Abstract
Background
Thrombocytosis is a common phenomenon in critically ill patients. Although thrombocytosis is an independent risk factor for complications, it does not seem to influence mortality in intensive care (ICU) patients.
Objectives
Our investigation aimed to evaluate the etiological and clinical relevance of a platelet count greater than 450 × 109/l in ICU patients.
Materials and methods
Patients admitted for a minimum of 4 days to an interdisciplinary ICU during a 45-month period were enrolled in this retrospective observational study. Thrombocytopenic patients (platelet count <150 × 109/l in at least one measurement) were excluded. The study patients were divided into two groups: thrombocytosis group (thrombocytes >450 × 109/l in at least one measurement) and control group (thrombocytes = 150 − 450 × 109/l during ICU stay). Univariate and multiple regression analysis were used to determine the influence of severe co-morbidities on the development of thrombocytosis and the association of elevated platelet count with thrombotic embolism, length of stay (LOS) in ICU, and mortality.
Results
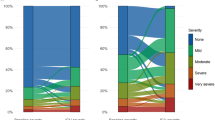
A total of 307 patients were analyzed, of whom thrombocytosis was observed in 119 cases. Independent risk factors for the development of thrombocytosis included SIRS, mechanical ventilation, and acute bleeding. Increasing age reduced the risk of thrombocytosis. Thromboembolism occurred in 16 patients (13.4%) with an elevated platelet count and only in nine patients (4.7%) with physiological platelet values (OR: 3.1; 95% CI: 1.3–7.2; p = 0.009). Mean duration of LOS was significantly longer in patients with thrombocytosis (25.2 vs.11.7 days, p < 0.0001). Elevated platelet count showed a negative correlation with ICU mortality (OR: 0.32; 95%-CI: 0.12–0.83; p = 0.019).
Conclusion
In our retrospective analysis the occurrence of thrombocytosis in a cohort of interdisciplinary ICU patients was associated with a higher rate of complications and longer LOS in the ICU. Despite these findings, thrombocytosis seems to reduce mortality in critical ill patients.
Zusammenfassung
Hintergrund
Eine erhöhte Thrombozytenzahl tritt häufig bei kritisch kranken Patienten auf. Obwohl diese als ein Risikofaktor für schwere Komplikationen betrachtet wird, scheint sie die Prognose der Intensivpatienten nicht zu verschlechtern.
Fragestellung
Ziel dieser Studie war es, die Ätiologie und klinische Relevanz einer Thrombozytenzahl über 450 × 109/l in einem intensivmedizinischen Patientenkollektiv zu untersuchen.
Material und Methoden
In diese retrospektive Beobachtungsstudie wurden für einen 45-monatigen Zeitraum alle Intensivpatienten mit einer Verweildauer von mindestens 4 Tagen eingeschlossen. Die Patienten mit einer Thrombozytenzahl unter 150 × 109/l wurden aus der weiteren Analyse ausgeschlossen. Die evaluierten Patienten wurden in 2 Gruppen geteilt: Thrombozytosegruppe (Thrombozyten >450 × 109/l in mindestens einer Untersuchung) und Kontrollgruppe (Thrombozyten: 150 × 109/l bis 450 × 109/l). Mit univarianten und multiplen Regressionsanalysen wurden Komorbiditäten auf das Auftreten einer Thrombozytose hin untersucht. Darüber hinaus wurde die Assoziation einer erhöhten Thrombozytenzahl in Bezug auf eine Thromboembolie, die intensivmedizinische Verweildauer und Mortalität evaluiert.
