Abstract
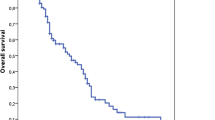
There is no evidence that prolonged pre diagnostic symptomatic intervals (PSI) increases the risk of death in pediatric brain tumors. When investigating the role of time previous research had not controlled for confounding variables or measured the pretreatment interval (PTI). We use the term global delay interval (GDI) to describe the sum of PSI and PTI. The aim of this research was to evaluate whether there was a decrease in the probability of survival in children with brain tumors due to a prolonged PSI, PTI and GDI, using a multivariate survival analysis. We retrospective review 127 clinical records labeled with the diagnosis of CNS tumors attended at a specialized pediatric center in Mexico City from January 2008 to December 2012. Patients with PSI and GDI diagnosed between 3 and 6 months showed statistical lower probability of surviving that those with intervals <3 months even when adjusting for age, sex, localization and tumor grade. When stratified for the place of residency and adjusted for sex, age, localization, grade of tumor, type of surgery and coadjuvant therapy, a GDI between 3 and 6 months showed to be a risk factor for the overall survival of brain tumors compared with an interval < 3 months. When analyzing the interaction, high grade tumors are at more risk of dying when GDI was between 3 and 6 months compared to <3 months. Prolonged PSI and GDI showed to be a potential prognostic factor for survival in CNS tumors, especially in high grade tumors. Future prospective research should measure the PSI, PTI and GDI and adjust for covariates in order to properly infer the effect of time in pediatric brain tumors.

Similar content being viewed by others
Abbreviations
- CNS:
-
Central Nervous System
- USA:
-
United States of America
- PSI:
-
Prediagnostic Symptomatic Intervals
- PTI:
-
Pretreatment Interval
- GDI:
-
Global Delay Interval
- GDP:
-
Gross Domestic Product
- HIMFG:
-
Hospital Infantil de México Federico Gómez
- IQR:
-
Interquartile Range
- CI:
-
Confidence Interval
- OS:
-
Overall Survival
- CNS ET/RF:
-
CNS Embryonal tumor with rhabdoid features
References
Wells EM, Packer RJ (2015) Pediatric brain tumors. Continuum 21:373–396
Siegel RL, Miller KD, Jemal A (2019) Cancer statistics, 2019. CA Cancer J Clin 69:7–34
Siegel RL, Miller KD, Jemal A (2016) Cancer statistics. CA Cancer J Clin 66:7–30
Wilne S, Collier J, Kennedy C, Koller K, Grundy R, Walker D (2007) Presentation of childhood CNS tumours: a systematic review and meta-analysis. Lancet Oncol 8:685–695
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68:394–424
Dang-Tan T, Franco EL (2007) Diagnosis delays in childhood cancer. Cancer. 110:703–713
Crawford JR, Santi MR, Vezina G, Myseros JS, Keating RF, LaFond DA et al (2007) CNS germ cell tumor (CNSGCT) of childhood: presentation and delayed diagnosis. Neurology. 68:1668–1673
Patel V, McNinch NL, Rush S (2019) Diagnostic delay and morbidity of central nervous system tumors in children and young adults: a pediatric hospital experience. J Neuro-Oncol 143:297–304
Shay V, Fattal-Valevski A, Beni-Adani L, Constantini S (2012) Diagnostic delay of pediatric brain tumors in Israel: a retrospective risk factor analysis. Childs Nerv Syst 28:93–100
Sethi RV, Marino R, Niemierko A, Tarbell NJ, Yock TI, MacDonald SM (2013) Delayed diagnosis in children with intracranial germ cell tumors. J Pediatr 163:1448–1453
Kukal K, Dobrovoljac M, Boltshauser E, Ammann RA, Grotzer MA (2009) Does diagnostic delay result in decreased survival in paediatric brain tumours? Eur J Pediatr 168:303–310
Flores LE, Williams DL, Bell BA, O’Brien M, Ragab AH (1986) Delay in the diagnosis of pediatric brain tumors. Am J Dis Child 140:684–686
Handayani K, Sitaresmi MN, Supriyadi E, Widjajanto PH, Susilawati D, Njuguna F, van de Ven PM, Kaspers GJL, Mostert S (2016) Delays in diagnosis and treatment of childhood cancer in Indonesia. Pediatr Blood Cancer 63:2189–2196
Dobrovoljac M, Hengartner H, Boltshauser E, Grotzer M (2002) Delay in the diagnosis of paediatric brain tumours. Eur J Pediatr 161:663–667
Molineus A, Boxberger N, Redlich A, Vorwerk P (2013) Time to diagnosis of brain tumors in children: a single-Centre experience. Pediatr Int 55:305–309
