Abstract
Goal of work
The admission of patients with hematological disorders to the intensive care unit (ICU) involves a complex resource usage and may be associated with high mortality. The decision making to transfer a severely ill patient to the ICU, therefore, presents an ethical dilemma. We assessed both early and long-term outcomes in relation to clinical characteristics with the aim to facilitate clinical decision making.
Materials and methods
We performed a cohort study of hematological patients admitted to ICU at a university hospital.
Main results
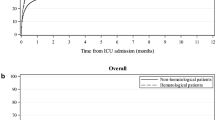
During a 6-year period (1996–2001), 85 patients with a median age of 59 years were admitted to ICU. The majority of patients (88%) suffered from hematological malignancies. Major reasons for ICU admission were respiratory failure (41%) and septic shock/pre-shock (24%). The median duration of ICU admission was 2 (1–67) days. Crude in-ICU, 30-day, and 6-month mortality rates were 30, 49, and 62%, respectively. Overall 5-year survival rate was 20%, and 13 (15%) patients were alive at time of follow-up (median 7.4 years). Respiratory failure requiring ventilatory support and a high Acute Physiology and Chronic Health Evaluation II score was significantly correlated to high in-ICU mortality, but not to long-term outcome. Type of hematological malignancy, neutropenia, thrombocytopenia, bacteremia, prior administration of chemotherapy, age, or gender was not significantly associated with outcome.
Conclusions
The current study provides encouraging results on long-term post-ICU outcome also in elderly patients with hematological diseases. For a substantial proportion of critically ill hematological patients, a short time care at an ICU is lifesaving. These patients should be offered intensive care unless or until it is clear that there is little prospect of recovery from the acute illness or that the underlying malignancy cannot be controlled.
Similar content being viewed by others
Introduction
Over the past decades, there has been a substantial progress in the management of patients with hematological malignancies including the development of risk-adapted treatment protocols, new chemotherapeutic agents, and other treatment modalities. This, together with improved supportive therapy, has extended survival time in these patients. Unfortunately, the intensification of cancer treatment has led to an increasing number of therapy-associated complications. These complications may be life threatening and often require advanced multidisciplinary care in an intensive care unit (ICU) [1]. The admission of patients with hematological disease to the ICU involves a complex resource usage. Furthermore, high mortality rates up to 75–85% have been reported in such patients especially when mechanical ventilation has been required [2–7]. The decision making to transfer a severely ill patient to the ICU, therefore, presents an ethical dilemma to hematologists as well as to intensive care specialists.
To maximize survival and limit unnecessary suffering and costs, attempts have been made to identify subgroups of patients that benefit from ICU admission [3, 5, 8–15]. Different potential risk factors have been analyzed including scoring systems to assess the severity of illness and organ failure. Such scoring systems have been shown to predict gross prognosis, but obviously, they cannot be used to distinguish survivors from non-survivors in the individual case [2, 11, 13, 15–17, 21]. In addition, there is limited information about long-term post-ICU survival in patients with hematological diseases.
In this study, focusing on patients with hematological diseases admitted to the ICU, we assessed both early and long-term outcomes in relation to clinical and laboratory characteristics with the aim to facilitate clinical decision making.
Materials and methods
We included all adult patients with hematological diseases admitted to the ICU at Karolinska University Hospital, Solna, over a 6-year period (1996–2001). The charts of these patients were reviewed, and detailed clinical and laboratory characteristics were recorded at the time of admission. The severity of acute illness was calculated for every patient at admission using the Acute Physiology and Chronic Health Evaluation (APACHE) II score [17]. Major reason for ICU admission, need for ventilation support, and time on ventilator were recorded. In-ICU, 30-day, 6-month mortality rates were determined. A data file with the unique personal identification numbers (obtained by each Swedish citizen shortly after birth or immigration) of these patients was linked with population-based Swedish Cause of Death Register run by the National Board of Health and Welfare, to get information on overall survival. Positive microbiological cultures taken within 1 week before or at admission were noted. For patients with multiple admissions, only the first admission was taken into account.
