Abstract
Introduction and hypothesis
Age is named as a risk factor for pelvic organ prolapse (POP), despite not being the primary outcome for many observational studies. Postmenopausal status is another associated factor but has many confounders. We aimed to systematically review the role of age and/or postmenopausal status in POP development.
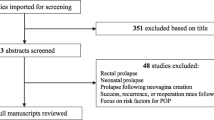
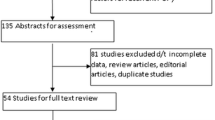
Methods
Systematic review addressing age and hormones, more specifically by postmenopausal status, from inception to March 2020 in four databases (PubMed, Embase, WOS, Cochrane Library). Quality of evidence was classified by the ROBINS-I classification for non-randomized studies. Experimental studies, animal studies, studies linking age with recurrent POP and case series were excluded. Effect estimates were collected from adjusted odds ratio plus 95% confidence intervals. Significance level was 5%. A discussion exploring mechanistic factors was also included.
Results
Nineteen studies (11 cross sectional, 6 cohort and 2 case control) were included for quantitative analysis. Only two studies presented a low overall risk of bias for age; most of the domains were of moderate risk. Every additional year was responsible for a 10% increase in the risk to develop POP (OR = 1.102 [1.021–1.190]; i2 = 80%, random analysis, p = 0.012). This trend was confirmed when age was dichotomized into a cutoff of 35 (p = 0.035) and 50 (p < 0.001) years. Although an increase in the risk for POP was noted in postmenopausal women, this did not reach statistical significance (OR = 2.080 [0.927–4.668], i2 = 0%, p = 0.076).
Conclusion
Age is a risk factor for POP; postmenopausal status was not statistically associated with POP, prompting the need for further studies addressing this factor.






Similar content being viewed by others
References
DuBeau CE. Aging and the lower urogenital system. Principles Gender-Spec Med Elsevier. 2010:432–48.
Nygaard I, Barber MD, Burgio KL, et al. Prevalence of symptomatic pelvic floor disorders in US women. Jama-J Am Med Assoc. 2008;300(11):1311–6. https://doi.org/10.1001/jama.300.11.1311.
Towers GD. The pathophysiology of pelvic organ prolapse. Female Pelv Med Reconstr Surg. 2004;10(3):109–22.
Wasenda EJ, Atan IK, Subramaniam N, Dietz HP. Pelvic organ prolapse: does hormone therapy use matter? Menopause-J North Am Menopause Soc. 2017;24(10):1185–9. https://doi.org/10.1097/GME.0000000000000898.
Fante JF, Machado HDC, Juliato CRT, Benetti-Pinto CL, Brito LGO. Pelvic floor disorders in women with premature ovarian insufficiency: a cross-sectional study. Menopause. 2020;27(4):450–8. https://doi.org/10.1097/gme.0000000000001523.
National Collaborating Centre for Women's and Children's H. National Institute for Health and Care Excellence: Clinical Guidelines. Menopause: Full Guideline. National Institute for Health and Care Excellence (UK) Copyright © 2015 National Collaborating Centre for Women's and Children's Health.; 2015.
Sterne JA, Hernán MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. Bmj. 2016;355:i4919. https://doi.org/10.1136/bmj.i4919.
Friedman T, Eslick GD, Dietz HP. Risk factors for prolapse recurrence: systematic review and meta-analysis. Int Urogynecol J. 2018;29(1):13–21. https://doi.org/10.1007/s00192-017-3475-4.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. Bmj. 2003;327(7414):557–60. https://doi.org/10.1136/bmj.327.7414.557.
Yuk JS, Lee JH, Hur JY, Shin JH. The prevalence and treatment pattern of clinically diagnosed pelvic organ prolapse: a Korean National Health Insurance Database-based cross-sectional study 2009-2015. Sci Rep. 2018;8(1):1334. https://doi.org/10.1038/s41598-018-19692-5.
