Abstract
Purpose
The aim was to evaluate the total diagnostic interval (TDI) and presenting complaints in children with brain tumours in Serbia.
Methods
This study retrospectively analysed 212 children aged 0–18 years newly diagnosed with brain tumours in two tertiary centres from mid-March 2015 to mid-March 2020 covering virtually all children with brain tumours in Serbia. TDI was calculated as the difference between the date of diagnosis and the date of symptom onset presented as a median in weeks. This variable has been evaluable for 184 patients.
Results
Overall TDI was 6 weeks. TDI was significantly longer in patients with low-grade tumours (11 weeks) than in patients with high-grade tumours (4 weeks). Children with the most frequent complaints (headache, nausea/vomiting and gait disturbance) were more likely to be diagnosed sooner. Patients with a single complaint had significantly longer TDI (12.5 weeks) contrasted to patients with multiple complaints (5 weeks).
Conclusion
TDI with a median of 6 weeks is similar to other developed countries. Our study supports the view that low-grade tumours will present later than high-grade tumours. Children with the commonest complaints and children with multiple complaints were more likely to be diagnosed sooner.
Similar content being viewed by others
Introduction
Brain tumours are considered the second most common malignancy of childhood [1]. It is generally believed that timely diagnosis might improve the outcome of malignant disease. As the significance of diagnostic delay for survivorship from paediatric cancers is unclear, the term total diagnostic interval (TDI) is now preferred [2, 3]. However, in children with brain tumours, longer TDI might confer a greater risk for the development of neurological sequelae [4,5,6,7]. Multiple factors have been identified to impact TDI, the most prominent being age at diagnosis, parent level of education, type of cancer and presenting symptoms [8]. Therefore, TDI in children with brain tumours varies widely. Additionally, presenting complaints are usually polymorphous and nonspecific [9]. TDI also reflects, to a certain extent, the efficacy of the health care service in terms of the referral of potential patients to tertiary care [10].
TDI in children with brain tumours has been studied around the world, mostly through single-institution investigations in high-income countries [11,12,13,14,15,16,17,18]. So far, it has never been thoroughly explored in any of the Balkan countries which share a similar socio-economic milieu [19]. Children with brain tumours in Serbia treated at National Cancer Research Centre were studied predominantly regarding management and its outcome so far, never to describe the diagnostic path of these patients [20,21,22].
Therefore, this study aimed to evaluate TDI and presenting complaints in children with brain tumours in Serbia for the first time to potentially identify factors eligible for improvement.
Methods
This study retrospectively analysed all children aged 0–18 years in two tertiary centres in Serbia, namely Neurosurgery Clinic, University Clinical Centre of Serbia (Klinika za neurohirurgiju Univerzitetskog kliničkog centra Srbije) and National Cancer Research Centre (Institut za onkologiju i radiologiju Srbije) newly diagnosed with brain tumours from mid-March 2015 to mid-March 2020 (until the beginning of the COVID-19 pandemic) covering virtually all children with brain tumours in Serbia.
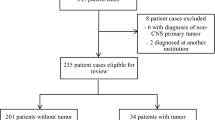
After reviewing patient registers in both institutions, 212 patients were eligible for analysis.
Collected data included age at diagnosis, sex, place of living, parent level of education, tumour type, tumour grade, tumour location, presenting symptoms, date of symptom onset and date of diagnosis.
Place of living was used to evaluate differences between country regions and urban and rural areas.
TDI representing the study outcome measure was calculated as the difference between the date of diagnosis (date of surgery for children who underwent it or date of first MRI indicating tumour presence in inoperable patients with diffuse intrinsic pontine gliomas and optic pathway gliomas) and the date of symptom onset presented in weeks. This variable has been evaluable for 184 patients.
Patients were subclassified into three groups according to their age at diagnosis.
Following descriptive statistics, analysis of TDI according to age, tumour type, tumour grade, tumour location, country region, urbanity, parental education and individual symptoms was performed using the double-sided Mann–Whitney U test and Kruskal–Wallis test. Additionally, the distribution of individual symptoms between different age groups and tumour locations was examined using the chi-square quadrant test or Fisher’s exact test as appropriate. A P-value of < 0.05 was considered statistically significant. Numbers missing for each analysis were reported. Described was conducted using the software package EZR (Saitama Medical Centre, Jichi Medical University, Japan) [23].