Azizi AA, Heßler K, Leiss U, Grylli C, Chocholous M, Peyrl A, Gojo J, Slavc I (2017) From symptom to diagnosis—the Prediagnostic symptomatic interval of pediatric central nervous system tumors in Austria. Pediatr Neurol 76:27–36
Mehta V, Chapman A, McNeely PD, Walling S, Howes WJ (2002) Latency between symptom onset and diagnosis of pediatric brain tumors: an eastern Canadian geographic study. Neurosurgery. 51:365–373
Stocco C, Pilotto C, Passone E, Nocerino A, Tosolini R, Pusiol A, Cogo P (2017) Presentation and symptom interval in children with central nervous system tumors. A single-center experience. Childs Nerv Syst 33:2109–2116
Wilne S, Collier J, Kennedy C, Jenkins A, Grout J, Mackie S, Koller K, Grundy R, Walker D (2012) Progression from first symptom to diagnosis in childhood brain tumours. Eur J Pediatr 171:87–93
Reulecke BC, Erker CG, Fiedler BJ, Niederstadt T-U, Kurlemann G (2008) Brain tumors in children: initial symptoms and their influence on the time span between symptom onset and diagnosis. J Child Neurol 23:178–183
Elhassan MMA, Mohamedani AA, Osman HHM, Yousif NO, Elhaj NM, Qaddoumi I (2019) Patterns, treatments, and outcomes of pediatric central nervous system tumors in Sudan: a single institution experience. Childs Nerv Syst 35:437–444
Fukuoka K, Yanagisawa T, Suzuki T, Shirahata M, Adachi J-I, Mishima K, Fujimaki T, Matsutani M, Nishikawa R (2014) Duration between onset and diagnosis in central nervous system tumors: impact on prognosis and functional outcome. Pediatr Int 56:829–833
Walker D, Wilne S, Grundy R, Kennedy C, Neil DA et al (2016) A new clinical guideline from the Royal College of Paediatrics and Child Health with a national awareness campaign accelerates brain tumor diagnosis in UK children - “headSmart: Be Brain Tumour Aware”. Neuro-Oncology 18:445–454
Abdelmabood S, Kandil S, Megahed A, Fouda A (2017) Delays in diagnosis and treatment among children with cancer: Egyptian perspective. East Mediterr Health J 23:422–429
Njuguna F, Martijn H, Langat S, Musimbi J, Muliro H, Skiles J, Vik T, Sitaresmi MN, van de Ven PM, Kaspers GJL, Mostert S (2016) Factors influencing time to diagnosis and treatment among pediatric oncology patients in Kenya. Pediatr Hematol Oncol 33:186–199
INEGI. Encuesta Intercensal 2015. In: Instituto Nacional de Estadística y Geografía [Internet]. 14 Mar 2015 [cited 28 Jan 2020]. Available: https://www.inegi.org.mx/programas/intercensal/2015/
CONAPO. 31.4 por ciento de la población en México son niñas, niños y adolescentes, de 0 a 17 años. In: Consejo Nacional de Población [Internet]. 30 April, 2019 [cited 28 Jan 2020]. Available: https://www.gob.mx/conapo/prensa/31-4-por-ciento-de-la-poblacion-en-mexico-son-ninas-ninos-y-adolescentes-de-0-a-17-anos-198293?idiom=es
INEGI. Por actividad económica. In: Instituto Nacional de Estadística y Geografía [Internet]. 2018 [cited 28 Jan 2020]. Available: https://www.inegi.org.mx/temas/pib/
CONEVAL. Medición de Pobreza 2008-2018, Estados Unidos Mexicanos. In: Consejo Nacional de Evaluación de la Política de Desarrollo Social [Internet]. 2018 [cited 28 Jan 2020]. Available: https://www.coneval.org.mx/Medicion/PublishingImages/Pobreza_2018/Serie_2008-2018.jpg
Santos-Preciado JI (2008) El Hospital Infantil de México y su Boletín Médico: un hito en la historia de la pediatría mexicana. Bol Med Hosp Infant Mex 65:81–82
de León Castro-Sierra Eduardo FC-P, Perez Peña-Diazconti M et al (2006) Bol Med Hosp Infant Mex 63:367–381
Ostrom QT, Gittleman H, Truitt G, Boscia A, Kruchko C, Barnholtz-Sloan JS (2018) CBTRUS Statistical Report: Primary Brain and Other Central Nervous System Tumors Diagnosed in the United States in 2011–2015. Neuro Oncol 20:iv1–iv86
Rivas-Vilela S, Rubió-Casadevall J, Fàbrega-Ribas A, Joly-Torta C, Vilardell L, Marcos-Gragera R (2019) Incidence and survival of central nervous system tumors in childhood and adolescence in Girona (Spain) 1990–2013: national and international comparisons. Clin Transl Oncol 21:1177–1185. https://doi.org/10.1007/s12094-019-02043-9
Desandes E, Guissou S, Chastagner P, Lacour B (2014) Incidence and survival of children with central nervous system primitive tumors in the French National Registry of childhood solid tumors. Neuro-Oncology 16:975–983
