Abstract
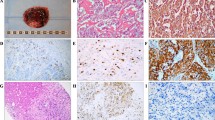
Paragangliomas (PGL) develop from the parasympathetic system in the head and neck (HN) and arise primarily in four distinct areas: Carotid body, vagal, middle ear, and larynx. Globally, the diagnosis and morphologic features are the same regardless of anatomic site, however the incidence, frequency of genetic alterations/syndromes and differential diagnosis vary. It is now recognized that nearly 40% of all HN PGLs are hereditary, including a significant subset without a known family history. Now pathologists are central to the evaluation for diagnosis and further management of patients with HNPGLs. Specifically, SDHB immunohistochemical evaluation is an excellent screening tool to detect tumors with alterations in the SDH family of genes that represent the majority of hereditary cases in HNPGL. Similarly, SDHB immunohistochemical analysis allows for screening of PGL syndrome associated tumors (gastrointestinal stromal tumor (GIST), renal cell carcinoma (RCC), and pituitary adenomas) that have now been linked by their overlapping gene alterations. Awareness of the spectrum of these syndromes, and their associated tumors, positions the pathologist to augment patient care and surveillance.



Similar content being viewed by others
References
Lee JH, Barich F, Karnell LH, et al. National Cancer Data Base report on malignant paragangliomas of the head and neck. Cancer. 2002;94:730–737.
Rodríguez-Cuevas S, López-Garza J, Labastida-Almendaro S. Carotid body tumors in inhabitants of altitudes higher than 2000 meters above sea level. Head Neck. 1998;20:374–8.
Boedeker CC, Hensen EF, Neumann HP, et al. Genetics of hereditary head and neck paragangliomas. Head Neck. 2014;36:907–16.
Pacak K, Wimalawansa SJ. Pheochromocytoma and paraganglioma. Endocr Pract. 2015;21:406–12.
Dahia PL. Pheochromocytoma and paraganglioma pathogenesis: learning from genetic heterogeneity. Nat Rev Cancer. 2014;14:108–19.
Castro-Vega LJ, Letouze E, Burnichon N, et al. Multi-omics analysis defines core genomic alterations in pheochromocytomas and paragangliomas. Nat Commun. 2015;6:6044.
Fishbein L. Pheochromocytoma and paraganglioma: genetics, diagnosis, and treatment. Hematol Oncol Clin North Am. 2016;30:135–50.
O’Neill S, O’Donnell M, Harkin D, Loughrey M, Lee B, Blair P. A 22-year Northern Irish experience of carotid body tumours. Ulster Med J. 2011;80:133–40.
Ferlito A, Barnes L, Wenig BM. Identification, classification, treatment, and prognosis of laryngeal paraganglioma. Review of the literature and eight new cases. Ann Otol Rhinol Laryngol. 1994;103:525–36.
Amato B, Bianco T, Compagna R, Siano M, Esposito G, Buffone G, et al. Surgical resection of carotid body paragangliomas: 10 years of experience. Am J Surg. 2014;207:293–8.
Langerman A, Athavale SM, Rangarajan SV, Sinard RJ, Netterville JL. Natural history of cervical paragangliomas: outcomes of observation of 43 patients. Arch Otolaryngol Head Neck Surg. 2012;138:341–5.
Qin RF, Shi LF, Liu YP, Lei DL, Hu KJ, Feng XH, et al. Diagnosis and surgical treatment of carotid body tumors: 25 years’ experience in China. Int J Oral Maxillofac Surg. 2009;38:713–8.
Sajid MS, Hamilton G, Baker DM; Joint Vascular Research Group. A multicenter review of carotid body tumour management. Eur J Vasc Endovasc Surg. 2007;34:127–30.
Carlson ML, Sweeney AD, Pelosi S, Wanna GB, Glasscock ME 3rd, Haynes DS. Glomus tympanicum: a review of 115 cases over 4 decades. Otolaryngol Head Neck Surg. 2015;152:136–42.
Capatina C, Ntali G, Karavitaki N, Grossman AB. The management of head-andneck paragangliomas. Endocr Relat Cancer. 2013;20:R291–R305.
Barnes L. Paraganglioma of the larynx. A critical review of the literature. ORL J Otorhinolaryngol Relat Spec. 1991;53:220–34.