The major outcomes studied were short- (in-ICU and 30-day) and long-term (6-month and 5-year) mortality rates/survivals. The data are expressed as means (± standard deviation) or as medians (range). Risk factors for in-ICU, 30-day, and 6-month mortality were studied by univariate analysis using Student’s t test (when appropriate, the Mann–Whitney U-test was used) for continuous variables, chi-square test for categorical variables, and Fisher’s exact test for small expected frequencies. Significant differences observed in univariate analyses were evaluated by multivariate logistic regression analysis.
Results
During the study period, 85 adult patients with hematological diseases were admitted to the ICU for a life-threatening complication. Their median age was 59 years (18–82 years), and the majority of patients suffered from hematological malignancies with acute leukemia (24%), non-Hodgkin lymphoma (20%), and multiple myeloma (15%) dominating (Table 1). Major reasons for ICU admission were respiratory failure (41%) and septic shock/pre-shock (24%; Table 2). Forty-eight (56%) patients had received chemotherapy within 4 weeks before admission, and 31 (36%) were still neutropenic (absolute neutrophil count < 0.5 × 109/l) at admission with a median duration of neutropenia of 12 days (range 5–53 days). A total of 44 (51%) patients had a positive bacterial culture, and 21 (24%) had bacteremia (see “Materials and methods”; Table 3). Detailed characteristics of the 85 patients are shown in Table 1. The median follow-up period for surviving patients from admission to ICU was 7.4 years (range 4.9–10.5 years).
The overall in-ICU, 30-day, and 6-month mortality rates were 30, 49, and 62%, respectively. Overall 5-year survival rate was 20%, and 13 (15%) patients were alive at time of follow-up. Respiratory failure requiring ventilatory support and a high APACHE II score were significantly correlated to high in-ICU mortality. However, only respiratory failure requiring ventilatory support predicted a high 30-day mortality (Table 4). This was confirmed by the multivariable logistic regression analysis where only ventilatory support was independently associated with a poor short-term outcome (Table 5). Patients with nonmalignant hematological diseases had a better long-term outcome than those with hematological malignancies (Table 4). However, type of hematological malignancy (acute leukemia vs other malignancy), neutropenia, thrombocytopenia, bacteremia, prior administration of chemotherapy, age, or gender was not significantly associated with outcome (Table 4). The overall 6-month and 5-year survival rates among elderly patients (age > 65 years) and other patients (age < 65 years) were 33% vs 39% (P = 0.63) and 15% vs 13% (P = 0.56), respectively.
Among patients requiring ventilatory support (n = 33), the median duration of ventilator treatment was 3 days (1–15 days), being significantly longer in non-survivors than in survivors (mean, 3.4 ± 3.4 days vs 0.8 ± 2.4 days; P < 0.001). Thirty-day mortality rates in patients receiving mechanical ventilation and noninvasive ventilation were 82 and 50%, respectively (P = 0.08).
A liberal attitude towards ICU admission was adapted during the study period, indicating that all patient with potential life-threatening complications of hematological disease were offered intensive care unless or until it was clear that there was no prospect of recovery from the acute illness or that the underlying malignancy could not be controlled. The number of ICU admissions, major reasons for admissions, and mean of APACHE II scores remained stable during the study period. Thus, mean APACHE II scores and short- and long-term outcomes of patients admitted during the first 3-year period were not different from those of patients admitted during the last 3 years (P > 0.05). Eighty-six percent of the admissions were done during workdays. In-ICU mortality rates for patients admitted in holidays and in workdays were 41 and 30%, respectively (P = 0.49).
During the study period, a total of 193 patients were treated with high-dose chemotherapy followed by autologous hematopoietic stem cell transplantation (HSCT) in our unit. Only two (1%) of these patients needed intensive care. No allogeneic HSCT were performed in this unit.