Numeric results are presented as median with interquartile range.
The study was conducted according to both institutional ethical policies. Written informed consent was obtained from parents/guardians of National Cancer Research Centre participants before the beginning of medical treatment where they agreed to the free use of data for research purposes as long as their identities were not made publicly available. The expert collegiate of Neurosurgery Clinic, University Clinical Centre of Serbia approved the collection of aforementioned data from medical records and publication has been granted by the Ethics Committee of the University Clinical Centre of Serbia (Ref. No. 17/22).
Results
This study included 212 children diagnosed with brain tumours from mid-March 2015 to mid-March 2020 including 7 patients with neurofibromatosis type 1 and 1 patient with neurofibromatosis type 2. The number of patients for each consecutive year was 45, 39, 36, 34, 51 and 7. Patient characteristics are reported in Table 1.
TDI was evaluated in 184/212 patients (69/95 patients from Neurosurgery Clinic, University Clinical Centre of Serbia and 115/117 from National Cancer Research Centre). Overall TDI was 6 (3, 14.25) weeks. TDI in a subgroup of patients with neurofibromatosis (evaluated in 6/8 patients) was 22 (14, 45.75) weeks being significantly longer than in 178/204 patients without neurocutaneous syndromes (6 (3, 14) weeks).
TDI was estimated for different age groups being 5 (4, 13) weeks in those aged 0–5 years, 6 (4, 12.75) weeks in children aged 6–11 years and 7 (3, 26) weeks in the group aged 12–18 years (Fig. 1a). Even though PSI did not statistically differ between age groups, age showed a weak positive correlation with PSI (Spearman’s correlation r = 0.158, P = 0.0319).
TDI was evaluated for different tumour locations and it was the longest for supratentorial tumours (8 (4, 19.5) weeks), followed by spinal cord tumours, midline tumours, infratentorial tumours and brainstem tumours being 7 (3, 10.5), 7 (4, 24), 5 (3, 10) and 5 (2, 12) weeks, respectively (Fig. 1b).
TDI according to tumour type is presented in Fig. 1c.
In patients with low-grade tumours (11 (4, 37) weeks), TDI was significantly longer than in patients with high-grade tumours (4 (3, 8) weeks). In patients who were not graded, TDI was 5 (2, 12) weeks (Fig. 1d).
TDI was evaluated in 176 patients according to their place of living. TDI was the same in urban (6 (4, 16) weeks) and rural populations (6 (3, 13.5)) weeks). TDI did not statistically differ either for different country regions being 5 (3, 14) weeks for the capital Belgrade, 5 (4, 8) weeks for the Autonomous Province of Vojvodina and 7 (4, 16.5) weeks for Central Serbia.
TDI did not statistically differ between different maximal parent education levels (estimated in 99 patients), but it was shorter the more educated parents were. In children whose parents graduated from elementary school, the median TDI was 8 (4, 13.25) weeks, and from secondary school 5 (4, 10) weeks, and in those with higher education, it was 4 (3, 8) weeks.
The most frequent complaints in 186 evaluated patients were nausea/vomiting, headache, gait disturbance, visual disturbance, motor deficit, seizure, altered mental status and endocrine disorders. Other complaints included back pain, speech disturbance, loss of sphincter control, vertigo, macrocrania, bulging fontanelle, torticollis and loss of milestones. TDI in patients with particular complaints and the absolute frequency distribution of particular complaints are presented in Table 2.
Patients with a single complaint (51/186) had significantly longer TDI (12.5 (4, 44.25) weeks) contrasted to patients with multiple complaints (5 (3, 11.75) weeks) (P = 0.005). The most frequent single complaints were visual disturbance (16/51), seizures (10/51) and headache (7/51). In 66/186 patients, headache and nausea/vomiting were simultaneously present representing the most common combination of complaints.
The distribution of complaints amongst different age groups is shown in Fig. 2. Statistical significance was noted for headaches being commonest in the oldest children, gait disturbance mostly noted in the youngest group and seizures being least frequently observed in the middle age group.
