Abstract
Purpose
To assess the epidemiology of intensive care unit (ICU) patients with thrombocytopenia (TP).
Methods
All consecutive ICU-admitted patients with TP either on admission or acquired during ICU stay were included. TP was defined as either absolute (platelet count <100 × 109/L) or relative (decrease in the platelet count >30 %). Extensive diagnostic workup of TP including bone marrow aspiration was performed.
Results
Absolute TP was diagnosed in 208 patients and relative TP in 93. In six patients (2 %), no cause of TP was identified. The median number of TP etiologies per patient was two, with sepsis being the leading cause. Bone marrow aspirates were analyzed in 238 patients. They showed a normal megakaryocyte number in 221 (93 %) and provided novel information for diagnosis in 52 (22 %). Results were susceptible to having an impact on patient management in 22 cases (11 %). The frequency of bone marrow aspiration with results susceptible to having an impact on management did not differ between patients with and without disseminated intravascular coagulation (P = 0.22) and with and without sepsis/septic shock (P = 0.7) but was significantly lower in patients with relative TP than in those with absolute TP (P < 0.01). A serious bleeding event was observed in 30 patients (14.9 %) and a nadir platelet count below 50 × 109/L was an independent risk factor (P < 0.05).
Conclusions
In thrombocytopenic patients, sepsis is the leading cause of TP. Bone marrow aspirates may yield significant information on TP mechanisms and contribute to the subsequent management of patients, especially those with absolute TP.
Similar content being viewed by others
Introduction
Thrombocytopenia (TP) is a common laboratory finding in intensive care unit (ICU) patients. A 150 × 109/L threshold is used in most studies to define TP [1–11] but its definition varies and some authors use other cut-offs such as 100 × 109/L [12–17], 50 × 109/L [18, 19], and 30 × 109/L [20]. In addition, most studies do not include a repeat platelet count to confirm TP, thereby limiting the accuracy of TP diagnosis [5, 6, 18]. Depending on the definition of TP, the clinical setting, and the case mix population, the frequency ranges from 8.3 to 67.6 % for prevalent TP (TP diagnosed on ICU admission) and from 13.0 to 44.1 % for incident TP (TP acquired during ICU stay) [21]. The causes of TP in critically ill patients are usually multifactorial and mainly result from enhanced platelet consumption, reduced platelet production, hemodilution, or a combination of any of these mechanisms. However, to our knowledge, very few studies have extensively assessed the causes of TP [6, 16].
Several works have addressed the consequences of TP as a determinant of severe bleeding [3, 5, 6, 18] but with conflicting results [3, 18]. Platelet count nadir and kinetics have been reported to be associated with adverse outcome in ICU patients [3, 4, 22–24]. The consequences of TP in critically ill patients are uncertain and hence its management remains unresolved.
We decided, therefore, to assess the epidemiology of ICU thrombocytopenic patients. We focused on TP etiologies by performing an extensive diagnostic workup that included bone marrow aspiration.
Patients and methods
Study population
This prospective observational study was carried out between July 2005 and November 2006. One medical and two mixed ICUs in a university hospital and two mixed ICUs in general hospitals took part. Patients older than 18 years who presented with TP either on admission or during ICU stay were included. Exclusion criteria included pregnancy and an ICU length of stay less than 48 h. In all patients, platelet counts were performed daily from ICU admission to ICU discharge. The study protocol was approved by the institutional ethics committee. Informed consent was required from the patients or their next of kin.
