Abstract
Introduction and hypothesis
We aimed to investigate the prevalence and risk factors of symptomatic pelvic organ prolapse (POP) in rural China.
Methods
A cross-sectional study of POP was conducted in rural China from February 2014 to March 2016. In total, 25,864 rural women were recruited. All were asked to complete a questionnaire that included questions about their age, job, parity, diseases, and so on. Symptomatic POP was assessed using Pelvic Organ Prolapse Quantification (POP-Q) system staging and validation questionnaires. Multivariate logistic regression was used to assess the factors associated with symptomatic POP.
Results
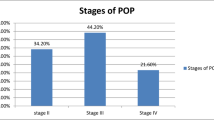
The prevalence of symptomatic POP was 9.10%. There was a consistent trend toward an increasing prevalence of POP with increasing age, ranging from 2.53 to 13.40% (P < 0.0001). Women aged 50–59 years [adjusted odds ratio (AOR) 1.86, 95% confidence interval (CI) 1.46–2.37] were more likely to have POP than women aged 20–29 years. POP was positively associated with giving birth to more than three children (AOR 2.18, 95% CI 1.88–2.43). Cesarean section was a significant protective factor (AOR = 0.34, 95% CI 0.33-0.49) compared with vaginal delivery. Multivariate logistic regression analysis showed that obesity, constipation, smoking, coughing, gynecological diseases, and other physical diseases were also associated with POP.
Conclusions
Symptomatic POP affects a substantial proportion of women in rural China. Older age, multiparity, vaginal delivery, obesity, and many chronic conditions significantly increased the odds of developing symptomatic POP. Additional healthcare campaigns are needed to educate women in rural areas about POP.

Similar content being viewed by others
Abbreviations
- POP:
-
Pelvic organ prolapse
- POP-Q:
-
Pelvic Organ Prolapse Quantification
- AOR:
-
Adjusted odds ratio
- CIs:
-
Confidence intervals
- BMI:
-
Body mass index
References
Masenga GG, Shayo BC, Rasch V. Prevalence and risk factors for pelvic organ prolapse in Kilimanjaro, Tanzania: a population based study in Tanzanian rural community. PLoS One. 2018;13(4):e0195910. https://doi.org/10.1371/journal.pone.0195910.
Zeleke BM, Bell RJ, Billah B, Davis SR. Symptomatic pelvic floor disorders in community-dwelling older Australian women. Maturitas. 2016;85:34–41. https://doi.org/10.1016/j.maturitas.2015.12.012.
Walker GJ, Gunasekera P. Pelvic organ prolapse and incontinence in developing countries: review of prevalence and risk factors. Int Urogynecol J. 2011;22(2):127–35. https://doi.org/10.1007/s00192-010-1215-0.
Chow D, Rodriguez LV. Epidemiology and prevalence of pelvic organ prolapse. Curr Opin Urol. 2013;23(4):293–8. https://doi.org/10.1097/MOU.0b013e3283619ed0.
Swift SE. The distribution of pelvic organ support in a population of female subjects seen for routine gynecologic health care. Am J Obstet Gynecol. 2000;183(2):277–85.
Li J, Shi L, Liang H, Ding G, Xu L. Urban-rural disparities in health care utilization among Chinese adults from 1993 to 2011. BMC Health Serv Res. 2018;18(1):102.
Zhang C, Tong J, Zhu L, Zhang L, Xu T, Lang J, et al. A population-based epidemiologic study of female sexual dysfunction risk in mainland China: prevalence and predictors. J Sex Med. 2017;14(11):1348.
Lembo A, Camilleri M. Chronic constipation. N Engl J Med. 2003;349(14):1360–8.
Luo J. Reliability and validity of Chinese version of pelvic floor distress questionnaires. [Doctoral dissertation. Fujian medical University] 2014. (in Chinese).
Ellerkmann RM, Cundiff GW, Melick CF, Nihira MA, Leffler K, Bent AE. Correlation of symptoms with location and severity of pelvic organ prolapse. Am J Obstet Gynecol. 2001;185(6):1332–7; discussion 1337-1338. https://doi.org/10.1067/mob.2001.119078.
Swift SE. The distribution of pelvic organ support in a population of female subjects seen for routine gynecologic health care. Am J Obstet Gynecol. 2000;183(2):277–85. https://doi.org/10.1067/mob.2000.107583.
