Abstract
This chapter focuses on the impact of fluid administration and ventilation on hemodynamics in critically ill patients. The chapter emphasizes the importance of determining fluid responsiveness before administering fluids to avoid volume overload, which can lead to increased morbidity and mortality. The parameters for predicting fluid responsiveness are based on cyclic variations in respiration on cardiac filling and require an understanding of heart-lung interactions. The chapter discusses the basics of respiratory and cardio-circulatory physiology, including the two components of the cardiovascular system (the circuit and pump), and how they are affected by transmural pressure. It will discuss the different functional hemodynamic monitoring tools with their indications and pitfalls. A thorough understanding of the effects of spontaneous and positive pressure ventilation on the cardiovascular system is important for anticipating and predicting hemodynamic effects after fluid administration and developing strategies to avoid or treat fluid infusion-related complications.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
- Shock
- Passive leg raising
- Pulse pressure variation
- Stroke volume variation
- Functional hemodynamics
- Fluid responsiveness
- Cardiac preload
- Heart-lung interactions
This chapter will explore a variety of different methods for determining fluid responsiveness, many of which are based on heart-lung interactions. A recent review paper provides a comprehensive overview of the various monitoring tools available, including arterial waveform variations and the passive leg raising test, as well as several other approaches [1]. It is noteworthy that any test, in order to be able to predict fluid responsiveness, should monitor cardiac output (CO) continuously.
Arterial waveform analysis. The first method to be discussed involves taking advantage of heart-lung interactions, specifically the respiratory variations in arterial pressure that are seen in ventilated patients. These variations have been shown to be related to central blood volume, diastolic function, and cardiac contractility. In 2000, Michard and colleagues demonstrated that the respiratory variation in pulse pressure, or pulse pressure variation (PPV), which reflects stroke volume variation (SVV), can detect fluid responsiveness when it is increased above 12–15% during controlled mechanical ventilation [2].
Since then, numerous studies have confirmed the validity of this index, while others have described various surrogates for stroke volume whose respiratory variability predicts response to fluid, such as systolic pressure variation (SPV) with the separation of deltaUp and deltaDown phenomena [3]. Only the deltaDown is an indicator for fluid responsiveness whereas deltaUp can be increased in patients with heart failure and situations of increased intrathoracic pressure (e.g., with high PEEP, autoPEEP, or abdominal hypertension). However, the limitations of these functional hemodynamic parameters soon became apparent, as to be accurate, PPV and SVV require a fixed heart rate and a significant positive-pressure-induced increase in intrathoracic pressure.
Other factors, such as spontaneous respiratory activity, cardiac arrhythmias, lower tidal volumes used in the management of acute respiratory distress syndrome, as well as low pulmonary compliance, increased intra-abdominal pressure [4], and right heart failure, may generate false positives and false negatives [5], making neither PPV nor SVV usable across all patients with cardiovascular insufficiency.
Although a little bit counterintuitive, PPV has a better overall area under the receiver operating characteristic curve (AUROC) to predict fluid responsiveness compared to SVV, and thus is preferred. In 2004, two articles in the same issue of the journal reported the ability of changes in the inferior vena cava diameter to predict fluid responsiveness [6, 7]. Unfortunately, vena cava distensibility shares many limitations with PPV and SVV and has limited predictive value [8].
The passive leg raising test. To circumvent the limits of PPV, the passive leg raising (PLR) test has been developed. The postural change, which was used for years by rescuers in patients falling in collapse, induces a significant though transient blood transfer from the lower extremities and the splanchnic territory that increases cardiac preload. The PLR test is considered positive if the cardiac output (CO) increases with 10%.
In 2006, the ability of the PLR test to detect preload responsiveness was demonstrated, including in conditions in which PPV is invalid [9]. It has been widely validated and integrated into international recommendations [10].
The end expiratory occlusion test. In 2009, heart-lung interactions during mechanical ventilation were explored again, and the end-expiratory occlusion test was developed, consisting of temporarily stopping the cyclical drop in preload caused by insufflation. This test was shown to indicate preload responsiveness if CO increased with 5% [11].
The respiratory systolic variation test. The respiratory systolic variation test (RSVT) was developed in 2005, consisting of four incremental, successive, pressure-controlled breaths [12], and the slope of the RSVT decreased significantly after intravascular fluid administration and correlated with the end-diastolic area and with changes in cardiac output better than filling pressure. Later, in 2017, the tidal volume challenge was developed to use PPV despite low tidal volume ventilation [13]. It simply consists of transiently increasing the tidal volume from 6 to 8 mL/kg and detecting a PPV increase in preload-responsive patients. The haemodynamic effects of recruitment manoeuvres also use heart-lung interactions (Fig. 5.1).
Tests and indices of preload responsiveness with proposed timeline. The principle of the dynamic assessment of preload responsiveness is to observe spontaneous or induced changes in cardiac preload, and the resulting change in cardiac output, stroke volume or their surrogates. Some tests or indices use heart–lung interactions in mechanically ventilated patients, while some others mimic a classical fluid challenge. Diagnostic threshold and the year of description are indicated. CO cardiac output, PPV pulse pressure variation. Adapted with permission from Monnet et al. [1]
The mini-fluid challenge test. Finally, since the “classical” fluid challenge (4 ml/kg/5–15 min) inherently induces fluid overload (when continued until the patient becomes no longer fluid responsive), a “mini-fluid challenge” made up of only 100–150 mL (1–2 ml/kg/1–5 min) of fluid was demonstrated to also predict volume responsiveness but with less inherent fluid accumulation (14). It has already received a reasonable validation.
Suggested Reading
-
1.
Monnet X, Malbrain M, Pinsky MR. The prediction of fluid responsiveness. Ann Intensive Care. 2022;12:46.
-
2.
Michard F, Boussat S, Chemla D, Anguel N, Mercat A, Lecarpentier Y, et al. Relation between respiratory changes in arterial pulse pressure and fluid responsiveness in septic patients with acute circulatory failure. Am J Respir Crit Care Med. 2000;162(1):134–8.
-
3.
Perel A, Pizov R, Cotev S. Systolic blood pressure variation is a sensitive indicator of hypovolemia in ventilated dogs subjected to graded hemorrhage. Anesthesiology. 1987;67(4):498–502.
-
4.
Malbrain MLNG, De Keulenaer BL, Khanna AK. Continuous intra-abdominal pressure: is it ready for prime time? Intensive Care Med. 2022;48(10):1501–4.
-
5.
Monnet X, Shi R, Teboul JL. Prediction of fluid responsiveness. What’s new? Ann Intensive Care. 2022;12(1):46.
-
6.
Barbier C, Loubieres Y, Schmit C, Hayon J, Ricome JL, Jardin F, et al. Respiratory changes in inferior vena cava diameter are helpful in predicting fluid responsiveness in ventilated septic patients. Intensive Care Med. 2004;30(9):1740–6.
-
7.
Feissel M, Michard F, Faller JP, Teboul JL. The respiratory variation in inferior vena cava diameter as a guide to fluid therapy. Intensive Care Med. 2004;30(9):1834–7.
-
8.
Vignon P, Repesse X, Begot E, Leger J, Jacob C, Bouferrache K, et al. Comparison of Echocardiographic Indices Used to Predict Fluid Responsiveness in Ventilated Patients. Am J Respir Crit Care Med. 2017;195(8):1022–32.
-
9.
Monnet X, Rienzo M, Osman D, Anguel N, Richard C, Pinsky MR, et al. Passive leg raising predicts fluid responsiveness in the critically ill. Crit Care Med. 2006;34(5):1402–7.
-
10.
