Abstract
Oncolytic virus (OV) is a genetically engineered virus that can selectively replicate in and kill tumor cells while not harming normal cells. OV therapy has been explored as a treatment for numerous cancers including glioblastoma, an aggressive and devastating brain tumor. Experiments show that extracellular matrix protein CCN1 limits OV therapy of glioma by orchestrating an antiviral response and enhancing the proinflammatory activation and migration of macrophages. Neutralizing CCN1 by antibody has been demonstrated to improve OV spread and tends to increase the time to disease progression. In this paper, we develop a mathematical model to investigate the effects of CCN1 on the treatment of glioma with oncolytic herpes simplex virus. We show that numerical simulations of the model are in agreement with the experimental results and then use the model to explore the anti-tumor effects of combining antibodies with OV therapy. Model simulations suggest that the macrophage content of the tumor is a critical factor to the success of OV therapy and to the reduction in tumor volume gained with the CCN1 antibody.








Similar content being viewed by others
References
Badie B, Schartner J (2001) Role of microglia in glioma biology. Microsc Res Tech 54(2):106–113
Badie B, Schartner JM (2000) Flow cytometric characterization of tumor-associated macrophages in experimental gliomas. Neurosurgery 46(4):957–962
Chen D, Roda JM, Marsh CB, Eubank TD, Friedman A (2012) Hypoxia inducible factors-mediated inhibition of cancer by GM-CSF: a mathematical model. Bull Math Biol 74(11):2752–2777
Desbaillets I, Tada M, De Tribolet N, Diserens AC, Hamou MF, Van Meir EG (1994) Human astrocytomas and glioblastomas express monocyte chemoattractant protein-1 (MCP-1) in vivo and in vitro. Int J Cancer 58(2):240–247
Dmitrieva N, Yu L, Viapiano M, Cripe TP, Chiocca EA, Glorioso JC, Kaur B (2011) Chondroitinase ABC I-mediated enhancement of oncolytic virus spread and antitumor efficacy. Clin Cancer Res 17(6):1362–1372
Emre Y, Imhof BA (2014) Matricellular protein CCN1/CYR61: a new player in inflammation and leukocyte trafficking. Sem Immunopathol, Springer 36:253–259
Freeman AI, Zakay-Rones Z, Gomori JM, Linetsky E, Rasooly L, Greenbaum E, Rozenman-Yair S, Panet A, Libson E, Irving CS et al (2006) Phase I/II trial of intravenous NDV-HUJ oncolytic virus in recurrent glioblastoma multiforme. Mol Ther 13(1):221–228
Friedman A, Tian J, Fulci G, Chiocca E, Wang J (2006) Glioma virotherapy: effects of innate immune suppression and increased viral replication capacity. Cancer Res 66(4):2314
Friedman A, Turner J, Szomolay B (2008) A model on the influence of age on immunity to infection with Mycobacterium tuberculosis. Exp Gerontol 43(4):275–285
Fulci G, Breymann L, Gianni D, Kurozomi K, Rhee SS, Yu J, Kaur B, Louis DN, Weissleder R, Caligiuri MA et al (2006) Cyclophosphamide enhances glioma virotherapy by inhibiting innate immune responses. Proc Natl Acad Sci 103(34):12,873–12,878
Fulci G, Dmitrieva N, Gianni D, Fontana EJ, Pan X, Lu Y, Kaufman CS, Kaur B, Lawler SE, Lee RJ et al (2007) Depletion of peripheral macrophages and brain microglia increases brain tumor titers of oncolytic viruses. Cancer Res 67(19):9398–9406
Gustafsson B, Kreiss H, Oliger J (2013) Time-dependent problems and difference methods. Wiley, Hoboken
Hao W, Friedman A (2014) The LDL–HDL profile determines the risk of atherosclerosis: a mathematical model. PloS One 9(3):e90,497
Haseley A, Alvarez-Breckenridge C, Chaudhury AR, Kaur B (2009) Advances in oncolytic virus therapy for glioma. Recent Pat CNS Drug Discov 4(1):1