Discussion
In this cohort study, comprising a population of patients with hematological diseases admitted to the ICU, we demonstrate a short- and long-term mortality which, albeit high, was comparable with that of critically ill non-cancer patients requiring intensive care [18–20]. Severe respiratory failure requiring mechanical ventilation was significantly associated with a worse outcome.
Several scoring systems to predict outcome in specific groups of ICU patients have been evaluated over the last two decades [13, 16, 17, 21]. In this study, the APACHE II scoring system predicted in-ICU mortality but not 30-day mortality or long-term survival. In previous reports, this scoring system has been shown to significantly discriminate survivors from non-survivors in critically ill patients, but has failed to predict individual outcome sufficiently [13, 15, 21]. The APACHE II scoring system alone should not be used for decision making about prolongation of resource-consuming treatment. Instead, it should serve to define patients at high risk who should be treated intensively and early.
The presence of a hematological malignancy or bacteremia was not significantly associated with outcome. These results are in accordance with some recent studies supporting the concept that these classic predictors of outcome have lost their impact on ICU mortality [9–11, 22]. The impact of age in critically ill patients with hematological malignancies is controversial. Some authors have reported worse outcome in the elderly patients [23]. However, in many studies, age is reported not to be an independent risk factor for death [5, 14, 24]. In our study, age above 65 years was not associated with a worse outcome, and elderly patients had a relatively high 6-month survival rate (33%). Therefore, there is no rationale for decision making regarding admission to the ICU based solely on patient’s age. Many authors have previously reported higher mortality rates in patients with profound neutropenia [1, 4, 25]. In the current study, and in good accordance with many other recent publications [3, 5, 6], neutropenia did not affect outcome. This finding can most probably be explained by the general improvement in the understanding and management of patients with chemotherapy-induced neutropenia.
The relatively low short- and long-term mortality rates (49 and 62%) in our study may be related to several factors. Firstly, an improvement in ICU survival rates has also been reported by other authors reflecting most probably a more liberal attitude regarding the indications for ICU admission together with improved ICU facilities through the last two decades [22, 24, 26, 27]. Secondly, we did not include patients undergoing allogeneic HSCT, as these patients were treated at a separate unit. Thirdly, despite the fact that this study was performed at a single institution, there is of course a selection bias regarding do-not-resuscitate orders in elderly and terminally ill patients. However, the homogeneity of the patient population throughout the study period probably reflects a consistency in treatment decisions.
During the study period, only 1% of patient who underwent autologous HSCT developed life-threatening complications requiring admission to the ICU. This number is lower than that reported in many earlier studies [28, 29]. However, more recent studies have demonstrated a decreasing ICU utilization in this patient category [30]. Improvements in the management of therapy-related complications and a refinement in patient selection can probably explain this encouraging finding.
The development of acute respiratory failure remains one of the foremost reasons for ICU admission of cancer patients [9, 14, 22, 31]. In the current study, the need for mechanical ventilation had a profound and sustained adverse effect on outcome. However, 25% (8/33) of patients requiring ventilatory support were still alive at 6 months, and 3 of these patients were long-term survivors (>5 years). Some authors have advocated limited intensive care use in patients after HCST and in patients in need of mechanical ventilation based on reports of a high mortality. However, recent reports have shown improved ICU survival even in these high-risk categories [32], reflecting an ongoing improvement in hematology and intensive care. Moreover, compared with other ICU patient categories, the duration of ICU admissions in patients with hematological diseases seems to be short (median of 2 days). This probably indicates an effective utilization of ICU resources.
In conclusion, the current study provides encouraging results on long-term post-ICU outcome in patients with hematological diseases. For a substantial proportion of critically ill hematological patients, a short time care at an ICU is lifesaving. Hematological patients with life-threatening complications should be offered intensive care unless or until it is clear that there is little prospect of recovery from the acute illness or that the underlying malignancy cannot be controlled.