The distribution of complaints between different tumour locations is presented in Fig. 3. The distribution is significantly different for all symptoms but for altered mental status and endocrine disorders. Nausea/vomiting, headache and gait disturbance were most common in infratentorial tumours. The visual disturbance was most frequent in midline tumours. Seizures were the commonest in supratentorial tumours. Endocrine disorders were exclusive to midline tumours.
Discussion
The estimated annual age-standardised incidence of brain tumours in European children aged 0–14 years was 29.9 per million person-years. In adolescents aged 15–19, it was 15.0 per million person-years [24].
The number of patients (n = 212) in our analysis in 5 years correlates with general European incidence. It also supports previously published data considering the incidence of paediatric brain tumours in Serbia as well as sex distribution showing slight male predominance [25, 26].
This was the first study to focus on total diagnostic interval and presenting complaints in children with brain tumours in Serbia. The main objective was to estimate time lost from the onset of symptoms until definitive diagnosis (total diagnostic interval). In 184 out of 212 patients, the median total diagnostic interval was 6 weeks. The interval from the onset of complaints until reaching the final diagnosis varies highly amongst countries and our results are comparable to the findings of other studies. In single-centre examples, the median total diagnostic interval in Germany was 13.5 weeks [11], in Austria 8.5 weeks [12], in Japan and the USA 6 weeks [13,14,15] and in Italy 4 weeks [16]. Nationwide studies showed a median total diagnostic interval of 8.3 weeks in Sweden and 4 weeks in Qatar [17, 18]. This has been summarised in Table 3.
Differences in TDI might be explained by variable organisation of the health care system and physicians’ awareness of how often brain tumours in children present with non-specific complaints. In primary care in Serbia, all children have free access to their chosen paediatrician instead of a general practitioner which might explain shorter TDI than in some other high-income countries [27].
Studies investigating TDI in children with brain tumours in developed countries often exclude patients with tumour predisposition syndromes, like neurofibromatosis, since diagnosis is made through regular imaging without any presenting symptoms. Therefore, when reported, TDI in patients with tumour predisposition syndromes is significantly shorter compared to patients without them [13, 28]. However, longer TDI in patients with neurofibromatosis (22 weeks) contrasted to other patients (6 weeks) in our study suggests that wariness of tumour risk in these patients is not high amongst practitioners requiring further education towards raising awareness of the topic. Furthermore, this implies that better identification and surveillance of tumour predisposition syndromes is needed.
TDI between different age groups showed a gradual increase across ages being 5 weeks in the youngest (0–5 years), 6 weeks in the medium (6–11 years) and 7 weeks in the oldest group (12–18 years). A shorter TDI in younger children was reported in previous research [10, 12, 29].
Tumour location seemed not to impact TDI having a median from 5 to 8 weeks in different locations. No significant difference between different tumour types and TDI medians ranging from 3 to 11.5 weeks has been noticed. However, TDI in craniopharyngioma stood out with a median TDI of 28 weeks. This finding is supported by previous studies and might be explained by slowly developing symptoms, predominantly visual disturbance [10, 14].
Significantly longer TDI was observed in low-grade tumours compared to high-grade tumours (11- vs 4-week median). This finding, reflecting tumour biology, has been observed previously [10, 17, 18, 28]. TDI in patients who were not graded was 5 weeks. It might be explained by the fact that this group in our study mostly encompasses diffuse intrinsic pontine gliomas exhibiting high-grade behaviour.
Similar median TDI between different country regions and urban and rural areas might be explained by universal access to primary health care and is not uncommon in other countries as well [30]. Observed TDI seemed to be shorter in children with more educated parents despite the lack of statistical significance (4 weeks in most educated parents, 8 weeks in the least educated ones) supporting the previous reports [31].
Systemic review analysing presenting complaints showed that the most frequent of them were headache, nausea/vomiting and gait disturbance [9]. The distribution of symptoms in our study supports that finding. Children with these complaints had a shorter total diagnostic interval (5-week median) compared to children without them (median ranging from 7 to 8 weeks) supporting the previous studies [17]. Additionally, a survival study of paediatric patients with brain tumours in Serbia conducted between 2007 and 2016 reported symptoms of increased intracranial pressure as the most common complaint [22].
