Abstract
Summary
This study aimed to better define the role of heel-QUS in fracture prediction. Our results showed that heel-QUS predicts fracture independently of FRAX, BMD, and TBS. This corroborates its use as a case finding/pre-screening tool in osteoporosis management.
Introduction
Quantitative ultrasound (QUS) characterizes bone tissue based on the speed of sound (SOS) and broadband ultrasound attenuation (BUA). Heel-QUS predicts osteoporotic fractures independently of clinical risk factors (CRFs) and bone mineral density (BMD). We aimed to investigate whether (1) heel-QUS parameters predict major osteoporotic fractures (MOF) independently of the trabecular bone score (TBS) and (2) the change of heel-QUS parameters over 2.5 years is associated with fracture risk.
Methods
One thousand three hundred forty-five postmenopausal women from the OsteoLaus cohort were followed up for 7 years. Heel-QUS (SOS, BUA, and stiffness index (SI)), DXA (BMD and TBS), and MOF were assessed every 2.5 years. Pearson’s correlation and multivariable regression analyses were used to determine associations between QUS and DXA parameters and fracture incidence.
Results
During a mean follow-up of 6.7 years, 200 MOF were recorded. Fractured women were older, more treated with anti-osteoporosis medication; had lower QUS, BMD, and TBS; higher FRAX-CRF risk; and more prevalent fractures. TBS was significantly correlated with SOS (0.409) and SI (0.472). A decrease of one SD in SI, BUA or SOS increased the MOF risk by (OR(95%CI)) 1.43 (1.18–1.75), 1.19 (0.99–1.43), and 1.52 (1.26–1.84), respectively, after adjustment for FRAX-CRF, treatment, BMD, and TBS. We found no association between the change of QUS parameters in 2.5 years and incident MOF.
Conclusion
Heel-QUS predicts fracture independently of FRAX, BMD, and TBS. Thus, QUS represents an important case finding/pre-screening tool in osteoporosis management. The change in QUS over time was not associated with future fractures, making it inappropriate for patient monitoring.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is a bone disorder affecting bone quantity and quality, which increases the risk of fracture. Dual-energy X-ray absorptiometry (DXA) scanning in the hip and lumbar spine (LS) is the gold standard for osteoporosis diagnosis. DXA provides the assessment of bone mineral density (BMD)—a bone quantity assessor—in the total hip (TH), femoral neck (FN), and LS, and of trabecular bone score (TBS)—a bone microarchitecture proxy—in the LS [1]. The operational diagnosis of osteoporosis is based on the presence of a fragility fracture and/or low BMD values at any of the three regions (T-score ≤ − 2.5 SD) [2]. About 50% of women who have an osteoporotic fracture do not have osteoporotic BMD values [3, 4], suggesting that BMD is insufficient to predict fracture, and confirming its multifactorial nature. Assessment can be completed by using the Fracture Risk Assessment Tool (FRAX), which calculates the 10-year probability of having an osteoporotic fracture based on clinical risk factors for fracture (CRF), and/or the DXA-derived parameters: BMD and TBS [5,6,7]. Unfortunately, despite these diagnosis tools and the fact that fractures are preventable [8], the lack of osteoporosis diagnosis has contributed to an important osteoporosis treatment gap [9,10,11]. This is partly because DXA exams are performed at a specialized radiology or nuclear medicine facilities. Improving the distribution of a screening strategy for osteoporosis could increase its awareness and eventually diagnosis and treatment. Further, the significant decrease in reimbursement for DXA in the USA and the disappearance of DXA centers because of this is an additional contributor.