Ergebnisse
Ausgewertet wurden die Daten von 307 Patienten: 119 in der Thrombozytosegruppe und 188 in der Kontrollgruppe. Die unabhängige Risikofaktoren einer Thrombozytose waren: SIRS („systemic inflammatory response syndrome“), Beatmungstherapie, akute Hämorrhagie und geringeres Alter. Eine venöse Thromboembolie trat bei 13,4 % der Patienten mit Thrombozytose und bei 4,7 % der Kontrollgruppe auf (Odds Ratio, OR: 3,1; 95 %-Konfidenzintervall, 95 %-KI: 1,3-7,2; p = 0,009). Die durchschnittliche Verweildauer auf der Intensivstation war in der Thrombozytosegruppe signifikant länger als in der Kontrollgruppe (25,2 ± 17,7 vs. 11,7 ± 10,4 Tage; p < 0,0001). Die Mortalität lag bei 11,7 % in der Thrombozytosegruppe, verglichen mit 14,9 % in der Kontrollgruppe, wobei die Patienten mit Thrombozytose einen wesentlich höheren initialen Schwergrad der Erkrankung aufwiesen (Simplified Acute Physiology Score II, SAPS II: 55 vs. 49 Punkte; p < 0,001). In der multifaktoriellen Regressionsanalyse war die Thrombozytose signifikant mit einer Risikosenkung der intensivstationären Mortalität assoziiert (OR: 0,32; 95%-KI: 0,12–0,83; p = 0,019).
Schlussfolgerung
Thrombozytose bei intensivmedizinischen Patienten ist mit einem Auftreten schwerer Komorbiditäten und einem erhöhten Risiko venöser Thromboembolien assoziiert, woraus sich eine verlängerte intensivmedizinische Verweildauer ableiten lässt. Hingegen reduziert eine Thrombozytose bei intensivmedizinischen Patienten das Mortalitätsrisiko und kann somit als Zusatzparameter in der Abschätzung des Verlaufs dienen.



Similar content being viewed by others
References
Agrawal S, Sachdev A, Gupta D et al (2008) Platelet counts and outcome in the pediatric intensive care unit. Indian J Crit Care Med 12:102–108
Akca S, Haji-Michael P, De Mendonca A et al (2002) Time course of platelet counts in critically ill patients. Crit Care Med 30:753–756
Akinosoglou K, Alexopoulos D (2014) Use of antiplatelet agents in sepsis: a glimpse into the future. Thromb Res 133:131–138
American Thoracic Society, Infectious Diseases Society Of A (2005) Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med 171:388–416
Bone RC, Balk RA, Cerra FB et al (1992) Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest 101:1644–1655
Brun-Buisson C (2000) The epidemiology of the systemic inflammatory response. Intensive Care Med 26(Suppl 1):S64–S74
Buss DH, Cashell AW, O’connor ML et al (1994) Occurrence, etiology, and clinical significance of extreme thrombocytosis: a study of 280 cases. Am J Med 96:247–253
De Backer D, Orbegozo Cortes D, Donadello K et al (2014) Pathophysiology of microcirculatory dysfunction and the pathogenesis of septic shock. Virulence 5:73–79
Folman CC, Ooms M, Kuenen BB et al (2001) The role of thrombopoietin in post-operative thrombocytosis. Br J Haematol 114:126–133
Gofrit ON, Shapiro A, Rund D et al (2006) Postoperative thrombocytosis as a marker for complications after urologic surgery. Scand J Urol Nephrol 40:161–165
Griesshammer M, Bangerter M, Sauer T et al (1999) Aetiology and clinical significance of thrombocytosis: analysis of 732 patients with an elevated platelet count. J Intern Med 245:295–300
Gurung AM, Carr B, Smith I (2001) Thrombocytosis in intensive care. Br J Anaesth 87:926–928
Ho KM, Chavan S (2013) Prevalence of thrombocytosis in critically ill patients and its association with symptomatic acute pulmonary embolism. A multicentre registry study. Thromb Haemost 109:272–279
Ho KM, Yip CB, Duff O (2012) Reactive thrombocytosis and risk of subsequent venous thromboembolism: a cohort study. J Thromb Haemost 10:1768–1774
Kaser A, Brandacher G, Steurer W et al (2001) Interleukin-6 stimulates thrombopoiesis through thrombopoietin: role in inflammatory thrombocytosis. Blood 98:2720–2725
Kashuk JL, Moore EE, Johnson JL et al (2010) Progressive postinjury thrombocytosis is associated with thromboembolic complications. Surgery 148:667–674 (discussion 674–665)
Kaushansky K (2005) The molecular mechanisms that control thrombopoiesis. J Clin Invest 115:3339–3347