On the other hand, the most frequent single complaints were visual disturbance and seizures which were more likely to display longer total diagnostic intervals (8 and 13 weeks respectively) attributable to treatment of other more common causes of these complaints in the paediatric population. Such a phenomenon has been already described [18]; however, there is data supporting the opposite view considering seizures [12]. Additionally, the oldest group of children were more likely to have a headache as a complaint compared to younger groups. In the youngest patients, on the other hand, gait disturbance has been observed twice as frequently as in the other two groups. These findings were also recorded in previous studies [9, 29] and might be additionally explained by the predilection of tumours in certain locations for different age groups.
Presenting complaints significantly varied between locations reflecting their biology. Nausea/vomiting, headache and gait disturbance were most common in infratentorial tumours. The visual disturbance was most frequent in midline tumours. Seizures were the commonest in supratentorial tumours. Endocrine disorders in our study were exclusively observed in midline tumours. Other research supports these findings [9, 28, 32].
TDI depends on patient/parent interval and healthcare system interval [3]. The major limitation of this study was the inability to differentiate between parental and system intervals/delays due to insufficient data in our retrospective study and it is a potential area to be addressed in the future. However, it has been shown that people of Serbian ancestry who emigrated to Austria displayed 6 weeks of TDI, the same as in our study, suggesting potentially similar patient and system intervals [12].
To decrease bias, all paediatric patients treated for central nervous system tumours were initially included; however, TDI was evaluable in 184 out of 212 patients due to some missing data. This study better represents children with more aggressive tumours since 98% of patients from the National Cancer Research Centre were with evaluable TDI, where a total of 5 physicians (paediatricians and radiation oncologists) create medical records, contrasted to 73% of patients from Neurosurgery Clinic, University Clinical Centre of Serbia, where 11 surgeons are in charge of the medical documentation. It might be explained by the interpersonal differences between doctors who create medical documentation for not adequately describing the diagnostic path with bigger heterogeneity at the Neurosurgery Clinic, University Clinical Centre of Serbia, due to a greater number of employees and their different medical specialties. Although the limitation of this study is the retrospective design, the mentioned might be overcome by a future prospective study. However, we present for the first time the national experience by including results from both tertiary centres treating children with central nervous system tumours.
According to Serbian medical chamber data, around 1200 paediatricians work in primary care meaning that every 30th will encounter a child with a brain tumour each year, leaving some without the opportunity to encounter such a patient during their whole working career [33]. A most recent Swedish study provided evidence that patient interval does not vary amongst different tumour types/locations, suggesting that most interventions should be directed towards medical professionals [17]. Special campaigns and guidelines for physicians are created worldwide to raise awareness of paediatric tumours [10, 34]. The World Health Organization declared low-grade gliomas as one of the goal tumours to be diagnosed and treated early in the Global Initiative for Childhood Cancer [35]. Additionally, in the 2020 Lancet Commission considering cost-effective interventions for improving care for children with cancer, it has been suggested that most low- and middle-income countries should establish comprehensive national paediatric cancer registers by 2030 [36]. Our data might contribute to designing such guidelines for Serbia and encourage better surveillance of paediatric brain tumours.
This is the first study investigating presenting complaints and the total diagnostic interval in paediatric patients with brain tumours in Serbia. The total diagnostic interval with a median of 6 weeks is similar to other developed countries. Our study supports the view that low-grade tumours will present later than high-grade tumours. Children with the commonest complaints (headache, nausea/vomiting and gait disturbance) were more likely to be diagnosed sooner, as well as children with multiple complaints. Based on our study, the development of guidelines for referral intended for paediatricians in Serbia in primary health care might shorten the total diagnostic interval amongst children with brain tumours.
Availability of data and materials
All data generated or analysed during this study are included in this published article and its supplementary information files (S1 Appendix—Minimal dataset).