Quiroz LH, White DE, Juarez D, Shobeiri SA. Age effects on pelvic floor symptoms in a cohort of nulliparous patients. Female Pelvic Med Reconstr Surg. 2012;18(6):325–8. https://doi.org/10.1097/SPV.0b013e3182720255.
Wusu-Ansah OK, Opare-Addo HS. Pelvic organ prolapse in rural Ghana. Int J Gynaecol Obstet. 2008;103(2):121–4. https://doi.org/10.1016/j.ijgo.2008.06.014.
Slieker-ten Hove MC, Pool-Goudzwaard AL, Eijkemans MJ, Steegers-Theunissen RP, Burger CW, Vierhout ME. Prediction model and prognostic index to estimate clinically relevant pelvic organ prolapse in a general female population. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20(9):1013–21. https://doi.org/10.1007/s00192-009-0903-0.
Akter F, Gartoulla P, Oldroyd J, Islam RM. Prevalence of, and risk factors for, symptomatic pelvic organ prolapse in rural Bangladesh: a cross-sectional survey study. Int Urogynecol J. 2016;27(11):1753–9. https://doi.org/10.1007/s00192-016-3038-0.
Li Z, Xu T, Gong J, Liu Q, Zhu L. An epidemiologic study of pelvic organ prolapse in rural Chinese women: a population-based sample in China. Int Urogynecol J. 2019;30(11):1925–32. https://doi.org/10.1007/s00192-018-03859-9.
Swift S, Woodman P, O'Boyle A, et al. Pelvic organ support study (POSST): the distribution, clinical definition, and epidemiologic condition of pelvic organ support defects. Am J Obstet Gynecol. 2005;192(3):795–806. https://doi.org/10.1016/j.ajog.2004.10.602.
Wusu-Ansah OK, Opare-Addo HS. Pelvic organ prolapse in rural Ghana. Int J Gynecol Obstet. 2008;103(2):121–4.
Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL. Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol. 1997;89(4):501–6.
Fialkow MF, Newton KM, Lentz GM, Weiss NS. Lifetime risk of surgical management for pelvic organ prolapse or urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19(3):437–40. https://doi.org/10.1007/s00192-007-0459-9.
Nygaard I, Barber MD, Burgio KL, et al. Prevalence of symptomatic pelvic floor disorders in US women. Jama. 2008;300(11):1311–6. https://doi.org/10.1001/jama.300.11.1311.
Akervall S, Al-Mukhtar Othman J, Molin M, Gyhagen M. Symptomatic pelvic organ prolapse in middle-aged women - a national matched cohort study on the influence of childbirth. Am J Obstet Gynecol. 2019. https://doi.org/10.1016/j.ajog.2019.10.007
Asresie A, Admassu E, Setegn T. Determinants of pelvic organ prolapse among gynecologic patients in Bahir Dar, north West Ethiopia: a case-control study. Int J Women's Health. 2016;8:713–9. https://doi.org/10.2147/ijwh.s122459.
Gyhagen M, Al-Mukhtar Othman J, Åkervall S, Nilsson I, Milsom I. The symptom of vaginal bulging in nulliparous women aged 25-64 years: a national cohort study. Int Urogynecol J. 2019;30(4):639–47. https://doi.org/10.1007/s00192-018-3684-5.
Henok A. Prevalence and factors associated with pelvic organ prolapse among pedestrian Back-loading women in bench Maji zone. Ethiop J Health Sci. 2017;27(3):263–72. https://doi.org/10.4314/ejhs.v27i3.8.
Løwenstein E, Ottesen B, Gimbel H. Incidence and lifetime risk of pelvic organ prolapse surgery in Denmark from 1977 to 2009. Int Urogynecol J. 2015;26(1):49–55. https://doi.org/10.1007/s00192-014-2413-y.
Masenga GG, Shayo BC, Rasch V. Prevalence and risk factors for pelvic organ prolapse in Kilimanjaro, Tanzania: a population based study in Tanzanian rural community. PLoS One. 2018;13(4):e0195910. https://doi.org/10.1371/journal.pone.0195910.