Haseley A, Boone S, Wojton J, Yu L, Yoo JY, Yu J, Kurozumi K, Glorioso JC, Caligiuri MA, Kaur B (2012) Extracellular matrix protein CCN1 limits oncolytic efficacy in glioma. Cancer Res 72(6):1353–1362
Heo J, Reid T, Ruo L, Breitbach CJ, Rose S, Bloomston M, Cho M, Lim HY, Chung HC, Kim CW et al (2013) Randomized dose-finding clinical trial of oncolytic immunotherapeutic vaccinia JX-594 in liver cancer. Nat Med 19(3):329–336
Hwang TH, Moon A, Burke J, Ribas A, Stephenson J, Breitbach CJ, Daneshmand M, De Silva N, Parato K, Diallo JS et al (2011) A mechanistic proof-of-concept clinical trial with JX-594, a targeted multi-mechanistic oncolytic poxvirus, in patients with metastatic melanoma. Mol Ther 19(10):1913–1922
Jay P, Berge-Lefranc J, Marsollier C, Mejean C, Taviaux S, Berta P (1997) The human growth factor-inducible immediate early gene, CYR61, maps to chromosome 1p. Oncogene 14(14):1753–1757
Kim Y, Friedman A (2010) Interaction of tumor with its micro-environment: a mathematical model. Bull Math Biol 72(5):1029–1068
Kim Y, Roh S, Lawler S, Friedman A (2011) miR451 and AMPK mutual antagonism in glioma cell migration and proliferation: a mathematical model. PloS One 6(12):e28,293
Kim Y, Lee HG, Dmitrieva N, Kim J, Kaur B, Friedman A (2014) Choindroitinase ABC I-mediated enhancement of oncolytic virus spread and anti tumor efficacy: a mathematical model. PloS One 9(7):e102,499
Kurozumi K, Hardcastle J, Thakur R, Shroll J, Nowicki M, Otsuki A, Chiocca EA, Kaur B (2008) Oncolytic HSV-1 infection of tumors induces angiogenesis and upregulates CYR61. Mol Ther 16(8):1382–1391
Lau LF (2012) CCN1 and CCN2: blood brothers in angiogenic action. J Cell Commun Signal 6(3):121–123
Li Y, Zhu H, Zeng X, Fan J, Qian X, Wang S, Wang Z, Sun Y, Wang X, Wang W et al (2013) Suppression of autophagy enhanced growth inhibition and apoptosis of interferon-\(\beta \) in human glioma cells. Mol Neurobiol 47(3):1000–1010
Lun X, Yang W, Alain T, Shi ZQ, Muzik H, Barrett JW, McFadden G, Bell J, Hamilton MG, Senger DL et al (2005) Myxoma virus is a novel oncolytic virus with significant antitumor activity against experimental human gliomas. Cancer Res 65(21):9982–9990
Marino S, Hogue IB, Ray CJ, Kirschner DE (2008) A methodology for performing global uncertainty and sensitivity analysis in systems biology. J Theor Biol 254(1):178–196
Markert JM, Liechty PG, Wang W, Gaston S, Braz E, Karrasch M, Nabors LB, Markiewicz M, Lakeman AD, Palmer CA et al (2009) Phase Ib trial of mutant herpes simplex virus G207 inoculated pre-and post-tumor resection for recurrent GBM. Mol Ther 17(1):199–207
Morantz RA, Wood GW, Foster M, Clark M, Gollahon K (1979) Macrophages in experimental and human brain tumors: part 2: studies of the macrophage content of human brain tumors. J Neurosurg 50(3):305–311
Msaouel P, Dispenzieri A, Galanis E (2009) Clinical testing of engineered oncolytic measles virus strains in the treatment of cancer: an overview. Curr Opin Mol Ther 11(1):43
Nakao A, Kasuya H, Sahin T, Nomura N, Kanzaki A, Misawa M, Shirota T, Yamada S, Fujii T, Sugimoto H et al (2011) A phase I dose-escalation clinical trial of intraoperative direct intratumoral injection of HF10 oncolytic virus in non-resectable patients with advanced pancreatic cancer. Cancer Gene Ther 18(3):167–175
Parney IF, Waldron JS, Parsa AT (2009) Flow cytometry and in vitro analysis of human glioma-associated macrophages. J Neurosurg 110(3):572
Patel MR, Kratzke RA (2013) Oncolytic virus therapy for cancer: the first wave of translational clinical trials. Transl Res 161(4):355–364
Rhodes J, Sharkey J, Andrews P (2009) Serum IL-8 and MCP-1 concentration do not identify patients with enlarging contusions after traumatic brain injury. J Trauma Acute Care Surg 66(6):1591–1598
