Abstract
The surgical management of spinal metastases has unique challenges not encountered in other aspects of spine surgery due to the needs of the oncologic patient. Among the key steps in the surgical management is the decision-making process, which must take into account the systemic and adjuvant therapies that are also necessary for systemic and local control of the disease. Decision-making frameworks, such as the NOMS system, have been designed to take into account the multiple factors that can affect the prognosis of the oncologic patient and reach an optimal surgical plan that incorporates available adjuvant treatment, such as radiation therapy. Surgical intervention for spinal metastases has evolved from large reconstructive procedures to less invasive techniques, which still allow for the preservation of neural function and restoration of spinal stability, but with the strategy of selecting the optimal intervention which can best synergize with available adjuvant therapies for effective local disease control. Advancement of surgical strategies such as “separation surgery” and minimally invasive percutaneous stabilization techniques can achieve surgical goals with decreased morbidity and shortened recovery times, which allows for minimal disruption of adjuvant or systemic therapies. The development of conformal radiation techniques such as radiosurgery has greatly assisted in achieving these goals.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Bollen L, et al. Prognostic factors associated with survival in patients with symptomatic spinal bone metastases: a retrospective cohort study of 1 043 patients. Neuro-Oncology. 2014;16(7):991–8.
Groenen KHJ, et al. The Dutch national guideline on metastases and hematological malignancies localized within the spine; a multidisciplinary collaboration towards timely and proactive management. Cancer Treat Rev. 2018;69:29–38.
Leithner A, et al. Predictive value of seven preoperative prognostic scoring systems for spinal metastases. Eur Spine J. 2008;17(11):1488–95.
Tomita K, et al. Surgical strategy for spinal metastases. Spine (Phila Pa 1976). 2001;26(3):298–306.
Tokuhashi Y, et al. A revised scoring system for preoperative evaluation of metastatic spine tumor prognosis. Spine (Phila Pa 1976). 2005;30(19):2186–91.
Laufer I, et al. The NOMS framework: approach to the treatment of spinal metastatic tumors. Oncologist. 2013;18(6):744–51.
Bilsky MH, et al. Reliability analysis of the epidural spinal cord compression scale. J Neurosurg Spine. 2010;13(3):324–8.
Gerszten PC, Mendel E, Yamada Y. Radiotherapy and radiosurgery for metastatic spine disease: what are the options, indications, and outcomes? Spine (Phila Pa 1976). 2009;34(22 Suppl):S78–92.
Lovelock DM, et al. Correlation of local failure with measures of dose insufficiency in the high-dose single-fraction treatment of bony metastases. Int J Radiat Oncol Biol Phys. 2010;77(4):1282–7.
Laufer I, et al. Local disease control for spinal metastases following “separation surgery” and adjuvant hypofractionated or high-dose single-fraction stereotactic radiosurgery: outcome analysis in 186 patients. J Neurosurg Spine. 2013;18(3):207–14.
Fisher CG, et al. A novel classification system for spinal instability in neoplastic disease: an evidence-based approach and expert consensus from the Spine Oncology Study Group. Spine (Phila Pa 1976). 2010;35(22):E1221–9.
Newman WC, Laufer I, Bilsky MH. Neurologic, oncologic, mechanical, and systemic and other decision frameworks for spinal disease. Neurosurg Clin N Am. 2020;31(2):151–66.
Young RF, Post EM, King GA. Treatment of spinal epidural metastases. Randomized prospective comparison of laminectomy and radiotherapy. J Neurosurg. 1980;53(6):741–8.
Gilbert RW, Kim JH, Posner JB. Epidural spinal cord compression from metastatic tumor: diagnosis and treatment. Ann Neurol. 1978;3(1):40–51.
Patchell RA, et al. Direct decompressive surgical resection in the treatment of spinal cord compression caused by metastatic cancer: a randomised trial. Lancet. 2005;366(9486):643–8.
Steffee AD, Biscup RS, Sitkowski DJ. Segmental spine plates with pedicle screw fixation. A new internal fixation device for disorders of the lumbar and thoracolumbar spine. Clin Orthop Relat Res. 1986;203:45–53.