Ferlito A, Milroy CM, Wenig BM, Barnes L, Silver CE. Laryngeal paraganglioma versus atypical carcinoid tumor. Ann Otol Rhinol Laryngol. 1995;104(1):78–83.
Barnes L. Paragangliomas of the larynx. J Laryngol Otol. 1993;107(7):664; author reply 665-6.
Myssiorek D, Rinaldo A, Barnes L, Ferlito A. Laryngeal paraganglioma: an updated critical review. Acta Otolaryngol. 2004;124(9):995–9.
de Azevedo-Gamas A, Gloor F. A very unusual case of tumor of the larynx. Unexpected anatomopathologic diagnosis. Ann Otolaryngol Chir Cervicofac. 1968;85:329–35.
Rüfenacht H, Mihatsch MJ, Jundt K, Gächter A, Tanner K, Heitz PU. Gastric epitheloid leiomyomas, pulmonary chondroma, non-functioning metastasizing extra-adrenal paraganglioma and myxoma: a variant of Carney’s triad. Report of a patient. Klin Wochenschr. 1985;63:282–4.
van Nederveen FH, Gaal J, Favier J, et al. An immunohistochemical procedure to detect patients with paraganglioma and phaeochromocytoma with germline SDHB, SDHC, or SDHD gene mutations: a retrospective and prospective analysis. Lancet Oncol. 2009;10(8):764–71.
Gill AJ, Benn DE, Chou A, et al. Immunohistochemistry for SDHB triages genetic testing of SDHB, SDHC, and SDHD in paraganglioma-pheochromocytoma syndromes. Hum Pathol. 2010;41(6):805–14.
Haller F, Moskalev EA, Faucz FR, et al. Aberrant DNA hypermethylation of SDHC: a novel mechanism of tumor development in Carney triad. Endocr Relat Cancer. 2014;21:567–77.
Papathomas TG, Oudijk L, Persu A, et al. SDHB/SDHA immunohistochemistry in pheochromocytomas and paragangliomas: a multicenter interobserver variation analysis using virtual microscopy: a Multinational Study of the European Network for the Study of Adrenal Tumors (ENS@T). Mod Pathol. 2015;28(6):807–21.
Korpershoek E, Favier J, Gaal J, et al. SDHA immunohistochemistry detects germline SDHA gene mutations in apparently sporadic paragangliomas and pheochromocytomas. J Clin Endocrinol Metab. 2011;96(9):E1472–6.
Menara M, Oudijk L, Badoual C, et al. SDHD immunohistochemistry: a new tool to validate SDHx mutations in pheochromocytoma/ paraganglioma. J Clin Endocrinol Metab. 2015;100(2):E287–91.
Baysal BE, Willett-Brozick JE, Lawrence EC, et al. Prevalence of SDHB, SDHC, and SDHD germline mutations in clinic patients with head and neck paragangliomas. J Med Genet. 2002;39(3):178–83.
Benn DE, Robinson BG, Clifton-Bligh RJ. 15 YEARS OF PARAGANGLIOMA: clinical manifestations of paraganglioma syndromes types 1–5. Endocr Relat Cancer. 2015;22:T91–103.
Kunst HP, Rutten MH, de Mönnink JP, Hoefsloot LH, Timmers HJ, Marres HA, et al. SDHAF2 (PGL2-SDH5) and hereditary head and neck paraganglioma. Clin Cancer Res. 2011;17:247–54.
Piccini V, Rapizzi E, Bacca A, et al. Head and neck paragangliomas: genetic spectrum and clinical variability in 79 consecutive patients. Endocr Relat Cancer. 2012;19(2):149–55.
Burnichon N, Brière JJ, Libé R, Vescovo L, Rivière J, Tissier F, et al. SDHA is a tumor suppressor gene causing paraganglioma. Hum Mol Genet. 2010;19:3011–20.
Miettinen M, Wang ZF, Sarlomo-Rikala M, Osuch C, Rutkowski P, Lasota J. Succinate dehydrogenase-deficient GISTs: a clinicopathologic, immunohistochemical, and molecular genetic study of 66 gastric GISTs with predilection to young age. Am J Surg Pathol. 2011;35:1712–21.
