Abstract
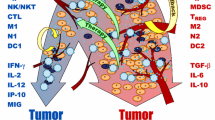
We develop a mathematical model of pancreatic cancer that includes pancreatic cancer cells, pancreatic stellate cells, effector cells and tumor-promoting and tumor-suppressing cytokines to investigate the effects of immunotherapies on patient survival. The model is first validated using the survival data of two clinical trials. Local sensitivity analysis of the parameters indicates there exists a critical activation rate of pro-tumor cytokines beyond which the cancer can be eradicated if four adoptive transfers of immune cells are applied. Optimal control theory is explored as a potential tool for searching the best adoptive cellular immunotherapies. Combined immunotherapies between adoptive ex vivo expanded immune cells and TGF-\(\beta \) inhibition by siRNA treatments are investigated. This study concludes that mono-immunotherapy is unlikely to control the pancreatic cancer and combined immunotherapies between anti-TGF-\(\beta \) and adoptive transfers of immune cells can prolong patient survival. We show through numerical explorations that how these two types of immunotherapies are scheduled is important to survival. Applying TGF-\(\beta \) inhibition first followed by adoptive immune cell transfers can yield better survival outcomes.







Similar content being viewed by others
References
Abdo J et al (2018) Immunotherapy plus cryotherapy: potential augmented abscopal effect for advanced cancers. Front Oncol 8:1–16
Anderson L, Jang SR-J, Yu J (2015) Qualitative behavior of systems of tumor-CD4\(^+\)-cytokine interactions with treatments. Math Methods Appl Sci 38:4330–4344
Arciero JC, Jackson TL, Kirschner DF (2004) A mathematical model of tumor-immune evasion and siRNA treatment. Dis Cont Dyn Syst Ser B 4(1):39–58
Bachem MG et al (2008) Pancreatic stellate cells role in pancreas cancer. Langenbecks Arch Surg 393:891–900
Bellone et al (2006) Cytokine expression profile in human pancreatic carcinoma cells and in surgical specimens: implications for survival. Cancer lmmunol Immunother 55:684–698
Burden T, Ernstberger J, Fister K (2004) Optimal control applied to immunotherapy. Dis Cont Dyn Sys Ser B 4:135–146
Castiglione F, Piccoli B (2007) Cancer immunotherapy, mathematical modeling and optimal control. J Theor Biol 247:723–732
Chung MJ et al (2014) Phase II clinical trial of ex vivo-expanded cytokine-induced killer cells therapy in advanced pancreatic cancer. Cancer Immunol Immunother 63(9):939–946
de Pillis L et al (2005) A validated mathematical model of cell-mediated immune response to tumor growth. Cancer Res 65(17):7950–7958
de Pillis L et al (2008) Optimal control of mixed immunotherapy and chemotherapy of tumors. J Biol Syst 16(1):51–80
Diefenbach A et al (2001) Rae1 and H60 ligands of the NKG2D receptor stimulate tumor immunity. Nature 413:165–171
Eftimie R et al (2010) Anti-tumour Th1 and Th2 immunity in the rejection of melanoma. J Theor Biol 265:467–480
Ellermeier J et al (2013) Therapeutic efficacy of bifunctional siRNA combining TGF-\(\beta 1\) silencing with RIG-I activation in pancreatic cancer. Cancer Res 73(6):1709–1720
Engelhart M, Lebiedz D, Sager D (2011) Optimal control for selected cancer chemotherapy ODE models: a view on the potential of optimal schedules and choice of objective function. Math Biosci 229:123–134
Fire A et al (1998) Potent and specific genetic interference by double-stranded RNA in Caenorhabditis elegans. Nature 391:806–811
Fleming W, Rishel R (1975) Deterministic and stochastic optimal control. Springer, New York
Friedman A, Hao W (2017) The role of exosomes in pancreatic cancer microenvironment. Bull Math Biol 79:1–23
Friedman A, Lai X (2018) Combination therapy for cancer with oncolytic virus and checkpoint inhibitor: a mathematical model. PLoS One 13(2):1–21
Gaspar NJ et al (2007) Inhibition of transforming growth factor beta signaling reduces pancreatic adenocarcinoma growth and invasiveness. Mol Pharmacol 72:152–161
Gold L (1999) The role for transforming growth factor-\(\beta \) (TGF-\(\beta \)) in human cancer. Crit Rev Oncog 10:303–360
Hanahan D, Weinberg RA (2011) Hallmarks of cancer: the next generation. Cell 144:646–674
Hariharan D et al (2008) Analysis of mortality rates for pancreatic cancer across the world. HPB 10:58–62
He D-H, Xu J-X (2017) A mathematical model of pancreatic cancer with two kinds of treatments. J Biol Syst 25(1):83–104
Heinemann V (2001) Gemcitabine: progress in the treatment of pancreatic cancer. Oncology 60(1):8–18