Rochat R, Liu X, Murata K, Nagayama K, Rixon F, Chiu W (2011) Seeing the portal in herpes simplex virus type 1 B capsids. J Virol 85(4):1871–1874
Roggendorf W, Strupp S, Paulus W (1996) Distribution and characterization of microglia/macrophages in human brain tumors. Acta Neuropathol 92(3):288–293
Stupp R, Mason WP, Van Den Bent MJ, Weller M, Fisher B, Taphoorn MJ, Belanger K, Brandes AA, Marosi C, Bogdahn U et al (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 352(10):987–996
Thorne A, Meisen W, Russell L, Yoo J, Bolyard C, Lathia J, Rich J, Puduvalli V, Mao H, Yu J et al (2014) Role of cysteine-rich 61 protein (CCN1) in macrophage-mediated oncolytic herpes simplex virus clearance. Mol Ther 2(9):1678–1687
Thorne SH, Liang W, Sampath P, Schmidt T, Sikorski R, Beilhack A, Contag CH (2010) Targeting localized immune suppression within the tumor through repeat cycles of immune cell-oncolytic virus combination therapy. Mol Ther 18(9):1698–1705
Tietz NW (1995) Clinical guide to laboratory tests. WB Saunders Co, Philadelphia
Tönjes M, Barbus S, Park YJ, Wang W, Schlotter M, Lindroth AM, Pleier SV, Bai AH, Karra D, Piro RM et al (2013) BCAT1 promotes cell proliferation through amino acid catabolism in gliomas carrying wild-type IDH1. Nat Med 19(7):901–908
Vähä-Koskela M, Hinkkanen A (2014) Tumor restrictions to oncolytic virus. Biomedicines 2(2):163–194
Vehlow A, Cordes N (2013) Invasion as target for therapy of glioblastoma multiforme. Biochim Biophys Acta (BBA) Rev Cancer 1836(2):236–244
Xie Q, Mittal S, Berens ME (2014) Targeting adaptive glioblastoma: an overview of proliferation and invasion. Neuro-oncology 16(12):1575–1584
Yang GP, Lau LF (1991) CYR61, product of a growth factor-inducible immediate early gene, is associated with the extracellular matrix and the cell surface. Cell Growth Differ Mol Biol J Am Assoc Cancer Res 2(7):351–357
Yoo JY, Haseley A, Bratasz A, Chiocca EA, Zhang J, Powell K, Kaur B (2012) Antitumor efficacy of 34.5 ENVE: a transcriptionally retargeted and “Vstat120”-expressing oncolytic virus. Mol Ther 20(2):287–297
Zhang X, Yu W, Dong F (2012) Cysteine-rich 61 (CYR61) is up-regulated in proliferative diabetic retinopathy. Graefe’s Arch Clin Exp Ophthalmol 250(5):661–668
Acknowledgments
K. Jacobsen and A. Friedman are supported by the Mathematical Biosciences Institute and the National Science Foundation under Grant No. DMS-0931642. L. Russell and B. Kaur are supported by the National Institutes of Health under Grant Nos. RO1NS064607-01, RO1CA150153-01 and P30NS045758.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
1.1 Parameter Estimation for the Dimensionalized Model
1.1.1 Diffusion and Chemotactic Coefficients
We assume that the diffusion coefficients of all tumor and immune cells are equal and take them to be \(8.64\times 10^{-5}\) \(\hbox {mm}^2\hbox {day}^{-1}\) (Hao and Friedman 2014; Kim et al. 2011). We assume that the diffusion coefficient, \(D_\mathrm{p}\), for a protein \(p\) can be calculated from its molecular weight, \(M_\mathrm{p}\), by the formula \(D_\mathrm{p}=KM_\mathrm{p}^{2/3}\) where \(K=0.325~\hbox {mm}^2\hbox {day}^{-1}\hbox {dalton}^{-2/3}\), as explained in Hao and Friedman (2014). The molecular weight of CCN1 is 42027 daltons (Jay et al. 1997). Hence, the diffusion coefficient of CCN1 is estimated by
The sensitivity of macrophage to chemoattractants is difficult to estimate and values in the literature include the range from \(8.64 \times 10^{4}\) to \(1.73\times 10^9\) \(\hbox {mm}^5\hbox {g}^{-1}\hbox {day}^{-1}\) (Hao and Friedman 2014; Kim and Friedman 2010). We choose an intermediate value of \(\chi _\mathrm{C}=\chi _\mathrm{P}=10^6\,\hbox {mm}^5\hbox {g}^{-1}\hbox {day}^{-1}\).