Evans L, Rhodes A, Alhazzani W, Antonelli M, Coopersmith CM, French C, et al. Executive Summary: Surviving sepsis campaign: international guidelines for the management of sepsis and septic shock 2021. Crit Care Med. 2021;49(11):1974–82.
-
11.
Gavelli F, Shi R, Teboul JL, Azzolina D, Monnet X. The end-expiratory occlusion test for detecting preload responsiveness: a systematic review and meta-analysis. Ann Intensive Care. 2020;10(1):65.
-
12.
Perel A, Minkovich L, Preisman S, Abiad M, Segal E, Coriat P. Assessing fluid-responsiveness by a standardized ventilatory maneuver: the respiratory systolic variation test. Anesth Analg. 2005;100(4):942–5.
-
13.
Myatra SN, Prabu NR, Divatia JV, Monnet X, Kulkarni AP, Teboul JL. The changes in pulse pressure variation or stroke volume variation after a “tidal volume challenge” reliably predict fluid responsiveness during low tidal volume ventilation. Crit Care Med. 2017;45(3):415–21.
-
14.
Muller L, Toumi M, Bousquet PJ, Riu-Poulenc B, Louart G, Candela D, et al. An increase in aortic blood flow after an infusion of 100 ml colloid over 1 minute can predict fluid responsiveness: the mini-fluid challenge study. Anesthesiology. 2011;115(3):541–7.
The learning objectives of this chapter are:
-
1.
Physiology of heart-lung interactions and their effect on hemodynamics
-
2.
Identify fluid responsiveness using heart-lung interactions
-
3.
Physiology, techniques, and evidence of various dynamic measures of fluid responsiveness based on heart-lung interactions
-
4.
Clinical implication of fluid responsiveness and consideration for fluid accumulation with injudicious fluid administration
Mr. J, a 62-year-old male with a history of hypertension, presented to the ICU with septic shock secondary to a urinary tract infection. The patient was intubated and mechanically ventilated, and initial resuscitation with fluids and vasopressors was initiated. The patient remained hypotensive despite ongoing vasopressor support. The critical care team suspected that the patient might be volume depleted, and they wanted to assess his fluid responsiveness.
The team decided to use heart-lung interactions to assess fluid responsiveness in Mr. J. They performed a passive leg raise (PLR) maneuver and monitored the patient’s hemodynamic response.
During the PLR, the team observed an increase in the stroke volume (SV) by 20%, indicating that Mr. J was fluid responsive. The patient received a fluid bolus, and his blood pressure improved. The team continued to monitor the patient closely and adjusted his fluid management accordingly.
Questions
-
Q1. Why did the critical care team decide to use heart-lung interactions to assess fluid responsiveness in Mr. J?
-
Q2. What was the hemodynamic response observed during the PLR maneuver, and what does it indicate and what are its limitations?
Introduction
A thorough understanding of ventilation and its effects on the hemodynamics of critically ill patients constitutes an integral part of managing patients in intensive care units. Cardiopulmonary interactions in ventilated and non-ventilated patients may affect the hemodynamics, which can lead to diminished tissue oxygen delivery and organ dysfunctions, thereby contributing to morbidity and mortality. Therefore, a thorough understanding of the effects of spontaneous and positive pressure ventilation on the cardiovascular system helps us to understand hemodynamic perturbations better and manage them appropriately.
The main goal of fluid administration is to increase the preload and ultimately to improve cardiac output and oxygen delivery. While consensus exists on the use of fluid challenge to assess preload responsiveness, the type of fluid, extent and rate of administration, and hemodynamic targets need to be standardized in clinical practice [1]. At times, the fluid challenge is unsafe and leads to volume overload in non-responders [2].
Increasing evidence suggests that excessive fluid administration is associated with increased mortality [3]. Fluid need and responsiveness should be assessed before fluid administration to avoid volume overload and its complications.
Differentiating fluid responders from non-responders is essential to determine the efficacy of therapy and to avoid the deleterious effects of volume overload. For this reason, various static and dynamic parameters have been used in critically ill patients to predict volume responsiveness. These parameters have varying degrees of accuracy and shortcomings in various patient groups. All these parameters are based on the impact of the cyclic variations caused by respiration on the cardiac filling and hence require a thorough understanding of heart-lung interactions. See also Chap. 4 to learn more about fluid dynamics during resuscitation according to Frank–Starling and Guyton-Hall.
Basics of Respiratory and Cardio-Circulatory Physiology
The cardiovascular system consists of mainly two components: the circuit and the pump. The circuit contains arterial resistance and venous capacitance vessels. Arteries and arterioles are the resistance vessels that have smooth muscles responsible for controlling the resistance to blood flow by changing the caliber. Venules and veins are capacitance vessels that hold at least 70% of circulating blood volume and have no major contribution to resistance. The pump is constituted of the right and left ventricles, enclosed by the pericardium. The ventricles work in parallel but pump in series and are connected to each other through pulmonary circulation. Both the heart and surrounding lungs are enclosed within the rigid chest wall, creating a chamber within a chamber effect [4]. Therefore, phasic changes in pleural pressure during the respiratory cycle will affect the pressure system of the cardiac chambers and influence the gradient for venous return, preload, and afterload [5, 6].
Transmural pressure (PTM) is the difference of pressures (internal to external) across a hollow structure. In the thoracic cavity, the external pressure for the heart is pericardial pressure (PPER) and for lungs, the external pressure is the pleural pressure (PPL) [7, 8].
The transmural pressure (RAPTM) for the right atrium can be calculated by the formula: RAPTM = RAP − PPL [9]. However, in the clinical practice, PPL and PPER are assumed to be equal to intrathoracic pressure (ITP) which is the external pressure around the heart and the lungs. However, it must be noted that ITP is not homogeneously distributed throughout the thorax [10]. The PTM is the actual working pressure that, together with chamber compliance, defines the venous return, cardiac filling, and hence, cardiac output. In clinical practice, PPL can be estimated by measuring the esophageal pressure with an air-filled balloon in the esophagus at end-expiration [11].
The lungs are surrounded by two pleural layers and enclosed by the chest wall and the diaphragm. The two pleural layers ensure the mechanical coupling between lung and the chest wall. PPL is negative in spontaneous breathing and acts as external pressure of the lung and cardiac structures. The PTM for lungs or transpulmonary pressure (PTP) is the difference of alveolar pressure (PAL) and PPL. It decides the lung volume at the end of inhalation, depending on the compliance of the lung within the chest wall [9].
Lung compliance (CL) and chest wall compliance (CCW) defines the total compliance of the respiratory system (CRS): i.e. (1/CRS = 1/CL + 1/CCW) [12].
Blood flow through the lungs depends on the driving pressure for the blood, that is (mean pulmonary artery pressure [PAPm] − mean left atrial pressure [LAPm]) and pulmonary vascular resistance (PVR) [13]. With a pulmonary artery catheter, LAPm can be estimated by measuring pulmonary artery occlusion pressure (PAOP).
The pulmonary vascular resistance is increased by vasoconstriction, hypoxic (Euler-Lilijestrand reflex [14]) or hypercapnic pulmonary vasoconstriction [15]. Pulmonary vessels are more compliant than systemic vessels, compressible by surrounding lungs and act as Starling resistors. A vessel working as a Starling resistor, can change its diameter and the related resistance to flow according to its surrounding pressure. Increased extravascular pressure (increased PAL or PPL) diminishes transmural pulmonary vascular pressure, resulting in an increased PVR [16]. During the respiratory cycle at end-expiration, when the lung is at its functional residual capacity (FRC) and where the resistance of inter-alveolar vessels equals the resistance of extra-alveolar vessels, PVR is the lowest [17].