Farinotti M, Ferrarini M, Solari A, Filippini G (1998) Incidence and survival of childhood CNS tumours in the region of Lombardy. Italy Brain 121(Pt 8):1429–1436
Magnani C, Aareleid T, Viscomi S, Pastore G, Berrino F, Oberaigner W et al (2001) Variation in survival of children with central nervous system (CNS) malignancies diagnosed in Europe between 1978 and 1992: the EUROCARE study. Eur J Cancer 37:711–721
Robertson PL, Zeltzer PM, Boyett JM, Rorke LB, Allen JC, Geyer JR, Stanley P, Li H, Albright AL, McGuire-Cullen P, Finlay JL, Stevens KR, Milstein JM, Packer RJ, Wisoff J, _ _ Survival and prognostic factors following radiation therapy and chemotherapy for ependymomas in children: a report of the Children’s Cancer group. J Neurosurg 1998;88: 695–703
de Araujo OL, da Trindade KM, Trompieri NM, Fontenele JB, Felix FHC (2011) Analysis of survival and prognostic factors of pediatric patients with brain tumor. J Pediatr 87:425–432
María GVM, Francis ERN, Nelson UL, Gutiérrez E, Gimón AV, Barboza D et al (2013) Tumores cerebrales pediátricos experiencia de 10 años. Revista Venezolana de Oncologia 25:85–97
Zareifar S, Rowshani F, Haghpanah S, Bordbar M (2018) Five- year survival rate of children with central nervous system tumors in shiraz, Iran. Iranian Journal of Pediatric Hematology and Oncology 8:1–11
Mehrvar A, Faranoush M, Hedayati Asl AA, Tashvighi M, Fazeli MA, Qaddoumi I, Mehrvar N, Sobuti B, Jafarpour A, Ravan parsa R, Zangooei R, Alebouyeh M, Vossough P (2014) Childhood central nervous system tumors at MAHAK’s pediatric Cancer treatment and research center (MPCTRC), Tehran. Iran Childs Nerv Syst 30:491–496
KA R (2011, 810) Epidemiology and survival of childhood primary central nervous system malignancies in Iran: Results from a single center. Pediatr Blood Cancer 57
Grob ST, Levy JMM (2017) Improving diagnostic and therapeutic outcomes in pediatric brain tumors. Mol Diagn Ther 22:25–39. https://doi.org/10.1007/s40291-017-0299-3
Pogorzala M, Styczynski J, Wysocki M (2014) Survival and prognostic factors in children with brain tumors: long-term follow-up single center study in Poland. Anticancer Res 34:323–326
Segal D, Karajannis MA (2016) Pediatric brain tumors: an update. Curr Probl Pediatr Adolesc Health Care 46:242–250
Rey-Casserly C, Diver T (2019) Late effects of pediatric brain tumors. Curr Opin Pediatr 31:789–796
Chen J, Mullen CA (2017) Patterns of diagnosis and misdiagnosis in pediatric Cancer and relationship to survival. J Pediatr Hematol Oncol 39:e110–e115
Qaddoumi I, Merchant TE, Boop FA, Gajjar A (2019) Diagnostic delay in children with central nervous system tumors and the need to improve education. J Neuro-Oncol 145:591–592
Ferrari A, Lo Vullo S, Giardiello D, Veneroni L, Magni C, Clerici CA, Chiaravalli S, Casanova M, Luksch R, Terenziani M, Spreafico F, Meazza C, Catania S, Schiavello E, Biassoni V, Podda M, Bergamaschi L, Puma N, Massimino M, Mariani L (2016) The sooner the better? How symptom interval correlates with outcome in children and adolescents with solid tumors: regression tree analysis of the findings of a prospective study. Pediatr Blood Cancer 63:479–485
Gerber NU, von Hoff K, von Bueren AO, Treulieb W, Deinlein F, Benesch M, Zwiener I, Soerensen N, Warmuth-Metz M, Pietsch T, Mittler U, Kuehl J, Kortmann RD, Grotzer MA, Rutkowski S (2012) A long duration of the prediagnostic symptomatic interval is not associated with an unfavourable prognosis in childhood medulloblastoma. Eur J Cancer 48:2028–2036
Acknowledgements
We are thankful to our patients and their families for the support to carry out this research. To the team of the Pediatric Neurology Department of HIMFG and their continuous search for excellence, kindness and integrity.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
There is no financial interest or benefit to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 28 kb)
Rights and permissions
About this article
Cite this article
Barragán-Pérez, E.J., Altamirano-Vergara, C.E., Alvarez-Amado, D.E. et al. The Role of Time as a Prognostic Factor in Pediatric Brain Tumors: a Multivariate Survival Analysis. Pathol. Oncol. Res. 26, 2693–2701 (2020). https://doi.org/10.1007/s12253-020-00875-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12253-020-00875-3