1.1.2 Estimate of \(d_\mathrm{C}\), \(\lambda _\mathrm{C},\mu _\mathrm{C}\) from Eq. (7)
We assume that the half-life of extracellular CCN1 is 30 h (Yang and Lau 1991) and accordingly take
CCN1 is highly overexpressed in glioma so we consider a typical concentration of CCN1 in tumor to be \(C_0=10^{-9}\hbox {g}\,\hbox {mm}^{-3}\) (Zhang et al. 2012). The steady-state of Eq. (7) is
We assume that with no virus present, CCN1 reaches the steady-state concentration \(C_0\); therefore, we take
Furthermore, we take the density of tumor cells and macrophages (Eq. (8) to be \(\theta = 10^6\,\hbox {cells}/\hbox {mm}^3\) (Friedman et al. 2006) and assume that approximately one-tenth of the tumor cells are infected by the virus (Fulci et al. 2006). Hence, we take a typical concentration of infected tumor cells to be \(y_0 = 10^5\, \hbox {cells}/\hbox {mm}^3\). Experimental evidence shows that in the presence of oncolytic virus, CCN1 gene expression is approximately three times higher than without virus (Haseley et al. 2012; Fig. 1a). Accordingly, we let \(C_1=3C_0\) and from Eq. (18), we deduce that
1.1.3 Estimate of \(b,d_\mathrm{y},k_\mathrm{y}, d_\mathrm{v},\delta _\mathrm{y},\delta _\mathrm{v}\) from Eqs. (2) and (5)
The lytic cycle of HSV-1 is approximately 12–16 h (Kurozumi et al. 2008). Accordingly, we take \(d_\mathrm{y}\), the lysis rate of infected tumor cells, to be \(1.5\,\hbox {day}^{-1}\). CCN1 has been shown to induce a cellular antiviral response that reduces viral replication; experimental data measuring luciferase-encoded virus indicates that the quantity of infectious particles is significantly reduced in the presence of CCN1 (Haseley et al. 2012; Figs. 2, 3). Therefore, we estimate that \(k_\mathrm{y}=0.1/C_0=10^8\,\hbox {mm}^3\hbox {g}^{-1}\). For oncolytic HSV-1, the burst size ranges from 10 to 100 (Friedman et al. 2006). We choose the burst size, \(b\), to be \(50\, \hbox {viruses}/\hbox {cell}\). Friedman et al. (2006) estimated the clearance rate of free HSV-1 to be \(0.6\,\hbox {day}^{-1}\) in a model that studied the affects of cyclophosphamide on virotherapy of glioma. We take the clearance rate of virus, \(\delta _\mathrm{v}\), to be \(0.5\,\hbox {day}^{-1}\).