Effects of Mechanical Ventilation on Intrathoracic Pressure
During the inspiratory phase of mechanical ventilation, the machine delivers a tidal volume through an artificial airway to the lungs leading to positive PAL and PPL. The transmission of airway pressure to the pleural space is lower if the CRS of the system is low, as in acute respiratory distress syndrome (ARDS), which has reduced lung compliance and therefore, has less hemodynamic effect by heart-lung interactions compare to increased compliant system as seen in chronic obstructive pulmonary disease (COPD) [18].
With the application of positive end-expiratory pressure (PEEP) and the absence of spontaneous breathing efforts, PPL is positive throughout the respiratory cycle. In contrast, with unforced spontaneous breathing, PPL always remains negative.
The physiological consequences of these changes in PPL and PTP are as follows:
-
1.
An elevated PAL combined with the supine position alters pulmonary blood flow by creating lung areas with zone 1 conditions (compression of alveolar vessels) and increasing the proportion of areas with zone 2 conditions (compression of veins), causing increased PVR and dead space ventilation.
-
2.
An increased ITP reduces PTM of large intrathoracic blood vessels as the vena cava and thoracic aorta, thereby diminishing intrathoracic blood volume.
-
3.
The ITP is also transmitted to the pericardium, which encloses the heart.
These physiological consequences are due to respiratory swings in intrathoracic pressure, and their effects on hemodynamics are predictable; for example, as RAP increases with positive ITP, the venous return goes down [19, 20]. This could lead to profound and sometimes abrupt cardio-circulatory effects with positive pressure ventilation. This phenomenon should be expected and patients need appropriate monitoring (Fig. 5.2). The overall effect of positive pressure on preload, afterload, and pump function will be explained in detail later.
The Pump
The pumping work of the heart is to maintain adequate and optimum cardiac output. Cardiac output is determined by the heart rate and stroke volume. Stroke volume is the amount of blood expelled from the left ventricle (LV) into the systemic circulation with each heartbeat. Averaged over several seconds to minutes, LV stroke volume equals right ventricular stroke volume. The LV preload, myocardial contractility, and afterload are the main determinants of stroke volume.
Venous Return and Ventricular Preload
Cardio-circulatory physiology and heart-lung interactions can best be understood if we familiarize ourselves with determinants of venous return and the functioning of the right ventricle. Of the total blood volume, only about 15% exerts pressure, and the rest is said to be “unstressed volume”, which theoretically exerts no pressure (or minimal pressure) on the walls of the vessels. Hence, unstressed volume is the blood volume that resides in the vessels at near-zero transmural pressure (PTM), or distending pressure. The additional blood volume above unstressed volume generating positive PTM is called stressed volume. Mean systemic filling pressure (MSFP) represents the pressure generated by elastic recoil of the systemic circulation during a no-flow state. This pressure represents which is thought to push blood towards the right atrium along a pressure gradient [21,22,23].
Stressed volume can be altered by a change of total intravascular volume and recruitment or de-recruitment of unstressed volume by a change in the vessel tone using vasopressors or vasodilators, which will alter the MSFP accordingly [22, 24, 25].
Venous return is directly proportional to the pressure gradient between MSFP and RAP and inversely proportional to the resistance of the vessels (Rv). MSFP as upstream and RAP as downstream pressure [26] for venous return create the pressure gradient necessary to overcome the resistance to venous return (VR) [27, 28].
In spontaneously breathing patients, because of negative PPL, RAP decreases and creates a higher-pressure gradient for venous return, resulting in higher return. On the other hand, during positive pressure ventilation (PPV), PPL increases and is partially transmitted to the right atrium, whose intracavitary pressure (RAP) rises, leading a decrease in pressure gradient and venous return.
The Starling curve shifts to the right leading to a decrease in cardiac output and venous return. Under mechanical ventilation, right ventricular preload is mainly affected by changes in PPL, whereas left ventricular preload is mainly affected by changes in PTP [29] (Fig. 5.3).
Effects of mean intrathoracic pressure on systemic vascular return. Systemic venous return to the right atrium is passive, with blood flow occurring due to pressure gradient between the superior/inferior vena cava and the right atrium. Psv systemic venous pressure, RAP right atrial pressure, PPV positive pressure ventilation
Ventricular Afterload
Afterload is defined as the force opposing ventricular ejection of blood [30]. Afterload can be approached by assessing ventricular wall tension or vascular resistance and impedance [31]. We will now discuss both ventricles separately, given their relatively different muscle mass, position, and orientation.
Left Ventricular Afterload
The work of the left ventricle depends on the aortic elastance (ΔP/ΔV) (i.e., to accommodate and release a proportion of each stroke volume temporarily) and the overall resistance of the arterial vessel tree [32]. Subtle intra-thoracic pressure swings like those during spontaneous respiration cause only minor cyclic changes in left ventricular afterload in healthy humans. However, the cardiac output can be considerably decreased by forced spontaneous inspiration or a Muller manoeuver due to an abrupt increase in transmural pressure and afterload [33].
During positive pressure ventilation or by the application of PEEP, ITP and concomitantly PPL rise. PTM of the LV and, to a lesser extent, of the intrathoracic part of the aorta falls, while PTM in the abdominal aorta remains higher, resulting in a net afterload reduction and facilitating blood flow from the intrathoracic to the abdominal compartment. These changes seem to be mainly mediated by changes in PPL [29].
With LV afterload reduction, the application of continuous positive airway pressure (CPAP) in spontaneously breathing patients or pressure support ventilation with PEEP in sedated patients can be a valuable supportive measure in the treatment of acutely decompensated left ventricular failure [34].
Right Ventricular Afterload
Blood is pumped by the right ventricle (RV) into the pulmonary vasculature, which is a highly compliant low-pressure system. Alterations in RV outflow are mainly mediated through changes in ITP [29, 35]. Changes in ITP can strongly affect transmural pulmonary vascular pressure and PVR, and thereby RV output. During spontaneous breathing, inspiration is associated with negative PPL, which distend the pulmonary vasculature, reducing RV afterload and thereby increases RV output.
During mechanical ventilation, tidal breathing increases PPL, thus reducing transmural pulmonary vascular pressure and consequently elevating RV afterload and decreasing RV output. In individuals with pre-existing right ventricular dysfunction, or severe hypoxic pulmonary vasoconstriction in the context of ARDS, mechanical ventilation (cyclical tidal inflation) may precipitate RV failure by increasing RV afterload [29, 35,36,37,38,39].
Since the RV possesses much lesser contractile reserves, acute elevations of afterload are poorly tolerated by the RV compared with the LV [39]. The lowest PVR during the respiratory cycle is seen at end-expiration at FRC. PVR rises at lung volumes both below and above the FRC [17].
Ventricular Interdependence
The LV and RV work as serial pumps connected by the pulmonary and systemic vasculature. Through their electrical and mechanical synchronization, they work in parallel within the confines of the pericardium. Due to the shared interventricular septum and the pericardial constraints, the diastolic pressure of one ventricle directly affects the diastolic filling of the other, and this phenomenon is called interventricular dependence [40, 41].
When the RV volume increases, the septum bulges to the left, leading to a decline in LV filling. This phenomenon can be seen in conditions with RV afterload elevation like pulmonary embolism, pulmonary hypertension, or mechanical ventilation. Increased RV pressure and volume leads to interventricular septum flattening or convex bowing into the LV cavity, thus decreasing the LV volume and filling. Clinically important examples of interventricular dependence are pericardial tamponade, status asthmaticus, and COPD [42].