References
Lloyd-Thomas AR, Dhaliwal HS, Lister TA, Hinds CJ (1986) Intensive therapy for life-threatening medical complications of haematological malignancy. Intensive Care Med 12:317–324
Cornet AD, Issa AI, van de Loosdrecht AA, Ossenkoppele GJ, Strack van Schijndel RJ, Groeneveld AB (2005) Sequential organ failure predicts mortality of patients with a haematological malignancy needing intensive care. Eur J Haematol 74:511–516
Epner DE, White P, Krasnoff M, Khanduja S, Kimball KT, Knaus WA (1996) Outcome of mechanical ventilation for adults with hematologic malignancy. J Investig Med 44:254–260
Estopa R, Torres Marti A, Kastanos N, Rives A, Agusti-Vidal A, Rozman C (1984) Acute respiratory failure in severe hematologic disorders. Crit Care Med 12:26–28
Groeger JS, Lemeshow S, Price K, Nierman DM, White P Jr, Klar J, Granovsky S, Horak D, Kish SK (1998) Multicenter outcome study of cancer patients admitted to the intensive care unit: a probability of mortality model. J Clin Oncol 16:761–770
Peters SG, Meadows JA III, Gracey DR (1988) Outcome of respiratory failure in hematologic malignancy. Chest 94:99–102
Tremblay LN, Hyland RH, Schouten BD, Hanly PJ (1995) Survival of acute myelogenous leukemia patients requiring intubation/ventilatory support. Clin Invest Med 18:19–24
Azoulay E, Adrie C, De Lassence A, Pochard F, Moreau D, Thiery G, Cheval C, Moine P, Garrouste-Orgeas M, Alberti C, Cohen Y, Timsit JF (2003) Determinants of postintensive care unit mortality: a prospective multicenter study. Crit Care Med 31:428–432
Azoulay E, Moreau D, Alberti C, Leleu G, Adrie C, Barboteu M, Cottu P, Levy V, Le Gall JR, Schlemmer B (2000) Predictors of short-term mortality in critically ill patients with solid malignancies. Intensive Care Med 26:1817–1823
Benoit DD, Vandewoude KH, Decruyenaere JM, Hoste EA, Colardyn FA (2003) Outcome and early prognostic indicators in patients with a hematologic malignancy admitted to the intensive care unit for a life-threatening complication. Crit Care Med 31:104–112
Blot F, Guiguet M, Nitenberg G, Leclercq B, Gachot B, Escudier B (1997) Prognostic factors for neutropenic patients in an intensive care unit: respective roles of underlying malignancies and acute organ failures. Eur J Cancer 33:1031–1037
Evison J, Rickenbacher P, Ritz R, Gratwohl A, Haberthur C, Elsasser S, Passweg JR (2001) Intensive care unit admission in patients with haematological disease: incidence, outcome and prognostic factors. Swiss Med Wkly 131:681–686
Guiguet M, Blot F, Escudier B, Antoun S, Leclercq B, Nitenberg G (1998) Severity-of-illness scores for neutropenic cancer patients in an intensive care unit: which is the best predictor? do multiple assessment times improve the predictive value? Crit Care Med 26:488–493
Massion PB, Dive AM, Doyen C, Bulpa P, Jamart J, Bosly A, Installe E (2002) Prognosis of hematologic malignancies does not predict intensive care unit mortality. Crit Care Med 30:2260–2270
Price KJ, Thall PF, Kish SK, Shannon VR, Andersson BS (1998) Prognostic indicators for blood and marrow transplant patients admitted to an intensive care unit. Am J Respir Crit Care Med 158:876–884
Silfvast T, Pettila V, Ihalainen A, Elonen E (2003) Multiple organ failure and outcome of critically ill patients with haematological malignancy. Acta Anaesthesiol Scand 47:301–306
Knaus WA, Draper EA, Wagner DP, Zimmerman JE (1985) APACHE II: a severity of disease classification system. Crit Care Med 13:818–829
Gopal I, Bhonagiri S, Ronco C, Bellomo R (1997) Out of hospital outcome and quality of life in survivors of combined acute multiple organ and renal failure treated with continuous venovenous hemofiltration/hemodiafiltration. Intensive Care Med 23:766–772