Friedman et al. (2006) did not consider particular immune cell populations and estimated the average immune killing rate of infected cells to be \(4.8\times 10^{-7}\,\hbox {mm}^3\,\hbox {cell}^{-1}\,\hbox {day}^{-1}\). We take the killing rate of infected cells by macrophage, \(\delta _\mathrm{y}\), to be \(4.8\times 10^{-8}\,\hbox {mm}^3\,\hbox {cell}^{-1}\,\hbox {day}^{-1}\). We make the assumption that the rate of macrophage-mediated killing is proportional to the surface area of the target. We assume the tumor cells to be spherical with a diameter of \(40\mu m\) (Tönjes et al. 2013). HSV-1 is an icosahedral virus with a diameter of approximately \(200\,nm\) (Rochat et al. 2011). Therefore, the ratio of the surface area of a tumor cell to surface area of a virus is approximately \(4\times 10^4\), and we accordingly take
1.1.4 Estimate of \(\alpha _\mathrm{C},k_\mathrm{C}\) from Eqs. (2) and (5) and \(m\)
As explained in Sect. 3, we take the default value of the macrophage content, \(m\), to be 0.10 and, according to Eq. (15), take the density of macrophage in a typical tumor to be \(M_0= 10^5\,\hbox {cells}\,\hbox {mm}^{-3}\). As supported by experimental evidence (Thorne et al. 2014, Figure 3b), we assume the macrophage density under OV treatment, \(M_1\), is 1.5 times higher than in a typical tumor. Cytotoxicity experiments by Haseley et al. (unpublished) suggest that macrophage-mediated killing resulted in 1.2 times more cell death in glioma cells overexpressing CCN1 compared to control glioma cells. Therefore, considering the term for macrophage killing of infected cells in Eq. (2), we estimate that
Here we assume that the number of infected cells is inversely proportional to the number of macrophages, so that \(y_1=\frac{y_0}{1.5}\) since \(M_1=1.5M_0\). We take \(k_\mathrm{C}=2C_0\) and thus solve for \(\alpha _\mathrm{C}\) to get \(\alpha _\mathrm{C}=1\).
1.1.5 Estimate of \(\lambda _\mathrm{x}\), \(k_\mathrm{x}\), and \(\beta _\mathrm{x}\) from Eq. (1)
Since high expression of CCN1 correlates with poor prognosis, we assume that the inhibition of tumor growth due to the IFN response orchestrated by CCN1 is not as strong as the inhibition of viral replication in Eq. (5). Therefore, we estimate \(k_\mathrm{x}=0.01/C_0=10^7\,\hbox {mm}^3\hbox {g}^{-1}\), so that \(k_\mathrm{x}=0.1k_\mathrm{y}\). We take the proliferation rate of uninfected glioma cells to be \(\lambda _\mathrm{x}=0.2\,\hbox {day}^{-1}\) based on data measuring the growth of subcutaneous glioma tumors in a control group of mice treated with phosphate-buffered saline (Yoo et al. 2012). We choose the infection rate of cells by virus to be \(\beta _\mathrm{x}=1.7\times 10^{-8}\,\hbox {mm}^3\hbox {day}^{-1}\hbox {virus}^{-1}\) as estimated by Friedman et al. (2006).
1.1.6 Estimate of \(\lambda _\mathrm{M}, \alpha _\mathrm{MC}, k_\mathrm{MC}\) from Eq. (4)
Experimental results by Thorne et al. Thorne et al. (2014) indicate that OV-induced CCN1 significantly increases macrophage migration and enhances the proinflammatory activation of macrophages. Accordingly, we take \(\alpha _\mathrm{MC}=2\). We also take \(k_\mathrm{MC}=C_0\). The death rate of macrophages, \(d_\mathrm{M}\), is taken to be \(0.015\,\hbox {day}^{-1}\) (Hao and Friedman 2014; Friedman et al. 2008).