Le Gall JR, Lemeshow S, Saulnier F (1993) A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA 270:2957–2963
Moher D, Hopewell S, Schulz KF et al (2010) CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. J Clin Epidemiol 63:e1–e37
Muehlstedt SG, Richardson CJ, Lyte M et al (2002) Systemic and pulmonary effector cell function after injury. Crit Care Med 30:1322–1326
Nijsten MW, Ten Duis HJ, Zijlstra JG et al (2000) Blunted rise in platelet count in critically ill patients is associated with worse outcome. Crit Care Med 28:3843–3846
Pate A, Baltazar GA, Labana S et al (2015) Systemic inflammatory response syndrome and platelet count 〉/=250x10(9) are associated with venous thromboembolic disease. Int J Gen Med 8:37–40
Powner DJ, Hoots WK (2008) Thrombocytosis in the NICU. Neurocrit Care 8:471–475
Reid VL, Webster NR (2012) Role of microparticles in sepsis. Br J Anaesth 109:503–513
Russwurm S, Vickers J, Meier-Hellmann A et al (2002) Platelet and leukocyte activation correlate with the severity of septic organ dysfunction. Shock 17:263–268
Salim A, Hadjizacharia P, Dubose J et al (2009) What is the significance of thrombocytosis in patients with trauma? J Trauma 66:1349–1354
Schafer AI (2004) Thrombocytosis. N Engl J Med 350:1211–1219
Schmuziger M, Christenson JT, Maurice J et al (1995) Reactive thrombocytosis after coronary bypass surgery. An important risk factor. Eur J Cardiothorac Surg 9:393–397 (discussion 397–398)
Stamou KM, Toutouzas KG, Kekis PB et al (2006) Prospective study of the incidence and risk factors of postsplenectomy thrombosis of the portal, mesenteric, and splenic veins. Arch Surg 141:663–669
Strauss R, Wehler M, Mehler K et al (2002) Thrombocytopenia in patients in the medical intensive care unit: bleeding prevalence, transfusion requirements, and outcome. Crit Care Med 30:1765–1771
Tchebiner JZ, Nutman A, Boursi B et al (2011) Diagnostic and prognostic value of thrombocytosis in admitted medical patients. Am J Med Sci 342:395–401
Tefferi A, Thiele J, Orazi A et al (2007) Proposals and rationale for revision of the World Health Organization diagnostic criteria for polycythemia vera, essential thrombocythemia, and primary myelofibrosis: recommendations from an ad hoc international expert panel. Blood 110:1092–1097
Valade N, Decailliot F, Rebufat Y et al (2005) Thrombocytosis after trauma: incidence, aetiology, and clinical significance. Br J Anaesth 94:18–23
Van Wessem KJ, Hennus MP, Heeres M et al (2013) Mechanical ventilation is the determining factor in inducing an inflammatory response in a hemorrhagic shock model. J Surg Res 180:125–132
Van Wessem KJ, Hennus MP, Van Wagenberg L et al (2013) Mechanical ventilation increases the inflammatory response induced by lung contusion. J Surg Res 183:377–384
Vanderschueren S, De Weerdt A, Malbrain M et al (2000) Thrombocytopenia and prognosis in intensive care. Crit Care Med 28:1871–1876
Wolber EM, Fandrey J, Frackowski U et al (2001) Hepatic thrombopoietin mRNA is increased in acute inflammation. Thromb Haemost 86:1421–1424
Zarbock A, Polanowska-Grabowska RK, Ley K (2007) Platelet-neutrophil-interactions: linking hemostasis and inflammation. Blood Rev 21:99–111
Acknowledgements
The authors thank Carmen Hennig and Annett Christel for the help in preparing the patients’ database.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
M. Banach, C. Lautenschläger, P. Kellner, and J. Soukup declare that they have no competing interests.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Additional information
Editorial board
M. Buerke, Siegen
P. Kellner and J. Soukup contributed equally to this study.
Rights and permissions
About this article
Cite this article
Banach, M., Lautenschläger, C., Kellner, P. et al. Etiology and clinical relevance of elevated platelet count in ICU patients. Med Klin Intensivmed Notfmed 113, 101–107 (2018). https://doi.org/10.1007/s00063-017-0276-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00063-017-0276-y