Risk factors for genital prolapse in non-hysterectomized women around menopause. Results from a large cross-sectional study in menopausal clinics in Italy. Progetto Menopausa Italia Study Group. Eur J Obstet Gynecol Reprod Biol. 2000;93(2):135-40.
Swift SE, Pound T, Dias JK. Case-control study of etiologic factors in the development of severe pelvic organ prolapse. Int Urogynecol J Pelvic Floor Dysfunct. 2001;12(3):187–92. https://doi.org/10.1007/s001920170062.
Tegerstedt G, Maehle-Schmidt M, Nyrén O, Hammarström M. Prevalence of symptomatic pelvic organ prolapse in a Swedish population. Int Urogynecol J Pelvic Floor Dysfunct. 2005;16(6):497–503. https://doi.org/10.1007/s00192-005-1326-1.
Vergeldt TF, Weemhoff M, IntHout J, Kluivers KB. Risk factors for pelvic organ prolapse and its recurrence: a systematic review. Int Urogynecol J. 2015;26(11):1559–73. https://doi.org/10.1007/s00192-015-2695-8.
Ismail SI, Bain C, Hagen S. Oestrogens for treatment or prevention of pelvic organ prolapse in postmenopausal women. Cochrane Database Syst Rev. 2010;(9):Cd007063. https://doi.org/10.1002/14651858.CD007063.pub2
Gedefaw G, Demis A. Burden of pelvic organ prolapse in Ethiopia: a systematic review and meta-analysis. BMC Womens Health. 2020;20(1):166. https://doi.org/10.1186/s12905-020-01039-w.
Gyhagen M, Al-Mukhtar Othman J, Akervall S, Nilsson I, Milsom I. The symptom of vaginal bulging in nulliparous women aged 25-64 years: a national cohort study. Int Urogynecol J. 2019;30(4):639–47. https://doi.org/10.1007/s00192-018-3684-5.
Lo TS, Jaili S, Uy-Patrimonio MC, Karim NB, Ibrahim R. Transvaginal management of severe pelvic organ prolapse in nulliparous women. J Obstet Gynaecol Res. 2017;43(3):543–50. https://doi.org/10.1111/jog.13234.
Norton P, Baker J, Sharp H, Warenski J. Genitourinary prolapse: relationship with joint mobility. Neurourol Urodynam. 1990;9:321–2.
Wan L, Liu X. Delayed-onset advanced pelvic organ prolapse after spinal cord injury in a young, nulliparous woman. Int Urogynecol J. 2016;27(5):825–7.
Dietz HP, Clarke B. Prevalence of rectocele in young nulliparous women. Aust N Z J Obstet Gynaecol. 2005;45(5):391–4.
Trowbridge ER, Wei JT, Fenner DE, Ashton-Miller JA, Delancey JO. Effects of aging on lower urinary tract and pelvic floor function in nulliparous women. Obstet Gynecol. 2007;109(3):715–20. https://doi.org/10.1097/01.aog.0000257074.98122.69.
Jundt K, Kiening M, Fischer P, et al. Is the histomorphological concept of the female pelvic floor and its changes due to age and vaginal delivery correct? Neurourol Urodyn. 2005;24(1):44–50. https://doi.org/10.1002/nau.20080.
Swenson CW, Masteling M, DeLancey JO, Nandikanti L, Schmidt P, Chen L. Aging effects on pelvic floor support: a pilot study comparing young versus older nulliparous women. Int Urogynecol J. 2019. https://doi.org/10.1007/s00192-019-04063-z
Raizada V, Mittal RK. Pelvic floor anatomy and applied physiology. Gastroenterol Clin N Am. 2008;37(3):493–509, vii. https://doi.org/10.1016/j.gtc.2008.06.003.