Heart-Lung Interactions: Clinical Application
The complex cardiopulmonary physiology interplay makes heart-lung interactions in a ventilated patient, very important, as mechanical ventilation can provoke cardiovascular instability [41]. An understanding of heart-lung interactions offers possibilities to predict hemodynamic alterations and to decide appropriate treatment modalities, especially guiding volume expansion, within the framework of functional hemodynamic monitoring [42].
Functional Hemodynamic Monitoring
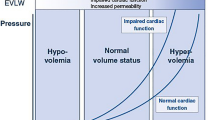
Concept of Fluid Responsiveness
Fluid depletion or hypovolemia is often the primary or contributory cause of acute circulatory failure, except in cases of cardiogenic shock. In intensive care units (ICUs), the decision regarding volume expansion is frequent and many a times quiet challenging. Fluid administration will lead to an increase in cardiac output only if the ventricles operate on the ascending (steep) portion of the frank starling curve (Fig. 5.4). If the preload of the ventricles operates on the flat portion of the frank starling curve, then volume expansion may only exert adverse effects without increasing the cardiac output or any hemodynamic benefit [43].
Schematic representation of the Frank–Starling relationship between ventricular preload and stroke volume. A given change in preload induces a larger change in stroke volume when the ventricle operates on the ascending portion of the relationship ((a) condition of preload dependence) than when it operates on the flat portion of the curve ((b) condition of preload independence)
Excessive fluid administration has been associated with a significant increase in mortality, acute kidney injury, and increased duration of mechanical ventilation [3]. Positive indicators of fluid responsiveness also do not justify fluid therapy by themselves [2, 43, 44]. The literature supports that only 50% of patients are fluid-responsive in patients with acute circulatory failure [4]. Besides, fluid responsiveness does not predict fluid tolerance. The cardinal purpose of fluid administration in circulatory shock is to increase tissue oxygenation, not cardiac output. To achieve this goal, fluid must be administered only if required (in circulatory shock), and are fluid responders (positive fluid responsiveness) and fluid tolerant. Hence, the primary purpose of fluid responsiveness is to determine which patients should not be given fluid. Several strategies have been developed to identify fluid responsiveness before fluid administration for resuscitation to avoid fluid overload and its complications. Various static and dynamic parameters have been evaluated to identify responders to fluid therapy [2].
The static parameters are inaccurate to predict preload responsiveness [44] (Fig. 5.4). Despite our current knowledge, there has been a continued and widespread use of static parameters to predict fluid responsiveness. According to a recently conducted study, fluid challenges in intensive care: the FENICE study [45], the CVP was used most often as a predictor for fluid responsiveness. The above observation is interesting, considering that the CVP is a poor variable to predict fluid responsiveness [46,47,48].
Other bedside indicators of preload, such as the RV end-diastolic volume (evaluated by thermodilution) and the LV end-diastolic area (measured by echocardiography), have also been tested as predictors of fluid responsiveness. Unfortunately, these parameters were also not found accurate enough to differentiate between fluid responder and non-responders [42, 49,50,51,52,53].
Studies have shown that the right atrial and pulmonary artery occlusion pressures do not always reflect transmural pressures in patients with external or intrinsic positive end-expiratory pressure (PEEP) [42, 46, 54]. In patients with decreased left ventricular compliance, the pulmonary artery occlusion pressure is not always a reliable indicator of left ventricular preload [47]. Measurement of RV end-diastolic volume by thermodilution is influenced by tricuspid regurgitation [55], which is frequently encountered in critically ill patients with pulmonary hypertension.
Studies have found that the left ventricular end-diastolic area, as measured by echocardiography, may not always accurately reflect the left ventricular end-diastolic volume and therefore may not be a reliable indicator of left ventricular preload [56]. In some cases, right ventricular dilation may offset the hemodynamic benefits of volume expansion, even when left ventricular preload is low [57]. Finally, the preload-induced changes in stroke volume also depend on contractility and afterload.
Dynamic Indicators for Fluid Responsiveness
The poor performance of static parameters has paved the way for the development of dynamic parameters based on heart-lung interaction for predicting fluid responsiveness. Dynamic indices have been shown to reduce unnecessary fluid loading and potential complications of volume overload. Dynamic indices based on heart-lung interactions are classified into two broad categories.
-
1.
Invasive assessment of respiratory changes in LV stroke volume
-
(a)
Stroke volume variation with respiration
-
(b)
Pulse pressure variation with respiration
-
(c)
Systolic pressure variation with respiration
-
(a)
-
2.
Non-invasive assessment of respiratory changes in LV stroke volume
-
(a)
Doppler echocardiography for measuring changes in LV stroke volume (VTI) with respiration
-
(b)
Echocardiographic assessment of the vena cava
-
(c)
Estimation of MSFP with ventilator maneuvers
-
(d)
Pulse pressure variation with respiration infrared photoplethysmography coupled with the volume clamp technique
-
(a)
Invasive Assessment of Respiratory Changes in LV Stroke Volume
Measurement of Stroke volume variation (SVV) and Pulse pressure variation by minimally invasive arterial pressure-based CO monitoring techniques (PiCCO, LiDCO) induced by mechanical ventilation were the first techniques used to assess fluid responsiveness. Fluid responsiveness may be assessed by calculating the variation in stroke volume (Δ SVV) with respiration which can be calculated as follow.
where SVmax and SVmin are the maximal and minimal values of stroke volume over a single respiratory cycle (Fig. 5.5). The difference between the maximal and minimal values of stroke volume over a single respiratory cycle is called stroke volume variation (SVV).
The reference stroke volume is measured during an end-expiratory pause (line of reference) and is divided into two components: Delta up (Δ up) and Delta down (Δ down). Delta up is the difference between the maximal and the reference stroke volume pressure. Delta down is the difference between the reference and the minimal stroke pressure (Fig. 5.5). In mechanically ventilated patients, hypovolemia has been shown to increase SPV [58], whereas volume expansion decreases SPV [58, 59]. The threshold of SVV >12% has been shown to predict fluid responsiveness with sensitivity and specificity greater than 85%.
Interestingly, Coriat et al. [59] reported a significant relationship between Δ SV down before fluid infusion and the increase in the cardiac index in response to volume expansion in patients after aortic surgery. Therefore, Δ SV down can be considered an indicator of fluid responsiveness because the higher Δ down before volume expansion, greater the increase in the cardiac index in response to fluid infusion.
Pulse Pressure Variation
Pulse pressure is the difference between systolic and diastolic pressure. It is directly proportional to LV stroke volume and inversely related to arterial compliance [60]. An increase in pleural pressure induced by mechanical ventilation affects both systolic and diastolic pressures. Hence, the pulse pressure is not directly influenced by the cyclic changes in pleural pressure. Instead, the respiratory changes in LV stroke volume are reflected by changes in peripheral pulse pressure during the respiratory cycle [61].
The fluid responsiveness may be assessed by calculating the respiratory changes in pulse pressure (PP) as follows.
where PPmax and PPmin are the maximal and minimal values of pulse pressure over a single respiratory cycle, respectively. The pulse pressure (systolic minus diastolic pressure) is maximal (PPmax) at the end of the inspiratory period and minimal (PPmin) three heartbeats later (i.e., during the expiratory period) (Fig. 5.5).
Michard and colleagues showed a good prediction of fluid responsiveness in septic patients with a PPV ≥12% [62]. In recent light of the evidence, calculating PPV may be of particular help in deciding whether to institute volume expansion. Indeed, if PPV is low (<13%), then a beneficial hemodynamic effect of volume expansion is very unlikely, and inotropes or vasoactive drugs should be started in order to improve hemodynamics. In contrast, if PPV is high (>13%), then a significant increase in the cardiac index in response to the fluid infusion is very likely.