To estimate the constant source of macrophages, \(\lambda _\mathrm{M}\), we consider the dynamics of the macrophage density at a spatially homogeneous steady-state without virus. In that case, there is a nonnegative advection velocity, \(u\), and Eq. (1) implies that
Substituting this expression into the homogeneous steady state of Eq. (4) gives
so that
1.1.7 Estimate of \(\lambda _\mathrm{P}, \alpha _\mathrm{M}, k_\mathrm{M}\) from Eq. (6)
We assume that in normal healthy tissue, the concentration of MCP-1 is \(P_0=3\times 10^{-13}\hbox {g}\,\hbox {mm}^{-3}\) (Rhodes et al. 2009) and that the degradation rate of MCP-1 is \(d_\mathrm{P}=1.7\) \(\hbox {day}^{-1}\) (Chen et al. 2012). According to Eq. (6), the steady-state concentration of MCP-1 satisfies the equation
and, therefore, with \(y=0\) and \(P=P_0\),
Experimental data show that, compared to uninfected glioma cells, MCP-1 expression is approximately 2.5 times larger in infected glioma cells without macrophages present and about 13 times higher in infected glioma cells cultured with macrophages (Thorne et al. 2014, Figure 5a). Accordingly, we let \(P_1=2.5P_0\) and \(P_2=13P_0\). By Eq. (20), we can estimate \(\lambda _\mathrm{P}\), the rate of MCP-1 production by infected glioma cells, by
and \(\alpha _\mathrm{M}\), corresponding to further production of MCP-1 due to macrophage signaling, by
where we assumed that
1.1.8 Estimate of \(\tilde{\alpha },k_\mathrm{P},\tilde{M}\) from Boundary Condition Eq. (14)
The density of macrophages in the blood ranges from \(2\times 10^4\) to \(10^5\) \(\hbox {cells}/\hbox {mL}\) (Tietz 1995). Accordingly, we choose \(\tilde{M} = 50\,\hbox {cells}\,\hbox {mm}^{-3}\). We also take \(\tilde{\alpha } = 1\) and \(k_\mathrm{P}=P_0\).
1.2 Nondimensionalized Model with Fixed Boundary
We nondimensionalize the cell and virus densities by \(\overline{x} = x/\theta \), \(\overline{y} = y/\theta \), \(\overline{n} = n/\theta \), \(\overline{M} = M/\theta \), \(\overline{v}=\frac{v}{b\theta }\). The protein concentrations are nondimensionalized by \(\overline{P}=P/P_0\) and \(\overline{C}=C/C_0\) where \(P_0\) and \(C_0\) are the reference concentrations given in Table 4. Correspondingly, other parameters are nondimensionalized:
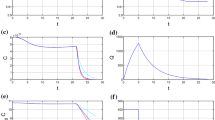
We eliminate the equation for dead cells by Eq. (8) and fix the moving boundary by making the transformation \(\overline{r}=r/R(t)\). Dropping the bar notation for simplicity, we obtain the following nondimensionalized model for \(r \in (0,1)\) and \(t > 0\):
With this transformation, the moving boundary condition (Eq. (10)) becomes Eq. (29). The boundary conditions at the tumor center remain unchanged so that
while the boundary conditions at the boundary of the tumor, Eqs. (13), (14), become
1.3 Numerical Scheme
We rewrite the nondimensionalized model (22)–(29) as
where \(D_z = D\) for \(z = x,y,M\). The advection coefficients are given by
and the reaction terms are given by
We formulate a finite difference upwind scheme to solve (30)–(35). Determining an upper bound for \(A_z\) in order to calculate the CFL condition (Gustafsson et al. 2013) is not analytically feasible. Thus, we use an adaptive scheme to ensure stability of the numerical method.
The mesh is defined as follows. Let
for \(i=1,\ldots ,N\) where \(\varDelta r = \frac{1}{N-1}\); thus \(r_1=0\) and \(r_\mathrm{n}=1\). We take \(N=50\). Let \(t_1=0\) and
for \(n = 1,2,\ldots \) where \(\varDelta t_{n}\) is chosen according to Eq. (47) below. Let \(z^n_i\) denote the numerical solution approximating \(z(r_i,t_\mathrm{n})\) for \(z = x,y,M,v,P,C,u\) and let \(R^n\) denote \(R(t_\mathrm{n})\).
