care 32(10):1924–1929. https://doi.org/10.2337/dc09-0738
Ray JG, Mamdani M, Tsuyuki RT, Anderson DR, Yeo EL, Laupacis A (2001) Use of statins and the subsequent development of deep vein thrombosis. Arch Intern Med 161(11):1405–1410. https://doi.org/10.1001/archinte.161.11.1405
Ray KK, Bays HE, Catapano AL et al (2019) Safety and efficacy of bempedoic acid to reduce LDL cholesterol. N Engl J Med 380(11):1022–1032. https://doi.org/10.1056/NEJMoa1803917
Reichel M, Knauf F (2021) Statins, obesity, and the microbiome: a potential mechanism for the pleiotropic effects of statin therapy. Kidney Int 99(3):531–533. https://doi.org/10.1016/j.kint.2020.07.038
Ribe AR, Vestergaard CH, Vestergaard M et al (2020) Statins and risk of intracerebral hemorrhage in individuals with a history of stroke. Stroke 51(4):1111–1119. https://doi.org/10.1161/STROKEAHA.119.027301
Ridker PM, Rifai N, Pfeffer MA et al (1998) Inflammation, pravastatin, and the risk of coronary events after myocardial infarction in patients with average cholesterol levels. Cholesterol and Recurrent Events (CARE) Investigators. Circulation 98(9):839–844. https://doi.org/10.1161/01.cir.98.9.839
Ridker PM, Danielson E, Fonseca FA et al (2008) Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med 359(21):2195–2207. https://doi.org/10.1056/NEJMoa0807646
Ridker PM, Pradhan A, MacFadyen JG, Libby P, Glynn RJ (2012) Cardiovascular benefits and diabetes risks of statin therapy in primary prevention: an analysis from the JUPITER trial. Lancet 380(9841):565–571. https://doi.org/10.1016/S0140-6736(12)61190-8
Ridker PM, Everett BM, Thuren T et al (2017) Antiinflammatory therapy with canakinumab for atherosclerotic disease. N Engl J Med 377(12):1119–1131. https://doi.org/10.1056/NEJMoa1707914
Ridker PM, Koenig W, Kastelein JJ, Mach F, Lüscher TF (2018) Has the time finally come to measure hsCRP universally in primary and secondary cardiovascular prevention? Eur Heart J 39(46):4109–4111. https://doi.org/10.1093/eurheartj/ehy723
Ridker PM, Everett BM, Pradhan A et al (2019) Low-dose methotrexate for the prevention of atherosclerotic events. N Engl J Med 380(8):752–762. https://doi.org/10.1056/NEJMoa1809798
Roberts JM, Redman CWG (1993) Pre-eclampsia: more than pregnancy-induced hypertension. Lancet 341(8858):1447–1451. https://doi.org/10.1016/0140-6736(93)90889-O
Rosenson RS, Baker SK, Jacobson TA, Kopecky SL, Parker BA (2014) An assessment by the Statin Muscle Safety Task Force: 2014 update. J Clin Lipidol 8(3, Supplement):S58–S71. https://doi.org/10.1016/j.jacl.2014.03.004
Sabatine MS, Giugliano RP, Keech AC et al (2017) Evolocumab and clinical outcomes in patients with cardiovascular disease. N Engl J Med 376(18):1713–1722. https://doi.org/10.1056/NEJMoa1615664
Sacks FM, Pfeffer MA, Moye LA et al (1996) The effect of pravastatin on coronary events after myocardial infarction in patients with average cholesterol levels. Cholesterol and Recurrent Events Trial investigators. N Engl J Med 335(14):1001–1009. https://doi.org/10.1056/nejm199610033351401
Sattar N, Preiss D, Murray HM et al (2010a) Statins and risk of incident diabetes: a collaborative meta-analysis of randomised statin trials. Lancet 375(9716):735–742. https://doi.org/10.1016/S0140-6736(09)61965-6
Sattar N, Preiss D, Murray HM et al (2010b) Statins and risk of incident diabetes: a collaborative meta-analysis of randomised statin trials. Lancet 375(9716):735–742. https://doi.org/10.1016/S0140-6736(09)61965-6
Schaefer WH, Lawrence JW, Loughlin AF et al (2004) Evaluation of ubiquinone concentration and mitochondrial function relative to cerivastatin-induced skeletal myopathy in rats. Toxicol Appl Pharmacol 194(1):10–23. https://doi.org/10.1016/j.taap.2003.08.013
Schech S, Graham D, Staffa J et al (2007) Risk factors for statin-associated rhabdomyolysis. Pharmacoepidemiol Drug Saf 16(3):352–358. https://doi.org/10.1002/pds.1287
Scheen AJ (2021) Statins and clinical outcomes with COVID-19: Meta-analyses of observational studies. Diabetes Metab 47(6):101220. https://doi.org/10.1016/j.diabet.2020.101220