Dumoulin C, Pazzoto Cacciari L, Mercier J. Keeping the pelvic floor healthy. Climacteric. 2019;22(3):257–62. https://doi.org/10.1080/13697137.2018.1552934.
Smith P, Heimer G, Norgren A, Ulmsten U. Steroid hormone receptors in pelvic muscles and ligaments in women. Gynecol Obstet Investig. 1990;30(1):27–30. https://doi.org/10.1159/000293207.
Smith P, Heimer G, Norgren A, Ulmsten U. Localization of steroid hormone receptors in the pelvic muscles. Eur J Obstet Gynecol Reprod Biol. 1993;50(1):83–5. https://doi.org/10.1016/0028-2243(93)90169-d.
Rizk DE, Al-Marzouqi AH, Hassan HA, Al-Kedrah SS, Fahim MA. Estrogen and ghrelin decrease cytoplasmic expression of p27kip1, a cellular marker of ageing, in the striated anal sphincter and levator muscle of ovariectomized rats. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18(4):413–8. https://doi.org/10.1007/s00192-006-0159-x.
Lang JH, Zhu L, Sun ZJ, Chen J. Estrogen levels and estrogen receptors in patients with stress urinary incontinence and pelvic organ prolapse. Int J Gynaecol Obstet. 2003;80(1):35–9. https://doi.org/10.1016/s0020-7292(02)00232-1.
Delancey JO. Fascial and muscular abnormalities in women with urethral hypermobility and anterior vaginal wall prolapse. Am J Obstet Gynecol. 2002;187(1):93–8. https://doi.org/10.1067/mob.2002.125733.
Whiteside JL, Barber MD, Paraiso MF, Walters MD. Vaginal rugae: measurement and significance. Climacteric. 2005;8(1):71–5. https://doi.org/10.1080/13697130500042490.
Bodner-Adler B, Bodner K, Schneidinger C, et al. Pelvic organ prolapse and endogenous circulating sex steroids in postmenopausal women: a case control-study. Eur J Obstet Gynecol Reprod Biol. 2017;210:177–81. https://doi.org/10.1016/j.ejogrb.2016.12.027.
Moalli PA, Talarico LC, Sung VW, et al. Impact of menopause on collagen subtypes in the arcus tendineous fasciae pelvis. Am J Obstet Gynecol. 2004;190(3):620–7. https://doi.org/10.1016/j.ajog.2003.08.040.
Moalli PA, Shand SH, Zyczynski HM, Gordy SC, Meyn LA. Remodeling of vaginal connective tissue in patients with prolapse. Obstet Gynecol. 2005;106(5 Pt 1):953–63. https://doi.org/10.1097/01.AOG.0000182584.15087.dd.
Bales G, Chung D, Ballert K. Pelvic organ prolapse in older adults. Geriatric Urology Springer. 2014:181–206.
Wasenda EJ, Kamisan Atan I, Subramaniam N, Dietz HP. Pelvic organ prolapse: does hormone therapy use matter? Menopause. 2017;24(10):1185–9. https://doi.org/10.1097/gme.0000000000000898.
López-Otín C, Blasco MA, Partridge L, Serrano M, Kroemer G. The hallmarks of aging. Cell. 2013;153(6):1194–217.
Kirkwood TB. Understanding the odd science of aging. Cell. 2005;120(4):437–47.
Gavin A-C, Aloy P, Grandi P, et al. Proteome survey reveals modularity of the yeast cell machinery. Nature. 2006;440(7084):631–6.
Balch WE, Morimoto RI, Dillin A, Kelly JW. Adapting proteostasis for disease intervention. Science. 2008;319(5865):916–9.
Vulic M, Strinic T, Tomic S, Capkun V, Jakus IA, Ivica S. Difference in expression of collagen type I and matrix metalloproteinase-1 in uterosacral ligaments of women with and without pelvic organ prolapse. Eur J Obstet Gynecol Reproduct Biol. 2011;155(2):225–8.