PPV of the arterial pressure is caused by preload and stroke volume changes in the right ventricle. Any factor interfering with the pulmonary vasculature or function may affect PPV [63, 64]. Its apparent simplicity may distract the clinician from several important pitfalls. PPV and SVV are influenced by any spontaneous respiratory effort [42], tidal volume (needs to be larger than 8 ml/kg, which is not current practice in lung-protective ventilation) [42], respiratory rate and pulmonary transit time [65], and the CRS [66]. The absence of sinus rhythm and frequent ectopic beats render PPV unusable. Most critically ill patients have above-mentioned limitations affecting the valid interpretation of PPV [67, 68]. The most important limitation of PPV is RV dysfunction, which also causes the arterial pressure to undulate because of smaller stroke volumes with increased afterload during mechanical inspiration.
In order to avoid deleterious volume loading, PPV should not be seen as a marker of volume responsiveness per se [35, 42, 69, 70] but rather as an indicator of LV function depending on RV stroke volume. A failure to increase cardiac output following volume expansion calls for an immediate diagnostic evaluation of the RV. If cardiac output is not augmented or vasopressors are not decreased following a volume challenge, no further volume should be applied, and careful evaluation of the RV function should be performed, if PPV is present.
If a patient’s blood volume is centralized owing to adrenergic (endogenous or exogenous) vasoconstriction with concomitant insufficient tissue perfusion, a negative PPV does not exclude the need for volume infusion. Venous return is maintained by vasoconstriction that shifts volume from the pool of unstressed volume to the pool of stressed volume. In this case, volume expansion may reduce the dose of vasopressor agents and restore tissue perfusion by normalizing unstressed volume and reducing vasoconstriction.
Overall, volume administration should be done when we have critical tissue oxygenation, evidence of fluid responsiveness and a positive effect on oxygen delivery can be documented. The assessment of cardiac preload dependence is helpful in predicting volume expansion efficacy and the hemodynamic effects of any therapy that induces changes in cardiac preload conditions.
In this regard, PPV has been shown to be useful in monitoring the hemodynamic effects of PEEP in mechanically ventilated patients with acute lung injury. The negative effects of increased pleural pressure on RV filling and increased transpulmonary pressure on RV afterload lead to decreased RV stroke volume, LV preload and thus decreased mean cardiac output.
Michard et al. assessed the clinical use of respiratory changes in arterial pulse pressure to monitor the hemodynamic effects of PEEP [71].
In their study on 14 mechanically ventilated patients with acute lung injury, first, a ∆ PP on zero end-expiratory pressure (ZEEP) was closely correlated with the PEEP-induced decrease in cardiac index; higher the PPV was on ZEEP, greater the decrease in cardiac index when PEEP was applied (Fig. 5.6). Also, the increase in ∆PP induced by PEEP was correlated with the decrease in cardiac index, such that changes in ∆ PP from ZEEP to PEEP could be used to assess the hemodynamics effects of PEEP without the need for a pulmonary artery catheter. Finally, when cardiac index decreased with PEEP, volume expansion induced an increase in cardiac index that was proportional to PPV before fluid infusion.
Relationship between the respiratory changes in pulse pressure on ZEEP (y-axis) and the PEEP-induced cardiac index changes (x-axis) in 14 ventilated patients with acute lung injury. The higher DPP is on ZEEP, the more marked the decrease in the cardiac index induced by PEEP [71]
Because the PP depends not only on stroke volume but also on arterial compliance, large changes in pulse pressure could theoretically be observed despite small changes in LV stroke volume if arterial compliance is low (elderly patients with peripheral vascular disease). Similarly, if arterial compliance is high (young patients without any vascular disease) despite large changes in LV stroke volume, only small changes in pulse pressure could be observed.
Non-invasive Assessment of Respiratory Changes in LV Stroke Volume
Although less invasive than pulmonary artery catheterization, femoral or radial arterial catheterization remains an invasive procedure. Infrared photoplethysmography coupled with the volume clamp technique [72] allows a non-invasive and continuous measurement of finger blood pressure, which has been shown to track changes in blood pressure accurately [73]. In mechanically ventilated patients, a close correlation and a good agreement between ∆PP measured from intra-arterial recordings and ∆PP measured noninvasively using the continuous measurement of finger blood pressure has been established [74].
Transthoracic echocardiographic measurement of variations of inferior vena cava (IVC) diameter induced by mechanical ventilation has been shown to predict preload responsiveness with reasonable sensitivity and specificity [50, 51, 75].
In a mechanically ventilated patient with no spontaneous breathing efforts, due to an increase in intrathoracic pressure, the IVC dilates during inspiration reaching maximum diameter. It collapses during expiration as the intrathoracic pressure drops, giving a minimum diameter. The percentage variation of IVC during inspiration against expiration gives the IVC distensibility index.
Distensibility index >18% offers 90% sensitivity and specificity in identifying fluid responders from non-responders [53, 76].
In spontaneously breathing patients, the IVC collapses on inspiration as intrathoracic pressure becomes negative, and the degree of IVC collapsibility during inspiration can be used to predict preload responsiveness (IVC collapsibility index) [52].
IVCmax maximum IVC diameter during expiration, IVCmin minimum IVC diameter during inspiration.
Currently, there is insufficient evidence to support its use, but the collapsibility index of >42% may predict increase in cardiac output after fluid challenge.
The change in stroke volume over the respiratory cycle in mechanically ventilated patients assessed noninvasively by transthoracic echocardiography can be used to predict preload responsiveness. Indeed, by assuming that aortic annulus diameter is constant over the respiratory cycle, the changes in aortic blood flow should reflect changes in LV stroke volume.
Stroke volume is calculated using the velocity time integral (VTI).
Cardiac output can be derived by multiplying SV to heart rate. By tracing the largest and smallest VTI over respiratory cycle, stroke volume variation (SVV) can be calculated.
Cardiac output measured by this method is comparable to the thermodilution method using a pulmonary artery catheter. SVV of >14% has a very high positive predictive value, and <10% has a high negative predictive value for fluid responsiveness.
Other Clinically Significant Clinical Interactions
While weaning a ventilated patient, abrupt transfer from mechanical ventilation to spontaneous breathing leads to an increase in LV preload and afterload. In a patient with compromised LV function, this might precipitate a left-side cardiac failure and cardiogenic pulmonary edema leading to weaning failure. Similarly, a patient presenting with respiratory distress due to cardiogenic pulmonary edema could greatly benefit from a trial of CPAP, because of the clear advantage of positive pressure in decreasing both preload and afterload.
In obstructive sleep apnea, patients exhibit inspiratory muscular efforts against a collapsed upper airway creating a strongly negative PPL, which is transmitted to the intrathoracic large veins and the right atrium, augmenting venous return. This leads to dilation of the RV accompanied by a shift of the interventricular septum towards the LV, reducing LV compliance and stroke volume (pulsus paradoxus) [77, 78]. Chronic right heart changes (cor pulmonale) and RV dysfunction are common in patients with severe obstructive sleep apnea. Patients with an impaired RV function cannot adapt to frequent and sudden increases in venous return and are prone to RV failure. Negative PPL also increases left ventricular afterload. Further arterial desaturation occurs during these apneic episodes leads to hypoxic pulmonary vasoconstriction, resulting in cor pulmonale in patients with severe obstructive sleep apnea. Nocturnal continuous positive airway pressure (CPAP) therapy helps to keep the upper airway open and prevent RV dysfunction and cor pulmonale in patients with severe OSA [77, 78].