Schultz BG, Patten DK, Berlau DJ (2018) The role of statins in both cognitive impairment and protection against dementia: a tale of two mechanisms. Transl Neurodegener 7:5–5. https://doi.org/10.1186/s40035-018-0110-3
Schwartz GG, Olsson AG, Ezekowitz MD et al (2001) Effects of atorvastatin on early recurrent ischemic events in acute coronary syndromes: the MIRACL study: a randomized controlled trial. JAMA 285(13):1711–1718. https://doi.org/10.1001/jama.285.13.1711
Schwartz GG, Steg PG, Szarek M et al (2018) Alirocumab and cardiovascular outcomes after acute coronary syndrome. N Engl J Med 379(22):2097–2107. https://doi.org/10.1056/NEJMoa1801174
Sen-Banerjee S, Mir S, Lin Z et al (2005) Kruppel-like factor 2 as a novel mediator of statin effects in endothelial cells. Circulation 112(5):720–726. https://doi.org/10.1161/CIRCULATIONAHA.104.525774
Shahar E, Chambless LE, Rosamond WD et al (2003) Plasma lipid profile and incident ischemic stroke: the Atherosclerosis Risk in Communities (ARIC) study. Stroke 34(3):623–631. https://doi.org/10.1161/01.Str.0000057812.51734.Ff
Siddiqui MK, Maroteau C, Veluchamy A et al (2017) A common missense variant of LILRB5 is associated with statin intolerance and myalgia. Eur Heart J 38(48):3569–3575. https://doi.org/10.1093/eurheartj/ehx467
Silverman MG, Ference BA, Im K et al (2016) Association between lowering LDL-C and cardiovascular risk reduction among different therapeutic interventions: a systematic review and meta-analysis. JAMA 316(12):1289–1297. https://doi.org/10.1001/jama.2016.13985
Simoncini T, Hafezi-Moghadam A, Brazil DP, Ley K, Chin WW, Liao JK (2000) Interaction of oestrogen receptor with the regulatory subunit of phosphatidylinositol-3-OH kinase. Nature 407(6803):538–541. https://doi.org/10.1038/35035131
Sorokin AV, Duncan B, Panetta R, Thompson PD (2006) Rhabdomyolysis associated with pomegranate juice consumption. Am J Cardiol 98(5):705–706. https://doi.org/10.1016/j.amjcard.2006.03.057
Sparks LD, Kryscio JR, Sabbagh NM, Connor JD, Sparks ML, Liebsack C (2008) Reduced risk of incident AD with elective statin use in a clinical trial cohort. Curr Alzheimer Res 5(4):416–421. https://doi.org/10.2174/156720508785132316
Stary HC, Chandler AB, Glagov S et al (1994) A definition of initial, fatty streak, and intermediate lesions of atherosclerosis. A report from the Committee on Vascular Lesions of the Council on Arteriosclerosis. American Heart Association. Circulation 89(5):2462–2478. https://doi.org/10.1161/01.CIR.89.5.2462
Stone NJ, Robinson JG, Lichtenstein AH et al (2014) 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 63(25 Pt B):2889–2934. https://doi.org/10.1016/j.jacc.2013.11.002
Suzumura K, Yasuhara M, Tanaka K, Suzuki T (1999) Protective effect of fluvastatin sodium (XU-62-320), a 3-hydroxy-3-methylglutaryl coenzyme a (HMG-CoA) reductase inhibitor, on oxidative modification of human low-density lipoprotein in vitro. Biochem Pharmacol 57(6):697–703. https://doi.org/10.1016/S0006-2952(98)00341-4
Tai W, He L, Zhang X et al (2020) Characterization of the receptor-binding domain (RBD) of 2019 novel coronavirus: implication for development of RBD protein as a viral attachment inhibitor and vaccine. Cell Mol Immunol 17(6):613–620
Takemoto M, Node K, Nakagami H et al (2001) Statins as antioxidant therapy for preventing cardiac myocyte hypertrophy. J Clin Investig 108(10):1429–1437. https://doi.org/10.1172/JCI13350
Tardif JC, Kouz S, Waters DD et al (2019) Efficacy and safety of low-dose colchicine after myocardial infarction. N Engl J Med 381(26):2497–2505. https://doi.org/10.1056/NEJMoa1912388
Thompson Paul D, Panza G, Zaleski A, Taylor B (2016) Statin-associated side effects. J Am Coll Cardiol 67(20):2395–2410. https://doi.org/10.1016/j.jacc.2016.02.071
Tonkin A, Aylward P, Colquhoun D et al (1998) Prevention of cardiovascular events and death with pravastatin in patients with coronary heart disease and a broad range of initial cholesterol levels. N Engl J Med 339(19):1349–1357. https://doi.org/10.1056/nejm199811053391902