References
Udaka YT, Packer RJ (2018) Pediatric brain tumors. In: Neurologic clinics (Vol. 36, Issue 3,), WB Saunders, pp 533–556. https://doi.org/10.1016/j.ncl.2018.04.009
Barr RD (2014) “Delays” in diagnosis: a misleading concept, yet providing opportunities for advancing clinical care. J Pediatr Hematol Oncol 36(3):169–172. https://doi.org/10.1097/MPH.0000000000000108
Weller D, Vedsted P, Rubin G, Walter FM, Emery J, Scott S, Campbell C, Andersen RS, Hamilton W, Olesen F, Rose P, Nafees S, van Rijswijk E, Hiom S, Muth C, Beyer M, Neal RD (2012) The Aarhus statement: improving design and reporting of studies on early cancer diagnosis. Br J Cancer 106(7):1262. https://doi.org/10.1038/BJC.2012.68
Pilotto C, Liguoro I, Scaravetti S, Passone E, D’Agostini S, Tuniz F, Skrap M, Cogo P (2021) Risk factors of persistent hydrocephalus in children with brain tumor: a retrospective analysis. Pediatr Neurosurg 56(3):205–212. https://doi.org/10.1159/000513732
Tsai ML, Chen CL, Hsieh KLC, Miser JS, Chang H, Liu YL, Wong TT (2018) Seizure characteristics are related to tumor pathology in children with brain tumors. Epilepsy Res 147:15–21. https://doi.org/10.1016/J.EPLEPSYRES.2018.08.007
Pietilä S, Lenko HL, Oja S, Koivisto AM, Pietilä T, Mäkipernaa A (2016) Electroretinography and visual evoked potentials in childhood brain tumor survivors. J Child Neurol 31(8):998–1004. https://doi.org/10.1177/0883073816634863
Malbari F, Gill J, Daigle A, Rodriguez LL, Raghubar KP, Davis KC, Scheurer M, Ma MM, Kralik SF, Meoded A, Okcu MF, Chintagumpala MM, Aldave G, Weiner HL, Kahalley LS (2022) Cerebellar mutism syndrome in pediatric neuro-oncology: a multidisciplinary perspective and call for research priorities. Pediatr Neurol 132:4–10. https://doi.org/10.1016/J.PEDIATRNEUROL.2022.04.014
Dang-Tan T, Franco EL (2007) Diagnosis delays in childhood cancer: a review. Cancer 110(4):703–713. https://doi.org/10.1002/cncr.22849
Wilne S, Collier J, Kennedy C, Koller K, Grundy R, Walker D (2007) Presentation of childhood CNS tumours: a systematic review and meta-analysis. Lancet Oncol 8(8):685–695. https://doi.org/10.1016/S1470-2045(07)70207-3
Shanmugavadivel D, Liu JF, Murphy L, Wilne S, Walker D (2020) Accelerating diagnosis for childhood brain tumours: an analysis of the HeadSmart UK population data. Arch Dis Child 105(4):355–362. https://doi.org/10.1136/archdischild-2018-315962
Molineus A, Boxberger N, Redlich A, Vorwerk P (2013) Time to diagnosis of brain tumors in children: a single-centre experience. Pediatr Int 55(3):305–309. https://doi.org/10.1111/ped.12095
Azizi AA, Heßler K, Leiss U, Grylli C, Chocholous M, Peyrl A, Gojo J, Slavc I (2017) From symptom to diagnosis—the prediagnostic symptomatic interval of pediatric central nervous system tumors in Austria. Pediatr Neurol 76:27–36. https://doi.org/10.1016/j.pediatrneurol.2017.08.006
Patel V, McNinch NL, Rush S (2019) Diagnostic delay and morbidity of central nervous system tumors in children and young adults: a pediatric hospital experience. J Neurooncol 143:297–304. https://doi.org/10.1007/s11060-019-03160-9
Fukuoka K, Yanagisawa T, Suzuki T, Shirahata M, Adachi JI, Mishima K, Fujimaki T, Matsutani M, Nishikawa R (2014) Duration between onset and diagnosis in central nervous system tumors: impact on prognosis and functional outcome. Pediatr Int 56(6):829–833. https://doi.org/10.1111/ped.12369
Coven SL, Stanek JR, Hollingsworth E, Finlay JL (2018) Delays in diagnosis for children with newly diagnosed central nervous system tumors. Neuro-Oncol Pract 5(4):227. https://doi.org/10.1093/NOP/NPY002
Stocco C, Pilotto C, Passone E, Nocerino A, Tosolini R, Pusiol A, Cogo P (2017) Presentation and symptom interval in children with central nervous system tumors. A single-center experience Child’s Nervous System 33(12):2109–2116. https://doi.org/10.1007/s00381-017-3572-1