Study protocol
The day of inclusion was the day of TP diagnosis. On inclusion, the following tests were performed and their results collected: activated partial thromboplastin time (aPTT), prothrombin time (PT), expressed as a percentage of the ratio of the PT in patients over the PT in controls (STA NEOPLASTINE CI PLUS; Diagnostica Stago, France), plasma level measurement of D-dimer (VIDAS D-dimer, BioMerieux, France), fibrinogen (STA FIBRINOGEN; Diagnostica Stago, France), serum level measurement of creatinine, ferritin, triglyceride, bilirubin, haptoglobin, lactate dehydrogenase (LDH), aspartate aminotransferase (ASAT), alanine aminotransferase (ALAT), vitamin B12, folic acid, and antibodies against Epstein–Barr virus (EBV) cytomegalovirus (CMV), human immunodeficiency virus (HIV), and B and C hepatitis using enzyme-linked immunosorbent assay (ELISA) techniques. A platelet antibody test was performed in patients who had had platelet transfusion administered within the 3 weeks before inclusion. In patients with previous heparin exposure and an intermediate or high suspicion of heparin-induced TP (HIT) as defined by a 4-T score greater than 3 [25], a PF4/heparin ELISA was carried out and when PF4/heparin antibodies were detected, a heparin-induced platelet activation test was performed. Bone marrow aspiration was performed and all aspirates were reviewed by an experienced hematologist. Daily platelet counts from inclusion to 14 days after inclusion or until ICU discharge if patients were discharged earlier were also recorded. The other data collected are given in Supplemental File 1.
Definitions
Absolute TP was defined by a platelet count below 100 × 109/L [12, 17] and relative TP by a decrease in the platelet count of more than 30 % [6] as compared with the highest values of the platelet counts observed within the preceding 4 days in patients without absolute TP. TP was confirmed using a subsequent platelet count control performed within the following 24 h. Patients with relative TP who developed absolute TP during their ICU stays were allocated to the absolute TP group.
A serious bleeding event (SBE) was defined by at least one of the following criteria: central nervous system hemorrhage, blood loss requiring the transfusion of three or more units of red blood cells (RBCs) in a 48-h period, bleeding requiring surgery or endoscopy, or fatal bleeding [26]. All other bleeding events were considered to be of minor importance.
Other definitions used are given in Supplemental File 2 [27–33].
Statistical analysis
Data were entered onto a computer and analyzed using Epi-info version 6 (Center for Disease Control, Atlanta, GA, USA) and Statview 5.0 statistical packages (SAS Institute Inc., SAS Campus Drive, Cary, NC 27515, USA). Values are expressed as mean ± SD or median and IQR or as a percentage of the group from which they were derived (categorical variables). Categorical data were compared using the χ 2 test or Fisher exact test, as appropriate. Continuous variables were compared using the Student’s t test or Mann–Whitney U test when appropriate. The nadir platelet count taken into account in the models was the lowest platelet count during ICU stay in patients without severe bleeding events and the lowest platelet count prior to the occurrence of SBE in the others. In patients who were administered prophylactic platelet transfusion, the nadir platelet count value entered in the model was the platelet count at the time of the first platelet transfusion. The risk of the first SBE was assessed in patients who did not receive prophylactic platelet transfusion by a logistic regression model. The relationships between hospital mortality and the study variables were assessed using a logistic regression model in which vital status at hospital discharge was the variable of interest. Variables with P < 0.20 by univariate analysis were entered into the logistic regression model, where they were kept if the P value in the multivariable context was less than 0.05 (stepwise variable-selection method). All statistical tests were two-tailed, and P values less than 0.05 were considered to be significant.
Results
Population
Of the 301 patients who met the inclusion criteria, 208 were diagnosed with absolute TP and 93 with relative TP (Supplemental File 3). The characteristics of the population are shown in Table 1. A total of 208 patients presented with absolute TP diagnosed either on admission (N = 102) or during ICU stay (N = 106). In the latter 106 patients, absolute TP developed at a median time of 3 days (IQR = 2–4) after ICU admission. Relative TP was ultimately diagnosed in 93 patients and developed at a median time of 4 days (IQR = 3–5) after ICU admission. The median duration of TP during the first 14 days following TP diagnosis was 4 days (IQR = 2–7) in patients with absolute TP. The daily platelet counts in the 14 days following TP diagnosis in patients with absolute and relative TP are given in Supplemental File 4.