Despite the widespread use of lung protective ventilation strategies [79], which may mitigate the mechanical effects on the right ventricle due to lower airway pressures, acute cor pulmonale in patients with ARDS is still highly prevalent. The risk of developing acute cor pulmonale becomes higher with poor oxygenation, hypercapnia, high ventilator pressures and pneumonia as the cause of ARDS [80]. In patients with ARDS, these effects are aggravated by hypoxic or hypercapnic pulmonary vasoconstriction, pulmonary micro-thrombosis, changes in West zones, and lung de-recruitment [81], all leading to pulmonary hypertension and a worse prognosis [82]. Thereby, RV decompensates as a result of high afterload. For the similar reasons, ARDS patients can decompensate during recruitment procedure; therefore, before recruitment, RV systolic function is to be evaluated.
In conditions like exacerbations of COPD or status asthmaticus, high lung compliance (CL) facilitates pressure transmission from the lung to the pulmonary vasculature, so these patients are prone to develop acute cor pulmonale. The high airway resistance leads to incomplete exhalation with air trapping, dynamic over-inflation, and auto-PEEP [83, 84], resulting in elevated afterload leading to RV dysfunction.
Cardiopulmonary Changes in Prone Positioning
Prone positioning has emerged as a promising therapy for patients of ARDS with refractory hypoxemia. Placing a patient in the prone position has important implications for both venous return and RV function. During prone ventilation, there is an increase in intra-abdominal pressure which leads to increase in central blood volume due to the shift of blood from the splanchnic into the thoracic circulation, which may induce recruitment of pulmonary microvasculature, increase in pulmonary capillary wedge pressure, and reduction in PVR and RV afterload. It is to be noted that the improved venous return will only be realized in the absence of a simultaneous rise in the resistance to venous return. Therefore, careful consideration should be paid to a patient’s volume status before initiating prone positioning. Additionally, the heterogeneity of lung involvement, compliance of chest wall and ventilation strategies utilized will determine to what extent the intra-thoracic milieu favours diminished RV preload, afterload, or some combination thereof [85, 86].
It follows that careful consideration should be given to the underlying cardiac function as well as the relative contributions of the pulmonary and chest wall compliance to the overall compliance of the respiratory system. Integration of these multiple, co-varying physiological elements may explain conflicting hemodynamic both in ARDS and other mechanically-ventilated patient populations.
Case Vignette
Why did the critical care team decide to use heart-lung interactions to assess fluid responsiveness in Mr. J?
-
Answer: The critical care team suspected that Mr. J might be volume depleted, and they wanted to assess his fluid responsiveness. Heart-lung interactions are a useful tool for assessing fluid responsiveness in critically ill patients. The PLR maneuver is a noninvasive method that can be used to predict fluid responsiveness by observing the changes in stroke volume or cardiac output.
What was the hemodynamic response observed during the PLR maneuver, and what does it indicate?
-
Answer: During the PLR maneuver, the team observed an increase in the stroke volume (SV) by 20%, indicating that Mr. J was fluid responsive. This increase in SV is a positive response to the PLR and indicates that the patient's cardiac preload was increased, leading to an increase in stroke volume. This response indicates that the patient may benefit from fluid administration to improve their hemodynamic status.
Limitations: Although heart-lung interactions are a useful tool for assessing fluid responsiveness, interpreting the results can be challenging. The PLR maneuver can produce false-positive results in patients with elevated intra-abdominal pressure or impaired venous return.
Lack of specificity: Heart-lung interactions are not specific to fluid responsiveness. Other factors, such as changes in vascular tone, inotropic agents, and positive pressure ventilation, can also affect the hemodynamic response to the PLR maneuver.
Conclusions
Ventilation can alter cardiovascular function by altering lung volume, intrathoracic pressure (ITP) and by increasing metabolic demands. Such cardiopulmonary interactions can have deleterious effects in critically ill patients. A thorough understanding of these interactions can help us to differentiate between fluid responders and non-responders and thus prevent the probable complications of an inappropriate fluid therapy.
Take Home Messages
-
The concept of predicting fluid responsiveness emerged from a twofold observation:
-
First, the potential harm caused by fluid administration
-
Second, the variable efficacy of fluid resuscitation
-
-
The ability to assess fluid responsiveness enables clinicians
-
To avoid administering harmful treatments to patients who do not require them
-
To provide fluids when they are needed
-
-
Dynamic measures of fluid responsiveness allow for personalized or even individualized resuscitation strategies that can be tailored to each patient’s individual needs, regardless of the type of fluid being used.
-
It is important to note that these “fluid responsiveness” measures must be used carefully in the most critically ill patients, as they must balance the need for aggressive restoration of blood flow with the risk of fluid overload.
-
Fluid responsive measures are an essential part of the arsenal of strategies that allow for personalized and individualized treatment of the most severe patients.
-
However, as it is equally crucial to avoid fluid accumulation, and clinicians must be cautious not to administer fluids when they are not necessary.
-
In the case of fluid accumulation syndrome (FAS), the presence of fluid unresponsiveness can serve as a trigger and/or safety parameter to guide fluid removal and restore euvolemia to the patient, thus ensuring optimal outcomes.
References
Cecconi M, De Backer D, Antonelli M, Beale R, Bakker J, Hofer C, Jaeschke R, Mebazaa A, Pinsky MR, Teboul JL, Vincent JL, Rhodes A. Consensus on circulatory shock and hemodynamic monitoring. Task force of the European Society of Intensive Care Medicine. Intensive Care Med. 2014;40(12):1795–815. https://doi.org/10.1007/s00134-014-3525-z.
Monnet X, Malbrain MLNG, Pinsky MR. The prediction of fluid responsiveness. Intensive Care Med. 2023;49(1):83–6. https://doi.org/10.1007/s00134-022-06900-0.
Messmer AS, Zingg C, Müller M, Gerber JL, Schefold JC, Pfortmueller CA. Fluid overload and mortality in adult critical care patients-a systematic review and meta-analysis of observational studies. Crit Care Med. 2020;48(12):1862–70. https://doi.org/10.1097/CCM.0000000000004617.
Tobin MJ. Effect of mechanical ventilation on heart-lung interactions principles and practice of mechanical ventilation. 3rd ed. New York: McGraw Hill; 2012. (Chapter 36).
Magder S, Verscheure S. Proper reading of pulmonary artery vascular pressure tracings. Am J Respir Crit Care Med. 2014;190(10):1196–8.
Marini JJ, Culver BH, Butler J. Mechanical effect of lung distention with positive pressure on cardiac function. Am Rev Respir Dis. 1981;124(4):382–6.
Holt JP, Rhode EA, Kines H. Pericardial and ventricular pressure. Circ Res. 1960;8(6):1171–81.
Tyberg JV, Smith ER. Ventricular diastole and the role of the pericardium. Herz. 1990;15(6):354–61.
Gubbler MR, Wigger O, Berger D. Swiss Med Wkly. 2017;147:w14491.
Lansdorp B, Hofhuizen C, van Lavieren M, van Swieten H, Lemson J, van Putten MJ, et al. Mechanical ventilation-induced intrathoracic pressure distribution and heart-lung interactions. Crit Care Med. 2014;42(9):1983–90.
Kingma I, Smiseth OA, Frais MA, Smith ER, Tyberg JV. Left ventricular external constraint: relationship between pericardial, pleural and esophageal pressures during positive end-expiratory pressure and volume loading in dogs. Ann Biomed Eng. 1987;15(3-4):331–46.
Rahn H, Otis AB, et al. The pressure-volume diagram of the thorax and lung. Am J Phys. 1946;146(2):161–78.
Naeije R. Pulmonary vascular resistance. A meaningless variable? Intensive Care Med. 2003;29(4):526–9.