Quantitative ultrasound (QUS) is a technology that sends and receives subaudible soundwaves through the bone. It characterizes bone tissue based on the ultrasound velocity (the speed of sound (SOS, in m/s)), attenuation (broadband ultrasound attenuation (BUA, in dB/MHz), and stiffness index (SI) [12]. Heel (or calcaneus) is the most-established QUS skeletal site for fracture prediction. Heel QUS parameters can predict fractures independently of clinical risk factors and BMD. Its fracture prediction ability is numerically similar to the one of DXA [12]. SOS and BUA reflect the mechanical and physical properties of the bone, such as elasticity, microarchitecture, and strength [13], and thus, their predictive value could be somewhat similar to that of TBS. On the other hand, it has been suggested that QUS might give different information from TBS in vivo; however, these preliminary data need confirmation [14, 15]. Advantages of the heel QUS over DXA are the lack of ionizing radiation, lower cost, and ease at transportation. Despite these clear advantages, currently this technology is not widely used in practice due to the lack of devices (it is no longer serviced in the USA), lack of specific validated thresholds for the QUS parameters, its very low sensitivity to change, and the lack of a clear effect of anti-osteoporotic treatment on QUS [12]. The International Society for Clinical Densitometry (ISCD) suggests using QUS as a prescreening tool for osteoporosis, which would identify people at low risk of fracture based on CRF and QUS parameters and for whom no further diagnostic assessment would be required. The use of QUS for follow-up objectives is not sufficiently studied [16]. Moreover, peripheral sites tend to be less responsive to treatment than axial skeletal sites. Using easily accessible tools, such as QUS, in prescreening strategies for osteoporosis might contribute at improving the existing gap in its diagnosis and treatment.
The overall aim of this study was to better define the role of heel QUS in predicting fracture risk in postmenopausal women in the OsteoLaus cohort. The first aim was to investigate whether heel QUS parameters can predict fractures independently of TBS, in addition to BMD and CRF. The secondary aim was to investigate if the change in percent of heel QUS parameters over 2.5 years is associated with incident fractures risk.
Methods
Study population
OsteoLaus, a sub-study of the CoLaus cohort, is an ongoing populational cohort of postmenopausal women aged ≥ 50 years at baseline, living in Lausanne. The cohort has been previously described in detail [17, 18]. A total of 1475 OsteoLaus participants underwent a baseline visit (March 2010–December 2012) and a follow-up visit every 2.5 years with almost 70% retention at the 4th visit. In this analysis, we use the data collected during the baseline, second, third, and fourth visits, comprising a mean total follow-up period of 6.7 years.
The Ethics Committee for Human Research of Canton Vaud approved the CoLaus Study and subsequently the OsteoLaus Study. All participants signed a written informed consent after having received a detailed description of the funding and aim of the study.
QUS assessments
QUS was measured at the heel at each OsteoLaus visit using the Achilles Express apparatus (GE-Lunar Co., Madison, USA), calibrated daily according to the manufacturer’s recommendation. The measurements were performed on the right heel; in case of a prevalent fracture on the right heel, they were performed on the left. All measurements were done by the same operator. The device directly measured SOS and BUA, and its software automatically calculated the SI, a manufacturer composite parameter: SI = 0.67 × BUA + 0.28 × SOS-420. The measurement precision, as expressed in coefficient of variation (CV%) in previous articles ranges between 1.85–3.40% for BUA, 0.26–0.30% for SOS, and 1.84–2.35% for SI [19,20,21,22]. We calculated the relative change (%) of the QUS parameters (ΔSI, ΔBUA, ΔSOS) between baseline and 2.5y using the next formula: Δparameter = (parameter2.5y—parameterbaseline)/parameterbaseline.
DXA assessments
DXA was performed on LS and hip using Discovery A System (Hologic Inc., Waltham, MA, USA), at baseline and at first follow-up visit. The machine quality control was performed daily with the spine phantom supplied by the manufacturers. Hip DXA was performed on the left hip. In case of hip replacement, the DXA scan was done on the right side. BMD and BMD T-scores were assessed for the TH, FN, and LS using NHANES reference database. TBSTT was calculated on the antero-posterior LS DXA scans using a research version of the TBS software, which is corrected for the regional soft tissue thickness (TBS iNsight BetaTT, Medimaps group, Geneva, Switzerland). Both LS BMD and TBSTT were calculated from the L1-L4 region, respecting the ISCD vertebrae exclusion criteria [16]. We calculated the relative change (in %) of DXA parameters (ΔFN BMD and ΔTBS) between baseline and 2.5y visit using the same formula as for the QUS parameters.