Qiu J, Qin M, Fan B, Chen X. Klotho protein reduced the expression of matrix Metalloproteinase-1 (MMP-1) and matrix Metalloproteinase-3 (MMP-3) in fibroblasts from patients with pelvic organ prolapse (POP) by Down-regulating the phosphorylation of ERK1/2. Med Sci Monitor: Intl Med J Exp Clin Res. 2019;25:3815.
Kuro-o M, Matsumura Y, Aizawa H, et al. Mutation of the mouse klotho gene leads to a syndrome resembling ageing. Nature. 1997;390(6655):45–51.
Franceschi C, Bonafè M, Valensin S, et al. Inflamm-aging: an evolutionary perspective on immunosenescence. Ann N Y Acad Sci. 2000;908(1):244–54.
Franceschi C, Campisi J. Chronic inflammation (inflammaging) and its potential contribution to age-associated diseases. J Gerontol Ser A: Biomed Sci Med Sci. 2014;69(Suppl_1):S4–9.
Narita M, Nuñez S, Heard E, et al. Rb-mediated heterochromatin formation and silencing of E2F target genes during cellular senescence. Cell. 2003;113(6):703–16.
Dimri GP, Lee X, Basile G, et al. A biomarker that identifies senescent human cells in culture and in aging skin in vivo. Proc Natl Acad Sci. 1995;92(20):9363–7.
Takahashi A, Ohtani N, Yamakoshi K, et al. Mitogenic signalling and the p16 INK4a–Rb pathway cooperate to enforce irreversible cellular senescence. Nat Cell Biol. 2006;8(11):1291–7.
Freund A, Orjalo AV, Desprez P-Y, Campisi J. Inflammatory networks during cellular senescence: causes and consequences. Trends Mol Med. 2010;16(5):238–46.
Salvioli S, Monti D, Lanzarini C, et al. Immune system, cell senescence, aging and longevity-inflamm-aging reappraised. Curr Pharm Des. 2013;19(9):1675–9.
Huang L, Zhao Z, Wen J, Ling W, Miao Y, Wu J. Cellular senescence: a pathogenic mechanism of pelvic organ prolapse. Mol Med Rep. 2020;22(3):2155–62.
Kim EJ, Chung N, Park SH, et al. Involvement of oxidative stress and mitochondrial apoptosis in the pathogenesis of pelvic organ prolapse. J Urol. 2013;189(2):588–94.
Li B, Hong L, Min J, Wu D, Hu M, Guo W. The expression of glutathione peroxidase-1 and the anabolism of collagen regulation pathway transforming growth factor-beta1-connective tissue growth factor in women with uterine prolapse and the clinic significance. Clin Exp Obstet Gynecol. 2013;40(4):586–90.
Belayneh T, Gebeyehu A, Adefris M, Rortveit G, Awoke T. Pelvic organ prolapse in Northwest Ethiopia: a population-based study. Int Urogynecol J. 2019:1–9.
Min J, Li B, Liu C, et al. Extracellular matrix metabolism disorder induced by mechanical strain on human parametrial ligament fibroblasts. Mol Med Rep. 2017;15(5):3278–84.
Kufaishi H, Alarab M, Drutz H, Lye S, Shynlova O. Static mechanical loading influences the expression of extracellular matrix and cell adhesion proteins in vaginal cells derived from premenopausal women with severe pelvic organ prolapse. Reprod Sci. 2016;23(8):978–92.
Zhang Q, Liu C, Hong S, et al. Excess mechanical stress and hydrogen peroxide remodel extracellular matrix of cultured human uterosacral ligament fibroblasts by disturbing the balance of MMPs/TIMPs via the regulation of TGF-β1 signaling pathway. Mol Med Rep. 2017;15(1):423–30.
Usta A, Guzin K, Kanter M, Ozgül M, Usta CS. Expression of matrix metalloproteinase-1 in round ligament and uterosacral ligament tissue from women with pelvic organ prolapse. J Mol Histol. 2014;45(3):275–81.