Demura S, et al. Total en bloc spondylectomy for spinal metastases in thyroid carcinoma. J Neurosurg Spine. 2011;14(2):172–6.
Cloyd JM, et al. En bloc resection for primary and metastatic tumors of the spine: a systematic review of the literature. Neurosurgery. 2010;67(2):435–44; discussion 444–5.
Al-Omair A, et al. Surgical resection of epidural disease improves local control following postoperative spine stereotactic body radiotherapy. Neuro-Oncology. 2013;15(10):1413–9.
Bilsky MH, et al. Single-stage posterolateral transpedicle approach for spondylectomy, epidural decompression, and circumferential fusion of spinal metastases. Spine (Phila Pa 1976). 2000;25(17):2240–9; discussion 250.
Pennington Z, et al. Minimally invasive versus conventional spine surgery for vertebral metastases: a systematic review of the evidence. Ann Transl Med. 2018;6(6):103.
Than KD, et al. Complication rates associated with open versus percutaneous pedicle screw instrumentation among patients undergoing minimally invasive interbody fusion for adult spinal deformity. Neurosurg Focus. 2017;43(6):E7.
Wang H, et al. Comparison of open versus percutaneous pedicle screw fixation using the sextant system in the treatment of traumatic thoracolumbar fractures. Clin Spine Surg. 2017;30(3):E239–e246.
Moussazadeh N, et al. Short-segment percutaneous pedicle screw fixation with cement augmentation for tumor-induced spinal instability. Spine J. 2015;15(7):1609–17.
Barzilai O, et al. Utility of cement augmentation via percutaneous fenestrated pedicle screws for stabilization of cancer-related spinal instability. Oper Neurosurg (Hagerstown). 2019;16(5):593–9.
Versteeg AL, et al. Complications after percutaneous pedicle screw fixation for the treatment of unstable spinal metastases. Ann Surg Oncol. 2016;23(7):2343–9.
Barzilai O, Bilsky MH, Laufer I. The role of minimal access surgery in the treatment of spinal metastatic tumors. Global Spine J. 2020;10(2 Suppl):79s–87s.
Dousset V, et al. Asymptomatic cervical haemangioma treated by percutaneous vertebroplasty. Neuroradiology. 1996;38:392–4.
Amar AP, et al. Percutaneous transpedicular polymethylmethacrylate vertebroplasty for the treatment of spinal compression fractures. Neurosurgery. 2001;49(5):1105–14; discussion 1114–5.
Berenson J, et al. Balloon kyphoplasty versus non-surgical fracture management for treatment of painful vertebral body compression fractures in patients with cancer: a multicentre, randomised controlled trial. Lancet Oncol. 2011;12(3):225–35.
Sorensen ST, et al. Vertebroplasty or kyphoplasty as palliative treatment for cancer-related vertebral compression fractures: a systematic review. Spine J. 2019;19(6):1067–75.
Lee MJ, et al. Percutaneous treatment of vertebral compression fractures: a meta-analysis of complications. Spine (Phila Pa 1976). 2009;34(11):1228–32.
Stangenberg M, et al. Cervical vertebroplasty for osteolytic metastases as a minimally invasive therapeutic option in oncological surgery: outcome in 14 cases. Neurosurg Focus. 2017;43(2):E3.
Lieberman IH, Togawa D, Kayanja MM. Vertebroplasty and kyphoplasty: filler materials. Spine J. 2005;5(6 Suppl):305S–16S.
Lieberman IH, et al. Initial outcome and efficacy of “kyphoplasty” in the treatment of painful osteoporotic vertebral compression fractures. Spine (Phila Pa 1976). 2001;26(14):1631–8.
Chang X, et al. Vertebroplasty versus kyphoplasty in osteoporotic vertebral compression fracture: a meta-analysis of prospective comparative studies. Int Orthop. 2015;39(3):491–500.