Fracture’s assessments
Major osteoporotic fractures (MOFs) comprised radiological VF, and clinical hip, forearm, or humerus fractures. Hip, forearm, and humerus fractures data were collected from questionnaires. In the questionnaire, for each fracture, the date of occurrence, type (traumatic, non-traumatic, pathological), and site were specified. Vertebral fractures (VF) were assessed from the vertebral fracture assessment (VFA). Each study participant had a VFA image at each study visit, baseline, and follow-up visits. The presence of VF was assessed at each visit by two independent readers using the Genant’s semi-quantitative method [23]; discrepancies were adjudicated with the presence of a third reader. This method grades vertebral fractures from grade 1 to 3, where 3 is the most severe with a vertebra height loss of > 40% and 1 the mildest with a vertebra height loss of 20–25%. In this analysis, moderate (grade 2) and severe (grade 3) VF were included; two grade 1 VF were considered as one grade 2. To note, the percentage height loss is calculated as compared to the adjacent vertebra or its own anterior/posterior/middle height.
CRF and FRAX assessments
General characteristics, history of fractures, bone active medication intake (bisphosphonate, raloxifene, strontium ranelate, denosumab, teriparatide), and CRF data were collected from the questionnaires. The Swiss FRAXR assessment tool [www.shef.ac.uk/FRAX] was used to estimate the 10-year probability of having a major osteoporotic fracture based only on the CRF.
Statistical analysis
Baseline characteristics of participants were expressed as means and standard deviations (SDs) for continuous variables and as count (%) for categorical variables. Shapiro–Wilk test was used to assess whether variables were normally distributed. Differences between the women who had an incident MOF over 7 years and those who did not were assessed with independent-sample two‐tailed t-tests or chi‐square tests, as appropriate.
Pearson correlation coefficients were used to assess bivariate associations between DXA (LS BMD, FN BMD, LS TBS) and QUS parameters (SI, BUA, SOS, ΔSI, ΔBUA, and ΔSOS). Multivariate binary logistic regressions were used to assess the risk estimates of having an incident MOF per one standard deviation lower value for each three QUS parameters SOS, BUA, and SI (analysis 1) or their relative changes from baseline to the first follow-up visit after 2.5 years (ΔSOS, ΔBUA, ΔSI; analysis 2). For the analysis 1, models were adjusted for (i) FRAX and osteoporosis treatment intake (bisphosphonate, raloxifene, strontium ranelate, denosumab, teriparatide), (ii) additionally for FN BMD, and (iii) additionally for TBS. For analysis 2, models were adjusted for (i) the corresponding baseline QUS value, FRAX and osteoporosis treatment intake (bisphosphonate, raloxifene, strontium ranelate, denosumab, teriparatide), (ii) additionally for ΔFN BMD, and (iii) additionally for ΔTBS.
Incident MOF that had occurred during the 7.5-year period between baseline and visit 4 were considered in the models with baseline QUS parameters (analysis 1). Incident MOF that had occurred during the 5-year period between visit 2 and visit 4 were considered for the models of ΔQUS parameters (analysis 2). The results were expressed as beta standardized coefficients with their respective 95% confidence intervals (95% CI).
P < 0.05 was considered statistically significant. All statical analysis were conducted using SPSS Statistics for Macintosh, Version 27.0. Armonk, NY: IBM Corp.
Results
Baseline characteristics
Out of the 1475 post-menopausal women who participated at the baseline visit, 1345 were included in the analysis using the baseline values of the QUS parameters, and 1185 were included in the analysis using the relative changes of the QUS parameters. A flowchart of the study population is shown in Fig. 1.