According to (16) and (17), the initial conditions are \(x_i^1 = 1-\tilde{M}\), \(y_i^1=0\), \(M_i^1 = \tilde{M}\), \(v_i^1 = a\exp (r_i^2/(2\sigma ^2))\), \(P_i^1 = C_i^1 = 1\) for \(i=1,\ldots ,N\) and \(R^1 = 3\).
Given \(R^{n}\) and \(z^{n}\) for \(z = x,y,M,v,P,C\) we calculate \(R^{n+1}\) and \(z^{n+1}\) according to the following scheme:
-
1.
Compute \(F^{n}, F^{n}_z\) for \(z = x,y,M,v,P,C\) according to Eqs. (38)–(44) where the chemotaxis terms in \(F\) and \(F_\mathrm{M}\) are approximated by the form:
$$\begin{aligned}&\dfrac{\chi _\mathrm{P}}{(R^n)^2}\dfrac{1}{r_i^2\varDelta r^2}\left( r_{i+\frac{1}{2}}^2\left( \dfrac{M^n_{i+1}+M^n_{i}}{2}\right) (P^n_{i+1}-P^n_{i})\right. \nonumber \\&\quad \left. -r_{i-\frac{1}{2}}^2\left( \dfrac{M^n_{i}+M^n_{i-1}}{2}\right) (P^n_{i}-P^n_{i-1})\right) \end{aligned}$$(45)for \(i=2,...,N-1\) where \(r_{i+\frac{1}{2}} = r_i +\frac{\varDelta r}{2}\).
-
2.
Compute the advection velocity \(u^{n}\), according to Eq. (34), with the trapezoidal rule:
$$\begin{aligned} u_i^n = \dfrac{1}{r_i^2}\left( r_{i-1}^2u^n_{i-1}+\dfrac{R^n\varDelta r}{2}(r_i^2F^n_i+r^2_{i-1}F^n_{i-1})\right) \end{aligned}$$(46)for \(i=2,\ldots ,N\) where \(u^n_1 = 0\).
-
3.
Compute \(A_z^{n}\) for \(z = x,y,M,v,P,C\) according to Eqs. (36) and (37).
-
4.
Compute \(\Delta t_{n}\) as follows:
$$\begin{aligned} \Delta t_\mathrm{n} = \dfrac{0.1\Delta r}{\max (|A_\mathrm{x}^n|,|A_\mathrm{v}^n|,|A_\mathrm{P}^n|,|A_\mathrm{C}^n|)} \end{aligned}$$(47)in order to satisfy the CFL condition.
-
5.
Compute \(z_i^{n+1}\) for \(z = x,y,M,v,P,C\) and \(i=2,\ldots ,N-1\) using the upwind scheme:
$$\begin{aligned} z_i^{n+1}= & {} z_i^n + \Delta t_\mathrm{n}\left[ \dfrac{D_z}{(R^n)^2}\dfrac{1}{\varDelta r^2}\left( z^n_{i+1}-2z^n_i+z^n_{i-1}\right) \right. \nonumber \\&\quad \left. -\left( [A_z^+]_i^n[z_r^-]_i^n+[A_z^-]_i^n[z_r^+]_i^n\right) + [F_z]_i^n \right] \end{aligned}$$(48)where \(A_z^+=\max (A_z,0)\), \(A_z^-=\min (A_z,0)\), \([z_r^-]_i^n = \dfrac{z_i^n-z_{i-1}^n}{\Delta r}\), and \([z_r^+]_i^n = \dfrac{z_{i+1}^n-z_{i}^n}{\Delta r}\). Use the boundary conditions (30)–(32) to calculate \(z_i^n\) for \(i=1,N\).
-
6.
Compute \(R^{n+1}\), according to Eq. (29), by
$$\begin{aligned} R^{n+1} = R^{n} + \Delta t_{n} u_\mathrm{n}^{n}. \end{aligned}$$(49)
Rights and permissions
About this article
Cite this article
Jacobsen, K., Russell, L., Kaur, B. et al. Effects of CCN1 and Macrophage Content on Glioma Virotherapy: A Mathematical Model. Bull Math Biol 77, 984–1012 (2015). https://doi.org/10.1007/s11538-015-0074-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11538-015-0074-8