Rask O, Nilsson F, Lähteenmäki P, Ehrstedt C, Holm S, Sandström P, Nyman P, Sabel M, Grillner P (2022) Prospective registration of symptoms and times to diagnosis in children and adolescents with central nervous system tumors: a study of the Swedish Childhood Cancer Registry. Pediatr Blood Cancer 69(11):e29850. https://doi.org/10.1002/PBC.29850
Maaz AUR, Yousif T, Saleh A, Pople I, Al-Kharazi K, Al-Rayahi J, Elkum N, Malik M (2021) Presenting symptoms and time to diagnosis for pediatric central nervous system tumors in Qatar: a report from Pediatric Neuro-Oncology Service in Qatar. Child’s Nerv Syst 37(2):465–474. https://doi.org/10.1007/s00381-020-04815-z
Petrovic M (2008) The role of geography and history in determining the slower progress of post-communist transition in the Balkans. Communis Post-Commun 41(2):123–145. https://doi.org/10.1016/j.postcomstud.2008.03.008
Kanda Y (2013) Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant 48:452–458. https://doi.org/10.1038/bmt.2012.244
Bokun J, Grujicic D, Skender-Gazibara M, Paripovic L, Pekmezovic T, Kisic-Tepavcevic D, Ilic V, Raicevic S, Stanic D, Miskovic I, Saric M, Nikitovic M (2018) Management and treatment of children with medulloblastoma in Serbia, a middle-income country. JBUON 23(4):1156–1162
Stanić D, Grujičić D, Pekmezović T, Bokun J, Popović-Vuković M, Janić D, Paripović L, Ilić V, Slović MP, Ilić R, Raičević S, Sarić M, Mišković I, Nidžović B, Nikitović M (2021) Clinical profile, treatment and outcome of pediatric brain tumors in Serbia in a 10-year period: a national referral institution experience. PLoS One 16(10):e0259095. https://doi.org/10.1371/journal.pone.0259095
Nikitović M, Stanić D, Pekmezović T, Gazibara MS, Bokun J, Paripović L, Grujičić D, Sarić M, Mišković I (2016) Pediatric glioblastoma: a single institution experience. Child’s Nerv Syst 32(1):97–103. https://doi.org/10.1007/S00381-015-2945-6
Fidler MM, Colombet M, Piñeros M, Soerjomataram I, Bray F, National F, Steliarova-Foucher E, Fidler MM, Colombet M, Lacour B, Kaatsch P, Piñeros M, Soerjomataram I, Bray F, Willem Coebergh J (2018) Changing geographical patterns and trends in cancer incidence in children and adolescents in Europe, 1991–2010 (Automated Childhood Cancer Information System): a population-based study. Lancet Oncol 19:1159–1169. https://doi.org/10.1016/S1470-2045(18)30423-6
Karalexi MA, Dessypris N, Georgakis MK, Ryzhov A, Jakab Z, Zborovskaya A, Dimitrova N, Zivkovic S, Trojanowski M, Sekerija M, Antunes L, Zagar T, Eser S, Bastos J, Demetriou A, Agius D, Coza D, Gheorghiu R, Kantzanou M, Petridou ET (2020) Birth seasonality of childhood central nervous system tumors: analysis of primary data from 16 Southern-Eastern European population-based registries. Int J Cancer 147(5):1252–1263. https://doi.org/10.1002/ijc.32875
Georgakis MK, Papathoma P, Ryzhov A, Zivkovic-Perisic S, Eser S, Taraszkiewicz Ł, Sekerija M, Žagar T, Antunes L, Zborovskaya A, Bastos J, Florea M, Coza D, Demetriou A, Agius D, Strahinja RM, Themistocleous M, Tolia M, Tzanis S, Petridou ET (2017) Malignant central nervous system tumors among adolescents and young adults (15–39 years old) in 14 Southern-Eastern European registries and the US Surveillance, Epidemiology, and End Results program: mortality and survival patterns. Cancer 123(22):4458–4471. https://doi.org/10.1002/cncr.30884
Bogdanović R, Lozanović D, Pejović Milovančević M, Sokal Jovanović L (2016) The child health care system of Serbia. J Pediatr 177:S156–S172. https://doi.org/10.1016/j.jpeds.2016.04.053
Reulecke BC, Erker CG, Fiedler BJ, Niederstadt TU, Kurlemann G (2008) Brain tumors in children: initial symptoms and their influence on the time span between symptom onset and diagnosis. J Child Neurol 23(2):178–183. https://doi.org/10.1177/0883073807308692