Flowchart of the study population. Analysis 1: fracture prediction at 7.5 years by baseline QUS; analysis 2: fracture prediction at 5 years by ΔQUS. DXA, dual-energy X-ray absorptiometry; QUS, quantitative ultrasound. aWere included those who had DXA and QUS data at baseline and participated at least at visit 2 or 3 or 4; bwere included those who had ΔDXA and ΔQUS data and participated at least at visit 3 or 4
The baseline characteristics of all study participants and the differences in baseline characteristics between the fractured and non-fractured participants are shown in Table 1. The clinical characteristics of excluded and included participants are provided in supplementary material.
During the mean follow-up period of 6.7 (SD 1.5) years, 200 women experienced a MOF, of which 64% were a VF, 8% hip, 16% humerus, and 12% forearm (7% had two or more MOF). Women who fractured were older; had lower QUS, BMD, and TBS values; higher FRAX-CRF risk; and were more likely to have received osteoporosis treatment. However, there was no difference between the two groups for ΔBUA and ΔSOS.
Correlation among and between QUS and DXA parameters
We first calculated Pearson’s correlation coefficients between LS BMD, FN BMD, LS TBS, SI, BUA, SOS, ΔSI, ΔBUA, and ΔSOS (Table 2). All QUS parameters were moderately positively correlated with FN BMD, LS BMD, and TBS, with SI coefficients higher than for BUA or SOS (r = 0.449 to 0.472; vs. 0.376 to 0.422); correlation between BUA and SOS was only slightly stronger (r = 0.532; all p < 0.01). TBS was significantly correlated with SOS (0.409) and SI (0.472). SI, BUA, and SOS were weakly negatively correlated with their relative change in 2.5 years. There was no significant correlation between QUS relative changes and BMD or TBS values. Partial correlation coefficients adjusted for age and anti-osteoporotic treatment intake showed similar results (not shown).
Performance of QUS parameters in fracture prediction
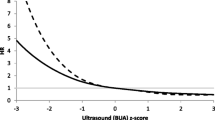
The odds ratios (95% CI) of having a MOF in the following 6.7 years were, for each SD decrease in SI, BUA, and SOS, 1.59 (1.33–1.90), 1.33 (1.13–1.57), and 1.69 (1.41–2.02), respectively, in a model adjusted for FRAX and anti-osteoporotic treatment intake (Table 3, model 1). These results remained significant after additional adjustment for FN BMD (model 2) and FN BMD and TBS (model 3), except for BUA in model 3 although showing a trend at the limit of significance. For every one SD in SI, BUA, or SOS, there was an inverse increase in the risk of MOF by 1.43 (1.18–1.75), 1.19 (0.99–1.43), and 1.52 (1.26–1.84), respectively, after adjustment for FRAX-CRF, osteoporosis treatment, BMD, and TBS. Similar trends were seen in the analysis for VF only (Supplementary Material). The relative percentage change of SI, BUA, or SOS over 2.5 years was not associated with the odds of having a fracture in the next 5 years in any of the three models (Table 4), which is consistent with QUS ability to provide a screening one-time assessment of fracture risk, in contrast to BMD and TBS which can provide accurate longitudinal measurements.
Discussion
This study investigated the fracture’s prediction ability of QUS-derived parameters, and of their relative change in 2.5 years. Our findings showed that the QUS-derived parameters are associated with the odds of having a MOF over a period of 7 years independently not only of the clinical risk factors and BMD, but of TBS also. This implicates that QUS-derived parameters give information on bone health, additionally to BMD and TBS. The relative change of SI, BUA and SOS over 2.5 years was not associated with the odds of having a MOF in the next 5 years.
Correlation between the QUS- and DXA-derived bone parameters
The correlations found between the QUS parameters and BMD values were within the range reported by previous studies, with BUA being generally more strongly correlated with all BMD values than SOS [24,25,26,27]. The degree of correlation between each of the QUS parameters was very close for both BMD and TBS, while previous studies have reported lower correlations between QUS parameters and TBS [14, 15]. As BUA is known as an estimator of bone structure, Olmos et al. speculated that TBS and QUS might be capturing different aspects of bone microarchitecture [14]. The higher correlation between QUS and TBS seen in our study might be due to the TBS version that we use—TBSTT—which is adjusted for tissue thickness, while previous studies used TBS adjusted for BMI. To note, TBSTT has been reported to better predict incident fractures than previous TBS adjusted for BMI [28]. However, the difference between both TBS software version does not substantially affect the correlation of bone properties that QUS and TBS indicate.