Torres-Peña JD, Katsiki N, Perez-Martinez P (2021) Could statin therapy be useful in patients with coronavirus disease 2019 (COVID-19)? Front Cardiovasc Med. https://doi.org/10.3389/fcvm.2021.775749
Tsao CW, Aday AW, Almarzooq ZI et al (2022) Heart disease and stroke statistics-2022 update: a report from the American Heart Association. Circulation. https://doi.org/10.1161/CIR.0000000000001052
Vega GL, Grundy SM (1991) Influence of lovastatin therapy on metabolism of low density lipoproteins in mixed hyperlipidaemia. J Intern Med 230(4):341–350. https://doi.org/10.1111/j.1365-2796.1991.tb00454.x
Vieira-Silva S, Falony G, Belda E et al (2020) Statin therapy is associated with lower prevalence of gut microbiota dysbiosis. Nature 581(7808):310–315. https://doi.org/10.1038/s41586-020-2269-x
Violi F, Calvieri C, Ferro D, Pignatelli P (2013) Statins as antithrombotic drugs. Circulation 127(2):251–257. https://doi.org/10.1161/CIRCULATIONAHA.112.145334
Waters DD, Ho JE, DeMicco DA et al (2011) Predictors of new-onset diabetes in patients treated with atorvastatin: results from 3 large randomized clinical trials. J Am Coll Cardiol 57(14):1535–1545. https://doi.org/10.1016/j.jacc.2010.10.047
Waters DD, Ho JE, Boekholdt SM et al (2013) Cardiovascular event reduction versus new-onset diabetes during atorvastatin therapy: effect of baseline risk factors for diabetes. J Am Coll Cardiol 61(2):148–152. https://doi.org/10.1016/j.jacc.2012.09.042
Wei J, Liao JK, Merz CNB (2021) Challenging statin pleiotropy: preeclampsia. Circulation 144(9):680–683. https://doi.org/10.1161/CIRCULATIONAHA.121.056140
Weitz-Schmidt G, Welzenbach K, Brinkmann V et al (2001) Statins selectively inhibit leukocyte function antigen-1 by binding to a novel regulatory integrin site. Nat Med 7(6):687–692. https://doi.org/10.1038/89058
Westerink J, Deanfield JE, Imholz BP et al (2013) High-dose statin monotherapy versus low-dose statin/ezetimibe combination on fasting and postprandial lipids and endothelial function in obese patients with the metabolic syndrome: the PANACEA study. Atherosclerosis 227(1):118–124. https://doi.org/10.1016/j.atherosclerosis.2012.11.028
Wilmanski T, Kornilov SA, Diener C et al (2022) Heterogeneity in statin responses explained by variation in the human gut microbiome. Med 3(6):388-405.e6. https://doi.org/10.1016/j.medj.2022.04.007
Xie Y, Xu E, Bowe B, Al-Aly Z (2022) Long-term cardiovascular outcomes of COVID-19. Nat Med 28(3):583–590. https://doi.org/10.1038/s41591-022-01689-3
Xu CB, Stenman E, Edvinsson L (2002) Reduction of bFGF-induced smooth muscle cell proliferation and endothelin receptor mRNA expression by mevastatin and atorvastatin. Biochem Pharmacol 64(3):497–505. https://doi.org/10.1016/s0006-2952(02)01189-9
Yaffe K, Barrett-Connor E, Lin F, Grady D (2002) Serum lipoprotein levels, statin use, and cognitive function in older women. Arch Neurol 59(3):378–384. https://doi.org/10.1001/archneur.59.3.378
Yu D, Liao JK (2022) Emerging views of statin pleiotropy and cholesterol lowering. Cardiovasc Res 118(2):413–423. https://doi.org/10.1093/cvr/cvab032
Zheng Z, Jayaram R, Jiang L et al (2016) Perioperative rosuvastatin in cardiac surgery. N Engl J Med 374(18):1744–1753. https://doi.org/10.1056/NEJMoa1507750
Zhou Z, Ryan J, Ernst Michael E et al (2021) Effect of statin therapy on cognitive decline and incident dementia in older adults. J Am Coll Cardiol 77(25):3145–3156. https://doi.org/10.1016/j.jacc.2021.04.075
Funding
No funding was received to assist with the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
This was a solicited review article. CG performed the literature review and drafted the manuscript, and JL provided critical review and edits to the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
German, C.A., Liao, J.K. Understanding the molecular mechanisms of statin pleiotropic effects. Arch Toxicol 97, 1529–1545 (2023). https://doi.org/10.1007/s00204-023-03492-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00204-023-03492-6