Medical conditions associated with TP
The median number of TP etiologies per patient was two (Table 2). Multiple causes of TP were more frequently observed in patients with absolute TP. Infections (sepsis/severe sepsis and septic shock) were the leading medical condition associated with TP. The sites of infection and etiologic microorganisms are shown in Supplemental File 5. Viral diagnostic workup was performed in 261 patients (87 %) and identified 69 viral infection-associated TP in 62 (24 %), due to EBV in 33 cases, CMV in 21, hepatitis B in 5, hepatitis C in 7, and HIV in 3. In 2 patients viral infection was the only medical condition associated with TP. In the 123 patients with DIC, infection was the main cause in 92 (75 %), followed by massive transfusion in 17 (7 %) and cancer in 6 (5 %). Of the 32 patients with drug-induced TP, 14 (44 %) had no other identified cause. In 169/301 patients (56 %), prior heparin exposure was present before TP diagnosis, including unfractionated heparin in 87 patients and low molecular weight heparin in 82. A diagnostic procedure for HIT was performed in 70 patients (41 %): heparin-PF4 immunoassay in all patients, and functional assay in 20 patients. The diagnosis of HIT was ultimately considered in 5/169 patients (3 %). Hemophagocytic syndrome was diagnosed in 14 patients, of whom 5 had at least five diagnostic criteria and the other 9 four criteria.
Bone marrow aspiration
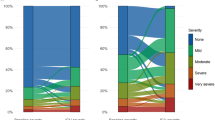
Bone marrow samples were taken in 255 patients and could be analyzed in 238. No complications were observed after aspiration. Decreased platelet production was observed in 17 cases (7 %). A total of 102 pathologic findings were identified in 44 % (71/163) of patients with absolute TP and in 28 % (21/75) of patients with relative TP (P = 0.03). In 54 patients, cytological signs like those classically described in patients with vitamin B12 or folate deficiencies were observed on bone marrow aspirates but were associated with serum vitamin deficiency in only 25. There was no relationship between vitamin deficiency and the presence of cytological signs (P = 0.22). However, megaloblastosis was more frequently observed in patients with than without vitamin deficiency (P = 0.02). In 52 (22 %) of the 238 patients with analyzable results, bone marrow aspirates yielded a positive diagnosis not previously established. Results of bone marrow aspirates yielding a previously unestablished diagnosis were observed in 24/96 patients (25 %) with DIC and in 28/142 (20 %) without (P = 0.40), in 39/182 patients (21 %) with sepsis and/or septic shock and in 13/56 (23 %) without (P = 0.9), and in 40/163 patients (25 %) with absolute TP and 12/75 (16 %) with relative TP (P = 0.19). A diagnosis established on the basis of bone marrow results and susceptible to having a significant impact on subsequent patient management was observed in 24 cases (11 %). Results of bone marrow aspirates susceptible to having a significant impact on subsequent patient management were observed in 13/96 patients (14 %) with DIC and in 11/142 (8 %) without (P = 0.22), in 17/182 patients (9 %) with sepsis and/or septic shock and in 7/56 patients (13 %) without (P = 0.7), and in 14 % of the patients (23/163) with absolute TP vs 1 % with relative TP (1/75), P < 0.01. The results of bone marrow examination are shown in Table 3 and examples of bone marrow smears are shown in Fig. 1.