Furthermore, SI, BUA, and SOS were all weakly negatively correlated with their relative change over 2.5 years, suggesting that those with higher values of SI, BUA or SOS loose more of the respective parameter over the next 2.5 years than those with lower values. Also, as previously seen, ΔSOS and ΔBUA were negatively correlated, indicating for changes in different directions over the 2.5 years. Schott et al. [29] followed 113 healthy post-menopausal women for 1.9 years and found no significant correlation between ΔSOS and ΔBUA (R = + 0.13; p = 0.2). Rosenthall et al. [30] studied the change of QUS parameters after 1 to 4 years of treatment with estrogen, bisphosphonate, high-dose vitamin D, and calcium or combination of them in 673 postmenopausal women and reported a negative correlation between SOS and BUA changes only among the treated individuals. They attributed this difference to the different bone properties assessed by the two parameters. In vivo studies [31, 32] have shown that BUA is influenced by bone density and structure, and SOS by bone density and elasticity. In our analysis, this correlation remained negative after adjusting for anti-osteoporotic treatment intake, suggesting that there was no effect of treatment on this correlation.
CRF-, BMD-, and TBS-independent association with fracture risk of the QUS parameters
Our study showed the QUS-derived parameters ability to predict MOF independently of FRAX, BMD, TBS, and anti-osteoporotic treatment intake over a mean follow-up period of 6.7 years. As a summary of previous studies, McCloskey et al. [6] concluded, in an individual level meta-analysis regrouping 46,124 participants, that QUS is a predictor of fracture in men and women independently of both age and BMD, particularly at low value, but its prediction ability decreases over the follow-up time since QUS assessment.
Our results showing that QUS predicts MOF independently of FRAX are consistent with the data from other prospective studies. Hans et al. [33] followed 13,000 postmenopausal women and found that combining CRF and SI predicts better the 10-year hip fracture probability than CRF or SI alone. Another similar study concluded that BUA could predict fractures independently of CRF and BMD [34]. Also, in accordance with other studies, the predictive value of QUS parameters dropped when further adjusting for BMD although remaining significant [6, 35]. In our study, this remained true after additional adjustment for TBS, with the OR for BUA at the limit of significance. This independence in fracture prediction could be explained by the fact that QUS is measured at a different site than TBS and BMD; it is known that bone measurements differ from one site to another. Also, QUS and DXA might capture complementary properties of bone health, which are predictors of fracture.
Among the three QUS parameters assessed, in the current study, SOS has the highest association with the odds of fracture, approximately 10 to 40% higher than SI and BUA, respectively. Other studies have reported that SI or BUA are superior to SOS at fracture prediction [6, 35]. This variability might be due to the type of osteoporotic fractures considered, as 64% of the MOF in our study were VF; a similar trend with SOS being a better predictor than BUA was observed in other studies on VF [6, 35, 36].
The change of QUS parameters over 2.5 years and its fracture predictive ability
This analysis showed that the changes of all three QUS parameters over 2.5 years were not associated with the odds of having a fracture in the following 5 years. The variation of QUS over time in adults has been studied in different contexts, mainly in interventional studies [25, 30, 37,38,39,40], in the evolution of QUS with ageing [29], in the comparison of QUS and DXA [20], and in the evaluation of the performance of QUS devices [19, 21]. In overall, QUS has a good precision, yet it remains low compared to the observed rates of change. In fact, the precision error of BUA and SOS is respectively 6–9 and 2–8 times larger than their annual rate loss [41]. This limits the QUS use as a relevant tool for treatment monitoring. However, Sahota et al. [25] suggested that it might be useful for longer-term monitoring. In this line, the lack of association of the QUS parameters changes over 2.5 years with fracture risk in our study, was expected.