Williamson SR, Eble JN, Amin MB et al. Succinate dehydrogenase-deficient renal cell carcinoma: detailed characterization of 11 tumors defining a unique subtype of renal cell carcinoma. Modern pathology. 2015;28:80–94.
Gill AJ, Pachter NS, Chou A, et al. Renal tumors associated with germline SDHB mutation show distinctive morphology. Am J Surg Pathol. 2011;35:1578–85.
Dwight T, Mann K, Benn DE, et al. Familial SDHA mutation associated with pituitary adenoma and pheochromocytoma/paraganglioma. J Clin Endocrinol Metab. 2013;98:E1103–8.
Dénes J, Swords F, Rattenberry E, et al. Heterogeneous genetic background of the association of pheochromocytoma/paraganglioma and pituitary adenoma: results from a large patient cohort. J Clin Endocrinol Metab. 2015;100(3):E531–41.
Baysal BE, Maher ER: 15 YEARS OF PARAGANGLIOMA: genetics and mechanism of pheochromocytoma-paraganglioma syndromes characterized by germline SDHB and SDHD mutations. Endocr Relat Cancer 2015;22:T71–82.
Boikos SA, Xekouki P, Fumagalli E, et al. Carney triad can be (rarely) associated with germline succinate dehydrogenase defects. Eur J Hum Genet. 2016;24:569–73.
Offergeld C, Brase C, Yaremchuk S, et al. Head and neck paragangliomas: clinical and molecular genetic classification. Clinics. 2012;67(Suppl 1):19–28.
Neumann HP, Sullivan M, Winter A, et al. Germline mutations of the TMEM127 gene in patients with paraganglioma of head and neck and extraadrenal abdominal sites. J Clin Endocrinol Metab. 2011;96:E1279–82.
Barnes L, Taylor SR. Carotid body paragangliomas. A clinicopathologic and DNA analysis of 13 tumors. Arch Otolaryngol Head Neck Surg. 1990;116(4):447–53.
Barnes L, Taylor SR. Vagal paragangliomas: a clinical, pathological, and DNA assessment. Clin Otolaryngol Allied Sci. 1991;16(4):376–82.
Capatina C, Ntali G, Karavitaki N, Grossman AB. The management of head-and-neck paragangliomas. Endocr Relat Cancer. 2013;20(5):R291–305.
Lee JH, Barich F, Karnell LH, Robinson RA, Zhen WK, Gantz BJ, Hoffman HT; American College of Surgeons Commission on Cancer; American Cancer Society. National Cancer Data Base report on malignant paragangliomas of the head and neck. Cancer. 2002;94(3):730–7.
Sethi RV, Sethi RK, Herr MW, Deschler DG. Malignant head and neck paragangliomas: treatment efficacy and prognostic indicators. Am J Otolaryngol. 2013;34(5):431–8.
NGS in PPGL (NGSnPPGL) Study Group, Toledo RA, Burnichon N, Cascon A, Benn DE, et al. Consensus Statement on next-generation-sequencing-based diagnostic testing of hereditary phaeochromocytomas and paragangliomas. Nat Rev Endocrinol. 2016.
Ellis RJ, Patel D, Prodanov T, Nilubol N, Pacak K, Kebebew E. The presence of SDHB mutations should modify surgical indications for carotid body paragangliomas. Ann Surg. 2014;260(1):158–62.
Lenders JW, Duh QY, Eisenhofer G, et al; Endocrine society. Pheochromocytoma and paraganglioma: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2014;99:1915–42
Taïeb D, Kaliski A, Boedeker CC, et al. (2014). Current approaches and recent developments in the management of head and neck paragangliomas. Endocr Rev. 2014;35:795–819.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author has no conflicts of interest to declare.
Ethical approval
This article does not contain any studies with human participants or animals performed by the author.
Additional information
Proceedings of the 2017 North American Society of Head and Neck Pathology Companion Meeting (San Antonio, TX).
Rights and permissions
About this article
Cite this article
Williams, M.D. Paragangliomas of the Head and Neck: An Overview from Diagnosis to Genetics. Head and Neck Pathol 11, 278–287 (2017). https://doi.org/10.1007/s12105-017-0803-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12105-017-0803-4