Outcome
A total of 44 patients received platelet transfusions during their stay and were therefore excluded from the analysis of risk factors of SBEs. None of them developed SBEs. In the 257 other patients, 38 episodes of SBE were observed in 30 patients. The median nadir platelet count was 44 × 109/L (27–69) in the 30 patients with SBE and 85 × 109/L (56–132) in the 227 patients without (P < 0.0001). SBE was observed in 30 % (26/164) of patients with absolute TP and in 4 % (4/93) with relative (P = 0.01). The incidence of patients developing SBE according to nadir platelet count was 28 % (5/18), 24 % (11/46), 10 % (10/104), and 4 % (4/89) (P = 0.001) for counts of less than 20 × 109/L, between 20 and 49 × 109/L, between 50 and 99 × 109/L, and at least 100 × 109/L, respectively (Fig. 2). In multivariate analysis a nadir platelet count below 50 × 109/L was an independent risk factor of SBEs (P < 0.05) (Supplemental Files 6a and 6b). Transfusion requirements are summarized in Supplemental File 7. Bleeding was the immediate cause of death in four patients with absolute TP. The ICU mortality of thrombocytopenic patients with a nadir platelet count between 50 and 99 × 109/L, between 20 and 49 × 109/L, and at most 20 × 109/L was 22 % (24/109), 43 % (29/67), and 61 % (22/36) (P = 0.009), respectively; the corresponding values for hospital mortality were 30 % (33/109), 52 % (35/67), and 67 % (24/36), respectively (P = 0.01). According to our definitions, the type of TP, absolute or relative, was not associated with ICU and hospital mortality. High SAPS II score, SBE, septic shock, and hemophagocytic syndrome were associated with hospital mortality in multivariate analysis (Supplemental File 8).
Discussion
Our study is one of the largest on the epidemiology and outcome of thrombocytopenic patients in the ICU setting [3–8, 11, 12, 16–18]. Another major strength of the study is its design. It was a prospective multicenter study in which there was a systematic search for causes of TP in critically ill patients. It also includes the largest number of bone marrow examinations in ICU thrombocytopenic patients performed so far.
Very few data are currently available on bone marrow aspiration results in ICU patients. Two large prospective studies have been performed but included fewer than 50 bone marrow aspirates in septic patients and focused on hemophagocytosis [34, 35]. In other studies bone marrow aspiration was only performed for unexplained TP [12, 17]. In one retrospective study, aspiration was performed in 18/38 thrombocytopenic patients and revealed a decrease in megakaryocytes in 4, but in only 1 did it yield a new diagnosis [12]. In one prospective study, aspiration was performed in 12/52 patients and identified TP etiology in 10 cases [17]. In our work, bone marrow aspiration was performed even when an evident cause of TP was present. Our study suggests that, in a mixed ICU population, TP is rarely due to a decline in platelet medullar production. It added significant information in 22 % of our patients by yielding a diagnosis not previously established. Since we did not record when bone marrow aspiration was performed to exclude a suspected diagnosis, its diagnostic contribution in thrombocytopenic patients could not be accurately measured. However, our study suggests, firstly, that the presence of DIC and sepsis are not sufficient criteria to not perform bone aspiration, particularly in patients with absolute TP, and, secondly, that the results of aspiration performed to assess TP mechanisms in relative TP have such a low impact on management that the procedure can be dispensed with.
Cytological signs suggesting vitamin B12/folate deficiency were observed on bone marrow slides but were not correlated with actual B12/folate deficiency shown by the results of assays. This discrepancy could be related to deficiencies in vitamin B1, vitamin D, and vitamin E or copper [36], which were not measured in our study. Also, we cannot rule out the possibility that in some patients with actual B12 and folate deficiency prior to supplementation the cytological abnormalities of B12 folate deficiency may have persisted. In contrast, the relative rarity of these morphological abnormalities in patients with actual vitamin B12/folate deficiencies could be related to the introduction of automated immunoassays, which yielded an earlier diagnosis of the deficiencies [37].
In our work, the very high rate of TP due to multiple causes may result from the prospective systematic search for an etiology of TP. In numerous cases we identified multiple causes, of which sepsis was the most frequent, as previously reported [6, 16, 17]. An inverse relationship between the severity of sepsis and platelet count has been reported [38]. TP during sepsis may result from an increased consumption or destruction of platelets due to DIC, hemophagocytosis, and immune mechanisms. Additional support for an association between TP and infection derives from studies demonstrating that the platelets significantly influence the balance between infection and immunity [39]. We found a high prevalence of viral infections. However, it is uncertain whether these infections were responsible for the cases of TP.