Strengths and limitations
To our knowledge, this is the first study assessing the prediction of fracture from QUS parameters independently of TBS in addition to FRAX and BMD. The monocentric nature of the OsteoLaus cohort, where all measurements were done under the same conditions (QUS, DXA, VFA), the homogeneity of the cohort (women over 50 years), and the performance of the QUS assessments by the same technician at each visit for all visits represent a significant strength for the current study.
Some limitations need to be considered. First, the cohort is composed of European post-menopausal women; thus, the results may not be applicable to non-Europeans and to men. Second, the non-VF MOF were self-reported. Efforts to confirm them from medical records were made, but this could not be achieved for each case. However, VF which constitute 63% of the MOF, were assessed from VFAs by two independent experts. Third, the 2.5-year period to calculate a variation of QUS may be too short, as natural variation of QUS parameters is low regarding their precision [41]. Fourth, the precision of the QUS measurements was not calculated in the OsteoLaus Study center.
Conclusion
In conclusion, this study shows that heel QUS predicts fractures over a 6.7-year study duration, independently of FRAX-CRF, femoral neck BMD, and TBS. These results reinforce the rationale for using QUS combined with CRFs as a case finding/pre-screening tool as an alternative to FRAX-CRF or DXA when the latter is unavailable. Variation of QUS over 2.5 years did now show promise for future fracture prediction. Thus, it should not be used to monitor patients given changes in QUS are not associated with fracture risk.
References
Silva BC, Leslie WD, Resch H, Lamy O, Lesnyak O, Binkley N et al (2014) Trabecular bone score: a noninvasive analytical method based upon the DXA image: trabecular bone score. J Bone Miner Res 29(3):518–530
Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. Risk WHOSGoAoF, its Application to Screening for Postmenopausal O, editors. Geneva1994 1994
Siris ES, Chen Y-T, Abbott TA, Barrett-Connor E, Miller PD, Wehren LE et al (2004) Bone mineral density thresholds for pharmacological intervention to prevent fractures. Arch Intern Med 164(10):1108
Sornay-Rendu E, Munoz F, Garnero P, Duboeuf F, Delmas PD (2005) Identification of osteopenic women at high risk of fracture: the OFELY Study. J Bone Miner Res 20(10):1813–1819
Kanis JA, Johnell O, Oden A, Johansson H, McCloskey E (2008) FRAX and the assessment of fracture probability in men and women from the UK. Osteoporos Int 19(4):385–397
McCloskey EV, Kanis JA, Odén A, Harvey NC, Bauer D, González-Macias J et al (2015) Predictive ability of heel quantitative ultrasound for incident fractures: an individual-level meta-analysis. Osteoporos Int 26(7):1979–1987
McCloskey EV, Odén A, Harvey NC, Leslie WD, Hans D, Johansson H et al (2015) Adjusting Fracture Probability by Trabecular Bone Score. Calcif Tissue Int 96(6):500–509
Compston JE, McClung MR, Leslie WD (2019) Osteoporosis. The Lancet 393(10169):364–376
McCloskey E, Rathi J, Heijmans S, Blagden M, Cortet B, Czerwinski E et al (2021) The osteoporosis treatment gap in patients at risk of fracture in European primary care: a multi-country cross-sectional observational study. Osteoporos Int 32(2):251–259
Clynes MA, Harvey NC, Curtis EM, Fuggle NR, Dennison EM, Cooper C (2020) The epidemiology of osteoporosis. British Medical Bulletin ldaa005
Hernlund E, Svedbom A, Ivergård M, Compston J, Cooper C, Stenmark J et al (2013) Osteoporosis in the European Union: medical management, epidemiology and economic burden: A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos 8(1–2):136