Hilmi M et al (2018) Immune therapies in pancreatic ductal adenocarcinoma: where are we now? World J Gastroent 24(20):2137–2151
Holen T et al (2001) Positional effects of short interfering RNAs targeting the human coagulation trigger tissue factor. Nucleic Acids Res 30:1757–1766
Hu X, Jang SR-J (2018a) Dynamics of tumor-CD4\(^+\)-cytokine-host cells interactions with treatments. Appl Math Comput 321:700–720
Hu X, Jang SR-J (2018b) Optimal treatments in cancer immunotherapy involving CD4\(^+\) T cells. WSEAS Trans Biol Biomed 15:48–67
Khajanchi S, Ghosh D (2015) The combined effects of optimal control in cancer remission. Appl Math Compu 271:375–388
Kirschner D, Panetta JC (1998) Modeling immunotherapy of the tumorimmune interaction. J Math Biol 37:235–252
Korobeinikov A et al (2016) Paradox of enrichment and system order reduction: bacteriophages dynamics as case study. Math Med. Biol 33:359–369
Kozono S et al (2013) Pirfenidone inhibits pancreatic cancer desmoplasia by regulating stellate cells. Cancer Res 73(7):2345–2356
Kuznetsov V et al (1994) Nonlinear dynamics of immunogenic tumors: parameter estimation and global bifurcation analysis. Bull Math Biol 56(2):295–321
Lenhart L, Workman JT (2007) Optimal control applied to biological models. Chapman & Hall, New York
Li X, Xu J-X (2016) A mathematical prognosis model for pancreatic patients receiving immunotherapy. J Theor Biol 406:42–51
Lipardi C et al (2001) RNAi as random degradative PCR: siRNA primers convert mRNA into dsRNAs that are degraded to generate new siRNAs. Cell 107:297–307
Louzoun Y et al (2014) A mathematical model for pancreatic cancer growth and treatments. J Theor Biol 351:74–82
Luo X et al (2016) Advances in cryoablation for pancreatic cancer. World J Gastroenterol 22(2):790–800
Mace TA et al (2013) Pancreatic cancer associated stellate cells promote differentiation of myeloid-derived suppressor cells in a stat3-dependent manner. Cancer Res 73:3007–3018
Martinez-Bosch N et al (2018) Immune evasion in pancreatic cancer: from mechanisms to therapy. Cancers 10(6):1–16
Maloney E et al (2017) Focused ultrasound for immuno-adjuvant treatment of pancreatic cancer: an emerging clinical paradigm in the era of personalized oncotherapy. Int Rev Immunol 36(6):338–351
Minelli A et al (2011) Controlled drug deliver in cancer immunotherapy: stability, optimization, and Monte Carlo analysis. SIAM J Appl Math 71:2220–2245
Morrison A et al (2018) Immunotherapy and prevention of pancreatic cancer. Trends Cancer 4(6):418–428
Nam JS et al (2008) Transforming growth factor beta subverts the immune system into directly promoting tumor growth through interleukin-17. Cancer Res 68(10):3915–3923
Niu L et al (2013) Combination treatment with comprehensive cryoablation and immunotherapy in metastatic pancreatic cancer. Pancreas 42:1143–1149
Patterson MA, Rao AV (2014) GPOPS-II: a MATLAB software for solving multiple-phase optimal control problems using hp-adaptive Gaussian quadrature collocation methods and sparse nonlinear programming. ACM Trans Math Softw 41(1):1–37
Rahib L et al (2014) Projecting cancer incidence and deaths to 2030: the unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Res 74(11):2913–2921
Siu H et al (1986) Tumor dormancy. I. Regression of BCL tumor and induction of a dormant tumor state in mice chimeric at the major histocompatibility complex. J lmmunol 137:1376–1382
Weinberg RA (2013) The biology of cancer, 2nd edn. Garland Science, London
Winograd R et al (2015) Induction of T-cell immunity overcomes complete resistance to PD-1 and CTLA-4 blockade and improves survival in pancreatic carcinoma. Cancer Immunol Res 3(4):399–411
Xu C, Wang J (2015) Delivery systems for siRNA drug development in cancer therapy. Asian J Pharm Sci 10:1–12
Xue H et al (2016) A novel tumor-promoting mechanism of IL-6 and the therapeutic efficacy of tocilizumab: Hypoxia-induced IL-6 is a potent autophagy initiator in glioblastoma via the p-STAT3-MIR155-3p-CREBRF pathway. Autophagy 12:1129–1152
Yates A, Callard R (2002) Cell death and the maintenance of immunological memory. Discrete Contin Dyn Syst Ser B 1(1):43–59
Zhao J et al (2016) Clinical and prognostic significance of serum transforming growth factor-\(\beta \) 1 levels in patients with pancreatic ductal adenocarcinoma. Br J Med Biol Res 49(8):1–5
Acknowledgements
We thank both reviewers for their many valuable comments that improved the original manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix: Sensitivity Analysis Based on the Survival Data of Niu et al.