The main consequence of TP is the perceived risk of bleeding, which may affect the management of thrombocytopenic patients by dissuading physicians from performing invasive procedures and administering anticoagulant therapy and subsequently lead to platelet transfusions. TP may contribute to bleeding in critically ill patients and ultimately result in death [3]. In our study, physicians administered platelet transfusion in patients with a platelet count below 50 × 109/L and who were developing active bleeding or undergoing an invasive procedure. This strategy is in agreement with recommendations published in 2012 by a French expert group [40]. Of note, of 35 patients with a platelet count below 20 × 109/L, 12 did not receive platelet transfusion or develop any severe bleeding events.
Five studies have assessed the risk for bleeding in ICU patients with TP [3, 5, 6, 14, 18], but only two used a consistent definition of bleeding. In univariate analysis most authors found a higher risk of bleeding in patients with lower platelet count [3, 6, 18] but in multivariate analysis the single variable associated with bleeding was sepsis [18]. In our study, the risk of bleeding was assessed after excluding patients who had received prophylactic platelet transfusions. A nadir platelet count below 50 × 109/L was identified as an independent risk factor for bleeding. We were unable to identify TP etiologies and patient subgroups as independent risk factors, but we cannot exclude the possibility that this negative result may have been due to the small number of patients and of SBEs. Furthermore, our study was limited to thrombocytopenic patients and did not include controls, and therefore, it is likely that the risk of severe bleeding events in the absolute TP group was underestimated.
We found that in ICU thrombocytopenic patients the presence of hemophagocytic syndrome carries a poor prognosis. However, we cannot preclude that we had over- or underestimated the diagnosis of hemophagocytic syndrome because we did not measure the absence of natural killer cell activity or the increase in soluble CD25 levels. In fact, hemophagocytic syndrome rather than a factor of excess mortality could be an additional marker of gravity. In a study of 56 patients with hemophagocytic syndrome including 13 with sepsis, the hospital mortality was 50 % and factors associated with hospital survival were Castleman’s disease and B cell lymphoma [35].
Conclusion
TP is associated with multiple etiologies in critically ill patients and, not surprisingly, sepsis is the leading cause. Bone marrow aspirates may yield significant information on TP mechanisms, and contribute to identifying etiologic diagnosis in some specific cases, especially in patients with absolute TP.
References
Vicente Rull JR, Loza Aguirre J, de la Puerta E, Moreno Millan E, Peñas Maldonado L, Perez Clausell C (1984) Thrombocytopenia induced by pulmonary artery flotation catheters. A prospective study. Intensive Care Med 10:29–31
Vonderheide RH, Thadhani R, Kuter DJ (1998) Association of thrombocytopenia with the use of intra-aortic balloon pumps. Am J Med 105:27–32
Vanderschueren S, De Weerdt A, Malbrain M, Vankersschaever D, Frans E, Wilmer A, Bobbaers H (2000) Thrombocytopenia and prognosis in intensive care. Crit Care Med 28:1871–1876
Akca S, Haji-Michael P, De Mendonça A, Suter P, Levi M, Vincent JL (2002) Time course of platelet counts in critically ill patients. Crit Care Med 30:753–756
Shalansky SJ, Verma AK, Levine M, Spinelli JJ, Dodek PM (2002) Risk markers for thrombocytopenia in critically ill patients: a prospective analysis. Pharmacotherapy 22:803–813