Dalton BE, et al. Radiofrequency-targeted vertebral augmentation versus traditional balloon kyphoplasty: radiographic and morphologic outcomes of an ex vivo biomechanical pilot study. Clin Interv Aging. 2012;7:525–31.
Krueger A, et al. Management of pulmonary cement embolism after percutaneous vertebroplasty and kyphoplasty: a systematic review of the literature. Eur Spine J. 2009;18(9):1257–65.
Wang LJ, et al. Pulmonary cement embolism associated with percutaneous vertebroplasty or kyphoplasty: a systematic review. Orthop Surg. 2012;4(3):182–9.
Gosev I, et al. Right ventricular perforation and pulmonary embolism with polymethylmethacrylate cement after percutaneous kyphoplasty. Circulation. 2013;127(11):1251–3.
Barzilai O, et al. Minimal access surgery for spinal metastases: prospective evaluation of a treatment algorithm using patient-reported outcomes. World Neurosurg. 2018;120:e889–901.
Tomasian A, et al. Percutaneous thermal ablation of spinal metastases: recent advances and review. AJR Am J Roentgenol. 2018;210(1):142–52.
Wallace AN, et al. Radiographic local control of spinal metastases with percutaneous radiofrequency ablation and vertebral augmentation. AJNR Am J Neuroradiol. 2016;37(4):759–65.
Singh S, Saha S. Electrical properties of bone. A review. Clin Orthop Relat Res. 1984;186:249–71.
Reyes M, et al. Multicenter clinical and imaging evaluation of targeted radiofrequency ablation (t-RFA) and cement augmentation of neoplastic vertebral lesions. J Neurointerv Surg. 2018;10(2):176–82.
Sloan AE, et al. Results of the NeuroBlate System first-in-humans Phase I clinical trial for recurrent glioblastoma: clinical article. J Neurosurg. 2013;118(6):1202–19.
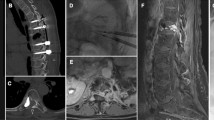
Tatsui CE, et al. Spinal laser interstitial thermal therapy: a novel alternative to surgery for metastatic epidural spinal cord compression. Neurosurgery. 2016;79(Suppl 1):S73–82.
Bastos DCA, et al. Spinal laser interstitial thermal therapy: single-center experience and outcomes in the first 120 cases. J Neurosurg Spine. 2020:1–10.
Yamada Y, et al. The impact of histology and delivered dose on local control of spinal metastases treated with stereotactic radiosurgery. Neurosurg Focus. 2017;42(1):E6.
Moulding HD, et al. Local disease control after decompressive surgery and adjuvant high-dose single-fraction radiosurgery for spine metastases. J Neurosurg Spine. 2010;13(1):87–93.
Yamada Y, et al. High-dose, single-fraction image-guided intensity-modulated radiotherapy for metastatic spinal lesions. Int J Radiat Oncol Biol Phys. 2008;71(2):484–90.
Tseng CL, et al. Spine stereotactic body radiotherapy: indications, outcomes, and points of caution. Global Spine J. 2017;7(2):179–97.
DeLaney TF, et al. Intraoperative dural irradiation by customized 192iridium and 90yttrium brachytherapy plaques. Int J Radiat Oncol Biol Phys. 2003;57(1):239–45.
Folkert MR, et al. Intraoperative 32P high-dose rate brachytherapy of the dura for recurrent primary and metastatic intracranial and spinal tumors. Neurosurgery. 2012;71(5):1003–10; discussion 1010–1.
Bludau F, et al. Phase I/II trial of combined kyphoplasty and intraoperative radiotherapy in spinal metastases. Spine J. 2018;18(5):776–81.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Wang, C.P., Brisco, A., Liu, J.K.C. (2022). Surgical Management of Metastatic Disease to the Spine. In: Leong, S.P., Nathanson, S.D., Zager, J.S. (eds) Cancer Metastasis Through the Lymphovascular System. Springer, Cham. https://doi.org/10.1007/978-3-030-93084-4_48
Download citation
DOI: https://doi.org/10.1007/978-3-030-93084-4_48
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-93083-7
Online ISBN: 978-3-030-93084-4
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)