Li BS, Guo WJ, Hong L, et al. Role of mechanical strain-activated PI3K/Akt signaling pathway in pelvic organ prolapse. Mol Med Rep. 2016;14(1):243–53.
Kawabata H, Katsura T, Kondo E, et al. Stress deprivation from the patellar tendon induces apoptosis of fibroblasts in vivo with activation of mitogen-activated protein kinases. J Biomech. 2009;42(15):2611–5.
Fernando R, Drescher C, Nowotny K, Grune T, Castro JP. Impaired proteostasis during skeletal muscle aging. Free Radic Biol Med. 2019;132:58–66.
Van Kan GA. Epidemiology and consequences of sarcopenia. JNHA-J Nutri Health Aging. 2009;13(8):708–12.
Larsson L, Degens H, Li M, et al. Sarcopenia: aging-related loss of muscle mass and function. Physiol Rev. 2019;99(1):427–511.
Alnaqeeb M, Al Zaid N, Goldspink G. Connective tissue changes and physical properties of developing and ageing skeletal muscle. J Anat. 1984;139(Pt 4):677.
Prado LG, Makarenko I, Andresen C, Krüger M, Opitz CA, Linke WA. Isoform diversity of giant proteins in relation to passive and active contractile properties of rabbit skeletal muscles. J Gen Physiol. 2005;126(5):461–80.
Alperin M, Cook M, Tuttle LJ, Esparza MC, Lieber RL. Impact of vaginal parity and aging on the architectural design of pelvic floor muscles. Am J Obstet Gynecol. 2016;215(3):312. e1–9.
Cook MS, Bou-Malham L, Esparza MC, Alperin M. Age-related alterations in female obturator internus muscle. Int Urogynecol J. 2017;28(5):729–34.
Fulop T, Larbi A, Kotb R, de Angelis F, Pawelec G. Aging, immunity, and cancer. Discov Med. 2011;11(61):537–50.
Agarwal S, Busse PJ. Innate and adaptive immunosenescence. Ann Allergy Asthma Immunol. 2010;104(3):183–90.
Verdú E, Ceballos D, Vilches JJ, Navarro X. Influence of aging on peripheral nerve function and regeneration. J Peripher Nerv Syst. 2000;5(4):191–208.
Wang Y-J, Zhou C-J, Shi Q, Smith N, Li T-F. Aging delays the regeneration process following sciatic nerve injury in rats. J Neurotrauma. 2007;24(5):885–94.
Bokov A, Chaudhuri A, Richardson A. The role of oxidative damage and stress in aging. Mech Ageing Dev. 2004;125(10-11):811–26.
Garbay B, Heape A, Sargueil F, Cassagne C. Myelin synthesis in the peripheral nervous system. Prog Neurobiol. 2000;61(3):267–304.
Blair IA. Lipid hydroperoxide-mediated DNA damage. Exp Gerontol. 2001;36(9):1473–81.
Opalach K, Rangaraju S, Madorsky I, Leeuwenburgh C, Notterpek L. Lifelong calorie restriction alleviates age-related oxidative damage in peripheral nerves. Rejuvenation Res. 2010;13(1):65–74.
SHERMAN BM, WEST JH, KORENMAN SG. The menopausal transition: analysis of LH, FSH, estradiol, and progesterone concentrations during menstrual cycles of older women. J Clin Endoc Metab. 1976;42(4):629–36.
Fuentes N, Silveyra P. Estrogen receptor signaling mechanisms. Advances in protein chemistry and structural biology. Elsevier; 2019:135-170.
Simpson E, Santen RJ. Celebrating 75 years of oestradiol. J Mol Endocrinol. 2015;55(3):T1.
Samavat H, Kurzer MS. Estrogen metabolism and breast cancer. Cancer Lett. 2015;356(2 Pt A):231–43. https://doi.org/10.1016/j.canlet.2014.04.018.