Korosec Jagodic H, Jagodic K, Podbregar M (2006) Long-term outcome and quality of life of patients treated in surgical intensive care: a comparison between sepsis and trauma. Crit Care 10:R134
Reyes WJ, Brimioulle S, Vincent JL (1999) Septic shock without documented infection: an uncommon entity with a high mortality. Intensive Care Med 25:1267–1270
Le Gall JR, Lemeshow S, Saulnier F (1993) A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA 270:2957–2963
Staudinger T, Stoiser B, Mullner M, Locker GJ, Laczika K, Knapp S, Burgmann H, Wilfing A, Kofler J, Thalhammer F, Frass M (2000) Outcome and prognostic factors in critically ill cancer patients admitted to the intensive care unit. Crit Care Med 28:1322–1328
Darmon M, Azoulay E, Alberti C, Fieux F, Moreau D, Le Gall JR, Schlemmer B (2002) Impact of neutropenia duration on short-term mortality in neutropenic critically ill cancer patients. Intensive Care Med 28:1775–1780
Azoulay E, Alberti C, Bornstain C, Leleu G, Moreau D, Recher C, Chevret S, Le Gall JR, Brochard L, Schlemmer B (2001) Improved survival in cancer patients requiring mechanical ventilatory support: impact of noninvasive mechanical ventilatory support. Crit Care Med 29:519–525
Lloyd-Thomas AR, Wright I, Lister TA, Hinds CJ (1988) Prognosis of patients receiving intensive care for life-threatening medical complications of haematological malignancy. Br Med J (Clin Res Ed) 296:1025–1029
Azoulay E, Recher C, Alberti C, Soufir L, Leleu G, Le Gall JR, Fermand JP, Schlemmer B (1999) Changing use of intensive care for hematological patients: the example of multiple myeloma. Intensive Care Med 25:1395–1401
Kress JP, Christenson J, Pohlman AS, Linkin DR, Hall JB (1999) Outcomes of critically ill cancer patients in a university hospital setting. Am J Respir Crit Care Med 160:1957–1961
Torrecilla C, Cortes JL, Chamorro C, Rubio JJ, Galdos P, Dominguez de Villota E (1988) Prognostic assessment of the acute complications of bone marrow transplantation requiring intensive therapy. Intensive Care Med 14:393–398
Crawford SW, Schwartz DA, Petersen FB, Clark JG (1988) Mechanical ventilation after marrow transplantation. Risk factors and clinical outcome. Am Rev Respir Dis 137:682–687
Soubani AO., Kseibi E, Bander JJ, Klein JL, Khanchandani G, Ahmed HP, Guzman JA (2004) Outcome and prognostic factors of hematopoietic stem cell transplantation recipients admitted to a medical ICU. Chest 126:1604–1611
Soares M, Salluh JI, Spector N, Rocco JR (2005) Characteristics and outcomes of cancer patients requiring mechanical ventilatory support for >24 hrs. Crit Care Med 33:520–526
Moran JL, Solomon PJ, Williams PJ (2005) Assessment of outcome over a 10-year period of patients admitted to a multidisciplinary adult intensive care unit with haematological and solid tumours. Anaesth Intensive Care 33:26–35
Acknowledgements
We thank Bo Nilsson, BSc, Unit of Cancer Epidemiology, Karolinska Institutet, Karolinska University Hospital, Stockholm, Sweden, for statistical advice. This study was supported by grants from the Swedish Cancer Society, the Stockholm County Council, and Karolinska Institutet Foundations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cherif, H., Martling, CR., Hansen, J. et al. Predictors of short and long-term outcome in patients with hematological disorders admitted to the intensive care unit for a life-threatening complication. Support Care Cancer 15, 1393–1398 (2007). https://doi.org/10.1007/s00520-007-0268-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-007-0268-1