Hans D, Métrailler A, Rodriguez EG, Lamy O, Shevroja E (2022) Quantitative ultrasound (QUS) in the management of osteoporosis and assessment of fracture risk: an update. In: Laugier P, Grimal Q, Laugier P, Grimal Q, editors. Bone Quantitative Ultrasound. 1364. Cham2022 7–34
Chin K-Y, Ima-Nirwana S (2013) Calcaneal quantitative ultrasound as a determinant of bone health status: what properties of bone does it reflect? Int J Med Sci 10(12):1778–1783
Olmos JM, Hernández JL, Pariente E, Martínez J, Valero C, González-Macías J (2020) Trabecular bone score and bone quantitative ultrasound in Spanish postmenopausal women. The Camargo Cohort. Study Maturitas 132:24–29
Rufus-Membere P, Holloway-Kew KL, Diez-Perez A, Kotowicz MA, Pasco JA (2021) Associations between Bone Material Strength Index, Calcaneal quantitative ultrasound, and bone mineral density in men. J Endocr Soc 5(4):bvaa179
Shuhart CR, Yeap SS, Anderson PA, Jankowski LG, Lewiecki EM, Morse LR et al (2019) Executive Summary of the 2019 ISCD Position Development Conference on Monitoring Treatment, DXA Cross-calibration and Least Significant Change, Spinal Cord Injury, Peri-prosthetic and Orthopedic Bone Health, Transgender Medicine, and Pediatrics. J Clin Densitom 22(4):453–71
Firmann M, Mayor V, Vidal PM, Bochud M, Pécoud A, Hayoz D et al (2008) The CoLaus study: a population-based study to investigate the epidemiology and genetic determinants of cardiovascular risk factors and metabolic syndrome. BMC Cardiovasc Disord 8:6
Shevroja E, Marques-Vidal P, Aubry-Rozier B, Hans G, Rivadeneira F, Lamy O et al (2019) Cohort Profile: The OsteoLaus study. Int J Epidemiol 48(4):1046–1047
Economos CD, Sacheck JM, Wacker W, Shea K, Naumova EN (2007) Precision of Lunar Achilles+ bone quality measurements: time dependency and multiple machine use in field studies. BJR 80(959):919–925
Greenspan SL, Bouxsein ML, Melton ME, Kolodny AH, Clair JH, Delucca PT et al (1997) Precision and discriminatory ability of calcaneal bone assessment technologies. J Bone Miner Res 12(8):1303–1313
Zochling J, Nguyen TV, March LM, Sambrook PN (2004) Quantitative ultrasound measurements of bone: measurement error, discordance, and their effects on longitudinal studies. Osteoporos Int 15(8)
Krieg MA, Cornuz J, Ruffieux C, Van Melle G, Büche D, Dambacher MA et al (2006) Prediction of hip fracture risk by quantitative ultrasound in more than 7000 Swiss women > or =70 years of age: comparison of three technologically different bone ultrasound devices in the SEMOF study. J Bone Miner Res 21(9):1457–1463
Genant HK, Wu CY, van Kuijk C, Nevitt MC (1993) Vertebral fracture assessment using a semiquantitative technique. J Bone Mineral Res: The Official Journal of the American Society for Bone and Mineral Research 8(9):1137–1148
Faulkner KG, McClung MR, Coleman LJ, Kingston-Sandah E (1994) Quantitative ultrasound of the heel: Correlation with densitometric measurements at different skeletal sites. Osteoporos Int 4(1):42–47
Sahota O, San P, Cawte SA, Pearson D, Hosking DJ (2000) A Comparison of the longitudinal changes in quantitative ultrasound with dual-energy X-ray absorptiometry: the four-year effects of hormone replacement therapy. Osteoporos Int 11(1):52–58
Njeh CF, Hans D, Li J, Fan B, Fuerst T, He YQ et al (2001) Comparison of six calcaneal quantitative ultrasound devices: precision and hip fracture discrimination. Osteoporos Int 11(12):1051–1062
Trimpou P, Bosaeus I, Bengtsson B-Å, Landin-Wilhelmsen K (2010) High correlation between quantitative ultrasound and DXA during 7 years of follow-up. Eur J Radiol 73(2):360–364