Appendix: Sensitivity Analysis Based on the Survival Data of Niu et al.
From Fig. 1a of Niu et al. (2013), there is one patient who survived for about 25 months with no immunotherapy and there is one patient who survived for about 30 months with four additional immunotherapies. For both groups of patients, there is one patient who survived for only about three months. These survival times are not outliers of the data sets, and there are no numerical values for the mean and standard deviation given by Niu et al. (2013). If such information were provided, then change in the parameter values based on a 90% or 95% confidence interval of the clinical data would be performed instead. We therefore increase each individual parameter by up to 3000% or until the survival time lies outside of (120, 750) days for cryotherapy and (120, 900) days for cryo-immunotherapy. For both groups of patients, only the median immunity is considered in our numerical investigation. We also decrease each baseline parameter value until either up to 90% or the survival time falls outside of the above time intervals. These results are summarized in Tables 5 and 6 for cryotherapy and cryo-immunotherapy, respectively. In addition, the numbers of survival days for the corresponding maximum percentage of changes are also provided.
From Table 5, one can see that parameters \(\beta _3\), \(k_3\), \(m_3\), \(r_3\), \(k_4\), \(k_5\) and \(\mu _5\) can be increased up to 3000% and decreased up to 90% without changing the survival time of 215 days from the baseline parameters when no immunotherapy is applied. It is quite surprising to observe the lack of effect of parameter \(\beta _3\) since \(\beta _3\) is the tumor antigenicity. Increasing/decreasing tumor antigenicity cannot prolong/reduce a patient’s survival time in the proposed model when there is no immunotherapy. For the tumor killing rate \(\delta _1\), it can be increased only up to 400% with the corresponding survival time being 529 days. Increasing \(\delta _1\) further would result in tumor eradication since the number of cancer cell would be less than one. It is also clear that the survival time is sensitive with respect to two other parameters \(r_1\) and \(b_1\) which are tumor dependent. Increasing \(b_1\) or decreasing \(r_1\) beyond the percentage changes given in the table also results in tumor eradication. Further, the survival time is sensitive to the parameter \(\mu _4\), the decay rate of the pro-tumor cytokines. Increasing this natural loss rate can clear off the tumor.
With four immunotherapies, the survival time is 387 days for the baseline parameter values with median immunity. Table 6 implies that the survival time is insensitive to the parameters \(\beta _3, k_3, m_3, r_3, m_4, \beta _5, k_5\) and \(\mu _5\) since increasing each of these up to 3000% or decreasing each up to 90% yields the same number 387 of survival days. Comparing with the above discussion of Table 5 of no immunotherapies, there are two new parameters \(m_4\) and \(\beta _5\) that appear here. However, their corresponding changes in Table 5 are very small which can also be viewed as insensitive when there is no immunotherapy. The survival time is sensitive to the parameters \(\delta _1, r_1, b_1, \mu _4\) and \(\beta _4\). The first four of these parameters are also sensitive to the survival time when there is no immunotherapy. The additional parameter \(\beta _4\), the maximum activation rate of pro-tumor cytokines, is sensitive when immunotherapy is applied. In particular, the number of tumor cells is less than one and tumor eradication occurs when it is decreased 60% from its baseline value.
Since bar charts provide better visualization of the effects on survival time, we also summarize the two tables using graphs presented in Fig. 7a–b, respectively. However, it is unclear how much each individual parameter can be varied from the bar graphs, and hence, Tables 5 and 6 are also provided to reflect the maximum percentages of changes and their corresponding survival times.
Rights and permissions
About this article
Cite this article
Hu, X., Ke, G. & Jang, S.RJ. Modeling Pancreatic Cancer Dynamics with Immunotherapy. Bull Math Biol 81, 1885–1915 (2019). https://doi.org/10.1007/s11538-019-00591-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11538-019-00591-3