Trowbridge ER, Fultz NH, Patel DA, DeLancey JO, Fenner DE. Distribution of pelvic organ support measures in a population-based sample of middle-aged, community-dwelling African American and white women in southeastern Michigan. Am J Obstet Gynecol. 2008;198(5):548.e1–6.
Li L, Wu J, Pu D, Zhao Y, Wan C, Sun L, et al. Factors associated with the age of natural menopause and menopausal symptoms in Chinese women. Maturitas. 2012;73(4):354–60. https://doi.org/10.1016/j.maturitas.2012.09.008.
Akter F, Gartoulla P, Oldroyd J, Islam RM. Prevalence of, and risk factors for, symptomatic pelvic organ prolapse in rural Bangladesh: a cross-sectional survey study. Int Urogynecol J. 2016;27(11):1753–9. https://doi.org/10.1007/s00192-016-3038-0.
Liu X, Li N, Liu C, Ren X, Liu D, Gao B, et al. Urban-rural disparity in utilization of preventive care services in China. Medicine (Baltimore). 2016;95(37):e4783.
Elnicki DM, Morris DK, Shockcor WT. Patient-perceived barriers to preventive health care among indigent, rural Appalachian patients. Arch Intern Med. 1995;155(4):421–4.
Elbiss HM, Osman N, Hammad FT. Prevalence, risk factors and severity of symptoms of pelvic organ prolapse among Emirati women. BMC Urol. 2015;15:66.
Islam RM, Bell RJ, Billah B, Hossain MB, Davis SR. The prevalence of symptomatic pelvic floor disorders in women in Bangladesh. Climacteric. 2016;19(6):558–64. https://doi.org/10.1080/13697137.2016.1240771.
Younis N, ., Khattab H, ., Zurayk H, ., El-Mouelhy M, ., Amin MF, Farag AM (1993) A community study of gynecological and related morbidities in rural Egypt. Stud Fam Plan 24 (3):175-186.
Garshasbi A, Faghih-Zadeh S, Falah N. The status of pelvic supporting organs in a population of iranian women 18 - 68 years of age and possible related factors. Arch Iran Med. 2006;9(2):124–8.
Lloyd CB, Adetunji JA, Ali MM, Cleland J, Johnson K, Clark SJ, et al. (2011) Nepal demographic and health survey 2006. Kathmandu Nepal Ministry of Health & Population Population Division 7 (2):592-599.
Ramalingam K, Monga A. Obesity and pelvic floor dysfunction. Best Pract Res Clin Obstet Gynaecol. 2015;29(4):541–7. https://doi.org/10.1016/j.bpobgyn.2015.02.002.
Wu JM, Vaughan CP, Goode PS, Redden DT, Burgio KL, Richter HE, et al. Prevalence and trends of symptomatic pelvic floor disorders in U.S. women. Obstet Gynecol. 2014;123(1):141–8.
Spence-Jones C, Kamm MA, Henry MM, Hudson CN. Bowel dysfunction: a pathogenic factor in uterovaginal prolapse and urinary stress incontinence. Br J Obstet Gynaecol. 1994;101(2):147–52.
Nygaard IE, Shaw JM. Physical activity and the pelvic floor. Am J Obstet Gynecol. 2016;214(2):164–71.
Woodman PJ, Swift SE, O’Boyle AL, Valley MT, Bland DR, Kahn MA, et al. Prevalence of severe pelvic organ prolapse in relation to job description and socioeconomic status: a multicenter cross-sectional study. Int Urogynecol J Pelvic Floor Dysfunct. 2006;17(4):340–5. https://doi.org/10.1007/s00192-005-0009-2.
Acknowledgments
This study obtained ethical approval from clinical trials.gov and http://www.chictr.org.cn (number: ChiCTR-OCH-14004675). Written consent was obtained from all eligible participants. All eligible patients were invited to participate in the study, and those who agreed were provided with a written informed consent form to sign. Ethical approval for the research was sought and obtained from the Research Ethical Committee at the Peking Union Medical College Hospital in 2014.
Funding
This study was funded by the CAMS Initiative for Innovative Medicine (CAMS-I2 M; 2017-I2 M-1-002).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Li, Z., Xu, T., Li, Z. et al. An epidemiologic study of pelvic organ prolapse in rural Chinese women: a population-based sample in China. Int Urogynecol J 30, 1925–1932 (2019). https://doi.org/10.1007/s00192-018-03859-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-018-03859-9