Shevroja E, Aubry-Rozier B, Hans G, Gonzalez-Rodriguez E, Stoll D, Lamy O et al (2019) Clinical performance of the updated trabecular bone score (TBS) algorithm, which accounts for the soft tissue thickness: the OsteoLaus Study. J Bone Miner Res 34(12):2229–2237
Schott AM, Hans D, Garnero P, Sornay-Rendu E, Delmas PD, Meunier PJ (1995) Age-related changes in os calcis ultrasonic indices: a 2-year prospective study. Osteoporos Int 5(6):478–483
Rosenthall L, Caminis J, Tenehouse A (1999) Calcaneal ultrasonometry: response to treatment in comparison with dual x-ray absorptiometry measurements of the lumbar spine and femur. Calcif Tissue Int 64(3):200–204
Cortet B, Boutry N, Dubois P, Legroux-Gérot I, Cotten A, Marchandise X (2004) Does quantitative ultrasound of bone reflect more bone mineral density than bone microarchitecture? Calcif Tissue Int 74(1):60–67
Bouxsein ML, Radloff SE (1997) Quantitative ultrasound of the calcaneus reflects the mechanical properties of calcaneal trabecular bone. J Bone Miner Res: The Official Journal of the American Society for Bone and Mineral Research 12(5):839–846
Hans D, Durosier C, Kanis JA, Johansson H, Schott-Pethelaz A-M, Krieg M-A (2008) Assessment of the 10-year probability of osteoporotic hip fracture combining clinical risk factors and heel bone ultrasound: the EPISEM prospective cohort of 12,958 elderly women. J Bone Miner Res 23(7):1045–1051
Moayyeri A, Kaptoge S, Dalzell N, Luben RN, Wareham NJ, Bingham S et al (2009) The effect of including quantitative heel ultrasound in models for estimation of 10-year absolute risk of fracture. Bone 45(2):180–184
Moayyeri A, Adams JE, Adler RA, Krieg MA, Hans D, Compston J et al (2012) Quantitative ultrasound of the heel and fracture risk assessment: an updated meta-analysis. Osteoporos Int 23(1):143–153
Glüer CC, Eastell R, Reid DM, Felsenberg D, Roux C, Barkmann R et al (2004) Association of five quantitative ultrasound devices and bone densitometry with osteoporotic vertebral fractures in a population-based sample: the OPUS Study. J Bone Miner Res 19(5):782–793
Frost ML, Blake GM, Fogelman I (2001) Changes in QUS and BMD measurements with antiresorptive therapy: a two-year longitudinal study. Calcif Tissue Int 69(3):138–146
Gonnelli S, Cepollaro C, Montagnani A, Martini S, Gennari L, Mangeri M et al (2002) Heel ultrasonography in monitoring alendronate therapy: a four-year longitudinal study. Osteoporos Int 13(5):415–421
Moschonis G, Manios Y (2006) Skeletal site-dependent response of bone mineral density and quantitative ultrasound parameters following a 12-month dietary intervention using dairy products fortified with calcium and vitamin D: the Postmenopausal Health Study. Br J Nutr 96(6):1140–1148
Atteritano M, Mazzaferro S, Frisina A, Cannata ML, Bitto A, D’Anna R et al (2009) Genistein effects on quantitative ultrasound parameters and bone mineral density in osteopenic postmenopausal women. Osteoporos Int 20(11):1947–1954
Damilakis J, Maris TG, Karantanas AH (2007) An update on the assessment of osteoporosis using radiologic techniques. Eur Radiol 17(6):1591–1602
Funding
Open access funding provided by University of Lausanne
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Didier Hans holds stock in Medimaps Group, the makers of the Trabecular Bone Score software. Antoine Métrailler, Olivier Lamy, Elena Gonzalez Rodriguez, and Enisa Shevroja declare that they have no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Métrailler, A., Hans, D., Lamy, O. et al. Heel quantitative ultrasound (QUS) predicts incident fractures independently of trabecular bone score (TBS), bone mineral density (BMD), and FRAX: the OsteoLaus Study. Osteoporos Int 34, 1401–1409 (2023). https://doi.org/10.1007/s00198-023-06728-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-023-06728-4