Blair IA. Analysis of estrogens in serum and plasma from postmenopausal women: past present, and future. Steroids. 2010;75(4-5):297–306. https://doi.org/10.1016/j.steroids.2010.01.012.
Bai SW, Chung DJ, Yoon JM, Shin JS, Kim SK, Park KH. Roles of estrogen receptor, progesterone receptor, p53 and p21 in pathogenesis of pelvic organ prolapse. Int Urogynecol J Pelvic Floor Dysfunct. 2005;16(6):492–6. https://doi.org/10.1007/s00192-005-1310-9.
Hendrix SL, Cochrane BB, Nygaard IE, et al. Effects of estrogen with and without progestin on urinary incontinence. Jama. 2005;293(8):935–48. https://doi.org/10.1001/jama.293.8.935.
Mokrzycki ML, Mittal K, Smilen SW, Blechman AN, Porges RF, Demopolous RI. Estrogen and progesterone receptors in the uterosacral ligament. Obstet Gynecol. 1997;90(3):402–4. https://doi.org/10.1016/s0029-7844(97)00285-8.
Cox DA, Helvering LM. Extracellular matrix integrity: a possible mechanism for differential clinical effects among selective estrogen receptor modulators and estrogens? Mol Cell Endocrinol. 2006;247(1-2):53–9.
Moalli PA, Debes KM, Meyn LA, Howden NS, Abramowitch SD. Hormones restore biomechanical properties of the vagina and supportive tissues after surgical menopause in young rats. Am J Obstet Gynecol. 2008;199(2):161. e1–8.
Moalli P, Talarico L, Sung V, et al. Impact of menopause on collagen subtypes in the arcus tendineous fasciae pelvis. Am J Obstet Gynecol. 2004;190(3):620–7.
Zong W, Zyczynski HM, Meyn LA, Gordy SC, Moalli PA. Regulation of MMP-1 by sex steroid hormones in fibroblasts derived from the female pelvic floor. Am J Obstet Gynecol. 2007;196(4):349. e1–349. e11.
Zong W, Meyn LA, Moalli PA. The amount and activity of active matrix metalloproteinase 13 is suppressed by estradiol and progesterone in human pelvic floor fibroblasts. Biol Reprod. 2009;80(2):367–74.
Zong W, Jallah ZC, Stein SE, Abramowitch SD, Moalli PA. Repetitive mechanical stretch increases extracellular collagenase activity in vaginal fibroblasts. Female Pelvic Med Reconstr Surg. 2010;16(5):257.
Ulrich D, Edwards SL, Su K, et al. Influence of reproductive status on tissue composition and biomechanical properties of ovine vagina. PLoS One. 2014;9(4):e93172.
Wagenseil JE, Mecham RP. New insights into elastic fiber assembly. Birth Defects Res Part C: Embryo Today: Revi. 2007;81(4):229–40.
Papke CL, Yanagisawa H. Fibulin-4 and fibulin-5 in elastogenesis and beyond: insights from mouse and human studies. Matrix Biol. 2014;37:142–9.
Drewes PG, Yanagisawa H, Starcher B, et al. Pelvic organ prolapse in fibulin-5 knockout mice: pregnancy-induced changes in elastic fiber homeostasis in mouse vagina. Am J Pathol. 2007;170(2):578–89. https://doi.org/10.2353/ajpath.2007.060662.
Liu X, Zhao Y, Pawlyk B, Damaser M, Li T. Failure of elastic fiber homeostasis leads to pelvic floor disorders. Am J Pathol. 2006;168(2):519–28. https://doi.org/10.2353/ajpath.2006.050399.
Alarab M, Bortolini MA, Drutz H, Lye S, Shynlova O. LOX family enzymes expression in vaginal tissue of premenopausal women with severe pelvic organ prolapse. Int Urogynecol J. 2010;21(11):1397–404. https://doi.org/10.1007/s00192-010-1199-9.