Strauss R, Wehler M, Mehler K, Kreutzer D, Koebnick C, Hahn EG (2002) Thrombocytopenia in patients in the medical intensive care unit: bleeding prevalence, transfusion requirements, and outcome. Crit Care Med 30:1765–1771
Crowther MA, Cook DJ, Meade MO, Griffith LE, Guyatt GH, Arnold DM, Rabbat CG, Geerts WH, Warkentin TE (2005) Thrombocytopenia in medical-surgical critically ill patients: prevalence, incidence, and risk factors. J Crit Care 20:348–353
Brogly N, Devos P, Boussekey N, Georges H, Chiche A, Leroy O (2007) Impact of thrombocytopenia on outcome of patients admitted to ICU for severe community-acquired pneumonia. J Infect 55:136–140
Sharma B, Sharma M, Majumder M, Steier W, Sangal A, Kalawar M (2007) Thrombocytopenia in septic shock patients—a prospective observational study of incidence, risk factors and correlation with clinical outcome. Anaesth Intensive Care 35:874–880
Caruso P, Ferreira AC, Laurienzo CE, Titton LN, Terabe DSM, Carnieli DS, Deheinzelin D (2010) Short- and long-term survival of patients with metastatic solid cancer admitted to the intensive care unit: prognostic factors. Eur J Cancer Care (Engl) 19:260–266
Vandijck DM, Blot SI, De Waele JJ, Hoste EA, Vandewoude KH, Decruyenaere JM (2010) Thrombocytopenia and outcome in critically ill patients with bloodstream infection. Heart Lung 39:21–26
Baughman RP, Lower EE, Flessa HC, Tollerud DJ (1993) Thrombocytopenia in the intensive care unit. Chest 104:1243–1247
Bonfiglio MF, Traeger SM, Kier KL, Martin BR, Hulisz DT, Verbeck SR (1995) Thrombocytopenia in intensive care patients: a comprehensive analysis of risk factors in 314 patients. Ann Pharmacother 29:835–842
Chakraverty R, Davidson S, Peggs K, Stross P, Garrard C, Littlewood TJ (1996) The incidence and cause of coagulopathies in an intensive care population. Br J Haematol 93:460–463
Hanes SD, Quarles DA, Boucher BA (1997) Incidence and risk factors of thrombocytopenia in critically ill trauma patients. Ann Pharmacother 31:285–289
Cawley MJ, Wittbrodt ET, Boyce EG, Skaar DJ (1999) Potential risk factors associated with thrombocytopenia in a surgical intensive care unit. Pharmacotherapy 19:108–113
Stéphan F, Hollande J, Richard O, Cheffi A, Maier-Redelsperger M, Flahault A (1999) Thrombocytopenia in a surgical ICU. Chest 115:1363–1370
Ben Hamida C, Lauzet J-Y, Rézaiguia-Delclaux S, Duvoux C, Cherqui D, Duvadelstin P, Stephan F (2003) Effect of severe thrombocytopenia on patient outcome after liver transplantation. Intensive Care Med 29:756–762
Salman SS, Fernández Pérez ER, Stubbs JR, Gajic O (2007) The practice of platelet transfusion in the intensive care unit. J Intensive Care Med 22:105–110
Cherif H, Martling C-R, Hansen J, Kalin M, Björkholm M (2007) Predictors of short and long-term outcome in patients with hematological disorders admitted to the intensive care unit for a life-threatening complication. Support Care Cancer 15:1393–1398
Hui P, Cook DJ, Lim W, Fraser GA, Arnold DM (2011) The frequency and clinical significance of thrombocytopenia complicating critical illness: a systematic review. Chest 139:271–278
Stephan F, Montblanc JD, Cheffi A, Bonnet F (1999) Thrombocytopenia in critically ill surgical patients: a case-control study evaluating attributable mortality and transfusion requirements. Crit Care 3:151–158
Martin CM, Priestap F, Fisher H et al (2009) A prospective, observational registry of patients with severe sepsis: the Canadian Sepsis Treatment and Response Registry. Crit Care Med 37:81–88
Moreau D, Timsit J-F, Vesin A, Garrouste-Orgeas M, de Lassence A, Zahar J-R, Adrie C, Vincent F, Cohen Y, Schlemmer B, Azoulay E (2007) Platelet count decline: an early prognostic marker in critically ill patients with prolonged ICU stays. Chest 131:1735–1741