Dobrovoljac M, Hengartner H, Boltshauser E, Grotzer MA (2002) Delay in the diagnosis of paediatric brain tumours. Eur J Pediatr 161(12):663–667. https://doi.org/10.1007/s00431-002-1088-4
Boutahar FZ, Benmiloud S, el Kababri M, Kili A, el Khorassani M, Allali N, Khattab M, Qaddoumi I, Hessissen L (2018) Time to diagnosis of pediatric brain tumors: a report from the Pediatric Hematology and Oncology Center in Rabat. Morocco Child’s Nerv Syst 34(12):2431. https://doi.org/10.1007/S00381-018-3927-2
Fajardo-Gutiérrez A, Sandoval-Mex AM, Mejía-Aranguré JM, Rendón-Macías ME, Martínez-García MDC (2002) Clinical and social factors that affect the time to diagnosis of Mexican children with cancer. Med Pediatr Oncol 39(1):25–31. https://doi.org/10.1002/MPO.10100
Løhmann DJA, Sørensen P, Jørgensen J, Rosthøj S (2014) Most central nervous system tumours in children are diagnosed with little delay after admission. Danish Med J 61(8):A4886. https://pubmed.ncbi.nlm.nih.gov/25162445/
Radosavljevic T (2013) Demograski trendovi i kadrovski potencijal Srbije. Lekarska komora Srbije. https://www.rlkbg.org.rs/images/docs/demografskitrendovi.pdf. Accessed 16 Jul 2022
Wilne S, Koller K, Collier J, Kennedy C, Grundy R, Walker D (2010) The diagnosis of brain tumours in children: a guideline to assist healthcare professionals in the assessment of children who may have a brain tumour. Arch Dis Child 95(7):534–539. https://doi.org/10.1136/adc.2009.162057
Global initiative for childhood cancer (2020) World Health Organisation. https://www.who.int/publications/m/item/global-initiative-for-childhood-cancer. Accessed 31 Aug 2022
Jude S, Denburg A, Gupta S, Bouffet E, Sung L, Atun R, Bhakta N, Denburg A, Lindsay Frazier A, Friedrich P, Gupta S, Lam CG, Ward ZJ, Yeh JM, Allemani C, Coleman MP, di Carlo V, Loucaides E, Fitchett E, Rodriguez-Galindo C (2020) The Lancet Oncology Commission sustainable care for children with cancer: a Lancet Oncology Commission. Lancet Oncol 21(4):e185–e224. https://doi.org/10.1016/S1470-2045(20)30022-X
Acknowledgements
The authors would like to thank the nurses, doctors and staff of the National Cancer Research Centre, Belgrade, and the Neurosurgery Clinic, University Clinical Centre of Serbia, Belgrade, for their dedicated care of paediatric patients on daily basis.
Author information
Authors and Affiliations
Contributions
AJ, RI, DJ and VI wrote the original draft of the manuscript and conducted further editing. Responsible for the conceptualization of the research are AJ, RI, DJ, DG and VI. The core methodology was created by DJ and VI. All authors provided patient data and validated results. AJ performed the formal statistical analysis and prepared figures and tables. MPS, LP, MN, DJ, DG and VI supervised the research. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki and to both institutional ethical policies. Written informed consent was obtained from parents/guardians of National Cancer Research Centre participants before the beginning of medical treatment where they agreed to the free use of data for research purposes as long as their identities were not made publicly available. The expert collegiate of Neurosurgery Clinic, University Clinical Centre of Serbia, approved the collection of aforementioned data from medical records and publication has been granted by the Ethics Committee of the University Clinical Centre of Serbia (Ref. No. 17/22).
All data generated or analysed during this study are included in this published article (and its supplementary information files).
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jovanović, A., Ilić, R., Pudrlja Slović, M. et al. Total diagnostic interval in children with brain tumours in a middle-income country: national experience from Serbia. Childs Nerv Syst 39, 3169–3177 (2023). https://doi.org/10.1007/s00381-023-05958-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-023-05958-5