Lumb AB, Slinger P. Hypoxic pulmonary vasoconstriction: physiology and anesthetic implications. Anesthesiology. 2015;122(4):932–46.
Dorrington KL, Talbot NP. Human pulmonary vascular responses to hypoxia and hypercapnia. Pflugers Arch. 2004;449(1):1–15.
West JB, Dollery CT, Naimark A. Distribution of blood flow in isolated lung; relation to vascular and alveolar pressures. J Appl Physiol. 1964;19:713–24.
Whittenberger JL, McGregor M, Berglund E, Borst HG. Influence of state of inflation of the lung on pulmonary vascular resistance. J Appl Physiol. 1960;15:878–82.
Jardin F, Genevray B, Brun-Ney D, Bourdarias JP. Influence of lung and chest wall compliances on transmission of airway pressure to the pleural space in critically ill patients. Chest. 1985;88(5):653–8.
Feihl F, Broccard AF. Interactions between respiration and systemic hemodynamics. Part I: basic concepts. Intensive Care Med. 2009;35(1):45–54.
Feihl F, Broccard AF. Interactions between respiration and systemic hemodynamics. Part II: practical implications in critical care. Intensive Care Med. 2009;35(2):198–205.
Magder S. Volume and its relationship to cardiac output and venous return. Crit Care. 2016;20(1):271. Correction in: Critical Care. 2017;21:16.
Magder S, De Varennes B. Clinical death and the measurement of stressed vascular volume. Crit Care Med. 1998;26(6):1061–4.
Berger D, Moller PW, Weber A, Bloch A, Bloechlinger S, Haenggi M, et al. Effect of PEEP, blood volume, and inspiratory hold maneuvers on venous return. Am J Physiol Heart Circ Physiol. 2016;311(3):794–806.
Magder S, Vanelli G. Circuit factors in the high cardiac output of sepsis. J Crit Care. 1996;11(4):155–66.
Bloch A, Berger D, Takala J. Understanding circulatory failure in sepsis. Intensive Care Med. 2016;42(12):2077–9.
Moller PW, Winkler B, Hurni S, Heinisch PP, Bloch AM, Sondergaard S, et al. Right atrial pressure and venous return during cardiopulmonary bypass. Am J Physiol Heart Circ Physiol. 2017;313(2):H408–20.
Berger D, Moller PW, Weber A, Bloch A, Bloechlinger S, Haenggi M, et al. Effect of PEEP, blood volume, and inspiratory hold maneuvers on venous return. Am J Physiol Heart Circ Physiol. 2016;311(3):H794–806.
Sondergaard S, Parkin G, Aneman A. Central venous pressure: soon an outcome-associated matter. Curr Opin Anaesthesiol. 2016;29(2):179–85.
Vieillard-Baron A, Matthay M, Teboul JL, Bein T, Schultz M, Magder S, et al. Experts’ opinion on management of hemodynamics in ARDS patients: focus on the effects of mechanical ventilation. Intensive Care Med. 2016;42(5):739–49.
Reichek N, Wilson J, St John Sutton M, Plappert TA, Goldberg S, Hirshfeld JW. Noninvasive determination of left ventricular end-systolic stress: validation of the method and initial application. Circulation. 1982;65(1):99–108.
Borlaug BA, Kass DA. Invasive hemodynamic assessment in heart failure. Heart Fail Clin. 2009;5(2):217–28.
Walley KR. Left ventricular function: time-varying elastance and left ventricular aortic coupling. Crit Care. 2016;20(1):270.
Buda AJ, Pinsky MR, Ingels NB Jr, Daughters GT, Stinson EB, Alderman EL. Effect of intrathoracic pressure on left ventricular performance. N Engl J Med. 1979;301(9):453–9.
Pinsky MR. Cardiovascular issues in respiratory care. Chest. 2005;128(5):592–7.
Vieillard-Baron A, Loubieres Y, Schmitt JM, Page B, Dubourg O, Jardin F. Cyclic changes in right ventricular output impedance during mechanical ventilation. J Appl Physiol. 1999;87(5):1644–50.
Berger D, Bloechlinger S, Takala J, Sinderby C, Brander L. Heart-lung interactions during neurally adjusted ventilatory assist. Crit Care. 2014;18(5):499.
Mekontso Dessap A, Boissier F, Charron C, Begot E, Repesse X, Legras A, et al. Acute cor pulmonale during protective ventilation for acute respiratory distress syndrome: prevalence, predictors, and clinical impact. Intensive Care Med. 2016;42(5):862–70.
Jardin F, Brun-Ney D, Cazaux P, Dubourg O, Hardy A, Bourdarias JP. Relation between transpulmonary pressure and right ventricular isovolumetric pressure change during respiratory support. Catheter Cardiovasc Diagn. 1989;16(4):215–20.
Pinsky MR. Determinants of pulmonary arterial flow variation during respiration. J Appl Physiol. 1984;56(5):1237–45.
Taylor RR, Covell JW, Sonnenblick EH, Ross J Jr. Dependence of ventricular distensibility on filling of the opposite ventricle. Am J Phys. 1967;213(3):711–8.
Vieillard-Baron A, Schmitt JM, Augarde R, Fellahi JL, Prin S, Page B, et al. Acute cor pulmonale in acute respiratory distress syndrome submitted to protective ventilation: incidence, clinical implications, and prognosis. Crit Care Med. 2001;29(8):1551–5.
Michard F, Teboul JL. Using heart-lung interactions to assess fluid responsiveness during mechanical ventilation. Crit Care. 2000;4:282.
Pinsky MR. Functional haemodynamic monitoring. Curr Opin Crit Care. 2014;20(3):288–93.
Osman D, et al. Cardiac filling pressures are not appropriate to predict hemodynamic response to volume challenge. Crit Care Med. 2007;35(1):64–8.
Cecconi M, et al. Fluid challenges in intensive care: the FENICE study-A global inception cohort study. Intensive Care Med. 2015;41(9):1529–37.
Pinsky MR, Vincent JL, De Smet JM. Estimating left ventricular filling pressure during positive end-expiratory pressure in humans. Am Rev Respir Dis. 1991;143:25–31.
Raper R, Sibbald WJ. Misled by the wedge? The Swan-Ganz catheter and left ventricular preload. Chest. 1986;89:427–34.
Fessler HE, Brower RG, Wise RA, Permutt S. Mechanism of reduced LV afterload by systolic and diastolic positive pleural pressure. J Appl Physiol. 1988;65:1244–50.
Reuse C, Vincent JL, Pinsky MR. Measurements of right ventricular volumes during fluid challenge. Chest. 1990;98:1450–4.
Squara P, Journois D, Estagnasié P, Wysocki M, Brusset A, Dreyfuss D, Teboul JL. Elastic energy as an index of right ventricular filling. Chest. 1997;111:351–8.
Tavernier B, Makhotine O, Lebuffe G, Dupont J, Scherpereel P. Systolic pressure variation as a guide to fluid therapy in patients with sepsis-induced hypotension. Anesthesiology. 1998;89:1313–21.
Tousignant CP, Walsh F, Mazer CD. The use of transesophageal echocardiography for preload assessment in critically ill patients. Anesth Analg. 2000;90:351–5.
Wagner JG, Leatherman JW. Right ventricular end-diastolic volume as a predictor of the hemodynamic response to a fluid challenge. Chest. 1998;113:1048–54.
Teboul JL, Pinsky MR, Mercat A, Anguel N, Bernardin G, Achard JM, Boulain T, Richard C. Estimating cardiac filling pressure in mechanically ventilated patients with hyperinflation. Crit Care Med. 2000;28(11):3631–6.