Lo GK, Juhl D, Warkentin TE, Sigouin CS, Eichler P, Greinacher A (2006) Evaluation of pretest clinical score (4 T’s) for the diagnosis of heparin-induced thrombocytopenia in two clinical settings. J Thromb Haemost 4:759–765
Bernard GR, Vincent JL, Laterre PF, LaRosa SP, Dhainaut JF, Lopez-Rodriguez A, Steingrub JS, Garber GE, Helterbrand JD, Ely EW, Fisher CJ (2001) Efficacy and safety of recombinant human activated protein C for severe sepsis. N Engl J Med 344:699–709
Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, Cohen J, Opal SM, Vincent J-L, Ramsay G (2003) 2001 SCCM/ESICM/ACCP/ATS/SIS international sepsis definitions conference. Intensive Care Med 29:530–538
Taylor FB Jr, Toh CH, Hoots WK, Wada H, Levi M (2001) Towards definition, clinical and laboratory criteria, and a scoring system for disseminated intravascular coagulation. Thromb Haemost 86:1327–1330
Sivula M, Tallgren M, Pettilä V (2005) Modified score for disseminated intravascular coagulation in the critically ill. Intensive Care Med 31:1209–1214
George JN, Raskob GE, Shah SR, Rizvi MA, Hamilton SA, Osborne S, Vondracek T (1998) Drug-induced thrombocytopenia: a systematic review of published case reports. Ann Intern Med 129:886–890
Janka GE (2005) Hemophagocytic lymphohistiocytosis. Hematology 10(Suppl 1):104–107
Schols SEM, Heemskerk JWM, Van Pampus ECM (2010) Correction of coagulation in dilutional coagulopathy: use of kinetic and capacitive coagulation assays to improve hemostasis. Transfus Med Rev 24:44–52
Louwes H, Zeinali Lathori OA, Vellenga E, de Wolf JT (1999) Platelet kinetic studies in patients with idiopathic thrombocytopenic purpura. Am J Med 106:430–434
François B, Trimoreau F, Vignon P, Fixe P, Praloran V, Gastinne H (1997) Thrombocytopenia in the sepsis syndrome: role of hemophagocytosis and macrophage colony-stimulating factor. Am J Med 103:114–120
Buyse S, Teixeira L, Galicier L, Mariotte E, Lemiale V, Seguin A, Bertheau P, Canet E, de Labarthe A, Darmon M, Rybojad M, Schlemmer B, Azoulay E (2010) Critical care management of patients with hemophagocytic lymphohistiocytosis. Intensive Care Med 36:1695–1702
Wickramasinghe SN (2006) Diagnosis of megaloblastic anaemias. Blood Rev 20:299–318
Andrès E, Affenberger S, Zimmer J, Vinzio S, Grosu D, Pistol G, Maloisel F, Weitten T, Kaltenbach G, Blicklé J-F (2006) Current hematological findings in cobalamin deficiency. A study of 201 consecutive patients with documented cobalamin deficiency. Clin Lab Haematol 28:50–56
Mavrommatis AC, Theodoridis T, Orfanidou A, Roussos C, Christopoulou-Kokkinou V, Zakynthinos S (2000) Coagulation system and platelets are fully activated in uncomplicated sepsis. Crit Care Med 28:451–457
Yeaman MR (2010) Platelets in defense against bacterial pathogens. Cell Mol Life Sci 67:525–544
Van der Linden T, Souweine B, Dupic L, Soufir L, Meyer P (2012) Management of thrombocytopenia in the ICU (pregnancy excluded). Ann Intensive Care 2:42–47
Acknowledgments
The authors thank Delphine Moreau for her participation in the design and drafting of the protocol and Jeffrey Watts and Pistache Saint Gènes for their help in preparing the manuscript. We are also grateful for the participation of biologists from the other hospital centers. Financial support: French Health Ministry (PHRC).
Conflicts of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Thiolliere, F., Serre-Sapin, A.F., Reignier, J. et al. Epidemiology and outcome of thrombocytopenic patients in the intensive care unit: results of a prospective multicenter study. Intensive Care Med 39, 1460–1468 (2013). https://doi.org/10.1007/s00134-013-2963-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-013-2963-3