Shynlova O, Bortolini MA, Alarab M. Genes responsible for vaginal extracellular matrix metabolism are modulated by women's reproductive cycle and menopause. Int Braz J Urol. 2013;39(2):257–67. https://doi.org/10.1590/s1677-5538.ibju.2013.02.15.
Zhao BH, Zhou JH. Decreased expression of elastin, fibulin-5 and lysyl oxidase-like 1 in the uterosacral ligaments of postmenopausal women with pelvic organ prolapse. J Obstet Gynaecol Res. 2012;38(6):925–31. https://doi.org/10.1111/j.1447-0756.2011.01814.x.
Pascual G, Mendieta C, Mecham RP, Sommer P, Bellón JM, Buján J. Down-regulation of lysyl oxydase-like in aging and venous insufficiency. Histol Histopathol. 2008;23(2):179–86. https://doi.org/10.14670/hh-23.179.
Matthews J, Gustafsson JA. Estrogen signaling: a subtle balance between ER alpha and ER beta. Mol Interv. 2003;3(5):281–92. https://doi.org/10.1124/mi.3.5.281.
Levin ER. Integration of the extranuclear and nuclear actions of estrogen. Mol Endocrinol. 2005;19(8):1951–9. https://doi.org/10.1210/me.2004-0390.
Curtis SW, Washburn T, Sewall C, et al. Physiological coupling of growth factor and steroid receptor signaling pathways: estrogen receptor knockout mice lack estrogen-like response to epidermal growth factor. Proc Natl Acad Sci U S A. 1996;93(22):12626–30. https://doi.org/10.1073/pnas.93.22.12626.
Ignar-Trowbridge DM, Pimentel M, Parker MG, McLachlan JA, Korach KS. Peptide growth factor cross-talk with the estrogen receptor requires the a/B domain and occurs independently of protein kinase C or estradiol. Endocrinology. 1996;137(5):1735–44. https://doi.org/10.1210/endo.137.5.8612509.
Zhao C, Matthews J, Tujague M, et al. Estrogen receptor beta2 negatively regulates the transactivation of estrogen receptor alpha in human breast cancer cells. Cancer Res. 2007;67(8):3955–62. https://doi.org/10.1158/0008-5472.can-06-3505.
Goldstein SR, Nanavati N. Adverse events that are associated with the selective estrogen receptor modulator levormeloxifene in an aborted phase III osteoporosis treatment study. Am J Obstet Gynecol. 2002;187(3):521–7. https://doi.org/10.1067/mob.2002.123938.
Albertazzi P, Sharma S. Urogenital effects of selective estrogen receptor modulators: a systematic review. Climacteric. 2005;8(3):214–20. https://doi.org/10.1080/13697130500117946.
Goldstein SR, Johnson S, Watts NB, Ciaccia AV, Elmerick D, Muram D. Incidence of urinary incontinence in postmenopausal women treated with raloxifene or estrogen. Menopause. 2005;12(2):160–4. https://doi.org/10.1097/00042192-200512020-00010.
Acknowledgments
We thank Dr. Rufus Cartwright, Dr. Maria Gyhagen, and Dr. Ian Milson for their contribution to revising this manuscript and giving significant input.
Funding
Grant 2019/26723-5, São Paulo Research Foundation (FAPESP).
Author information
Authors and Affiliations
Contributions
AY Weintraub, J Deprest: Project development, manuscript editing, and approval of the final manuscript.
J Manonai, P Moalli, O Shynlova: Manuscript editing and approval of the final manuscript.
LGO Brito, GMV Pereira, MA Bortolini: Project development, data management and analysis, manuscript editing, and approval of the final manuscript.
Corresponding author
Ethics declarations
Conflict of interests
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Brito, L.G.O., Pereira, G.M.V., Moalli, P. et al. Age and/or postmenopausal status as risk factors for pelvic organ prolapse development: systematic review with meta-analysis. Int Urogynecol J 33, 15–29 (2022). https://doi.org/10.1007/s00192-021-04953-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-021-04953-1