Spinale FG, Mukherjee R, Tanaka R, Zile MR. The effects of valvular regurgitation on thermodilution ejection fraction measurements. Chest. 1992;101:723–31.
Urbanowicz JH, Shaaban J, Cohen NH, Cahalan MK, Botvinick EH, Chatterjee K, Schiller NB, Dae MW, Matthay MA. Comparison of transesophageal echocardiographic and scintigraphic estimates of left ventricular end-diastolic volume index and ejection fraction in patients following coronary artery bypass grafting. Anesthesiology. 1990;72:607–12.
Magder S. The cardiovascular management of the critically ill patients. In: Pinsky MR, editor. Applied cardiovascular physiology. Berlin: Springer; 1997. p. 28–35.
Alec Rooke G, Schwid HA, Shapira Y. The effect of graded hemorrhage and intravascular volume replacement on systolic pressure variation in humans during mechanical and spontaneous ventilation. Anesth Analg. 1995;80:925–32.
Coriat P, Vrillon M, Perel A, Baron JF, Le Bret F, Saada M, Viars P. A comparison of systolic blood pressure variations and echocardiographic estimates of end-diastolic left ventricular size in patients after aortic surgery. Anesth Analg. 1994;78:46–53.
Berne RM, Levy MN. Physiology. 4th ed. St Louis: Mosby; 1998.
Jardin F, Farcot JC, Gueret P, Prost JF, Ozier Y, Bourdarias JP. Cyclic changes in arterial pulse during respiratory support. Circulation. 1983;68:266–74.
Michard F, Boussat S, Chemla D, Anguel N, Mercat A, Lecarpentier Y, et al. Relation between respiratory changes in arterial pulse pressure and fluid responsiveness in septic patients with acute circulatory failure. Am J Respir Crit Care Med. 2000;162(1):134–8.
Magder S. Clinical usefulness of respiratory variations in arterial pressure. Am J Respir Crit Care Med. 2004;169(2):151–5.
Sondergaard S. Pavane for a pulse pressure variation defunct. Crit Care. 2013;17(6):327.
De Backer D, Heenen S, Piagnerelli M, Koch M, Vincent JL. Pulse pressure variations to predict fluid responsiveness: influence of tidal volume. Intensive Care Med. 2005;31(4):517–23.
De Backer D, Taccone FS, Holsten R, Ibrahimi F, Vincent JL. Influence of respiratory rate on stroke volume variation in mechanically ventilated patients. Anesthesiology. 2009;110(5):1092–7.
Mesquida J, Kim HK, Pinsky MR. Effect of tidal volume, intrathoracic pressure, and cardiac contractility on variations in pulse pressure, stroke volume, and intrathoracic blood volume. Intensive Care Med. 2011;37(10):1672–9.
Mahjoub Y, Lejeune V, Muller L, Perbet S, Zieleskiewicz L, Bart F, et al. Evaluation of pulse pressure variation validity criteria in critically ill patients: a prospective observational multicentre point-prevalence study. Br J Anaesth. 2014;112(4):681–5.
Pinsky MR, Desmet JM, Vincent JL. Effect of positive end-expiratory pressure on right ventricular function in humans. Am Rev Respir Dis. 1992;146(3):681–7.
Vieillard-Baron A, Chergui K, Augarde R, Prin S, Page B, Beauchet A, et al. Cyclic changes in arterial pulse during respiratory support revisited by Doppler echocardiography. Am J Respir Crit Care Med. 2003;168(6):671–6.
Michard F, Chemla D, Richard C, Wysocki M, Pinsky MR, Lecarpentier Y, Teboul JL. Clinical use of respiratory changes in arterial pulse pressure to monitor the hemodynamic effects of PEEP. Am J Respir Crit Care Med. 1999;159:935–9.
Penaz J. Criteria for set point estimation in the volume clamp method of blood pressure measurement. Physiol Res. 1992;41:5–10.
Imholz BP, Wieling W, van Montfrans GA, Wesseling KH. Fifteen years experience with finger arterial pressure monitoring: assessment of the technology. Cardiovasc Res. 1998;38:605–16.
Michard F, Mercat A, Chemla D, Richard C, Teboul JL. Non invasive assessment of respiratory changes in arterial pulse pressure by infrared photoplethysmography in mechanically ventilated patients. Am J Respir Crit Care Med. 1999;159:A520.
Michard F, Boussat S, Chemla D, Anguel N, Mercat A, Lecarpentier Y, Richard C, Pinsky MR, Teboul JL. Relation between respiratory changes in arterial pulse pressure and fluid responsiveness in septic patients with acute circulatory failure. Am J Respir Crit Care Med. 2000;162:134–8.
Diebel L, Wilson RF, Heins J, Larky H, Warsow K, Wilson S. Enddiastolic volume versus pulmonary artery wedge pressure in evaluating cardiac preload in trauma patients. J Trauma. 1994;37:950–5.
Pinsky MR. Sleeping with the enemy: the heart in obstructive sleep apnea. Chest. 2002;121(4):1022–4.
Chai-Coetzer CL, Antic NA, Hamilton GS, McArdle N, Wong K, Yee BJ, et al. Physician decision making and clinical outcomes with laboratory polysomnography or limited-channel sleep studies for obstructive sleep apnea: a randomized trial. Ann Intern Med. 2017;166(5):332–40.
Brower RG, Matthay MA, Morris A, Schoenfeld D, Thompson BT, Wheeler A, Acute Respiratory Distress Syndrome Network. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000;342(18):1301–8.
Mayo P, Mekontso Dessap A, Vieillard-Baron A. Myths about critical care echocardiography: the ten false beliefs that intensivists should understand. Intensive Care Med. 2015;41(6):1103–6.
Duggan M, McCaul CL, McNamara PJ, Engelberts D, Ackerley C, Kavanagh BP. Atelectasis causes vascular leak and lethal right ventricular failure in uninjured rat lungs. Am J Respir Crit Care Med. 2003;167(12):1633–40.
Bull TM, Clark B, McFann K, Moss M, National Institutes of Health/National Heart, Lung, and Blood Institute ARDS Network. Pulmonary vascular dysfunction is associated with poor outcomes in patients with acute lung injury. Am J Respir Crit Care Med. 2010;182(9):1123–8.
Pepe PE, Marini JJ. Occult positive end-expiratory pressure in mechanically ventilated patients with airflow obstruction: the auto-PEEP effect. Am Rev Respir Dis. 1982;126(1):166–70.
Marini JJ. Dynamic hyperinflation and auto-positive end-expiratory pressure: lessons learned over 30 years. Am J Respir Crit Care Med. 2011;184(7):756–62.
Vieillard-Baron A, Charron C, Caille V, et al. Prone positioning unloads the right ventricle in severe ARDS. Chest. 2007;132:1440–6.
Jozwiak M, Teboul JL, Anguel N, et al. Beneficial hemodynamic effects of prone positioning in patients with acute respiratory distress syndrome. Am J Respir Crit Care Med. 2013;188:1428–33.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2024 The Author(s)
About this chapter
Cite this chapter
Singh, A., Srinivasan, S. (2024). Understanding Heart-Lung Interactions: Concepts of Fluid Responsiveness. In: Malbrain, M.L., Wong, A., Nasa, P., Ghosh, S. (eds) Rational Use of Intravenous Fluids in Critically Ill Patients. Springer, Cham. https://doi.org/10.1007/978-3-031-42205-8_5
Download citation
DOI: https://doi.org/10.1007/978-3-031-42205-8_5
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-42204-1
Online ISBN: 978-3-031-42205-8
eBook Packages: MedicineMedicine (R0)