Abstract
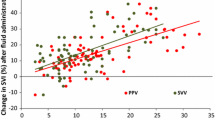
Changes in stroke volume (deltaSV) induced by a lung recruitment manoeuvre (LRM) have been shown to accurately predict fluid responsiveness during protective mechanical ventilation. Cardiac output monitors are used in a limited number of surgical patients. In contrast, all patients are monitored with a pulse oximeter, that may enable the continuous monitoring of a peripheral perfusion index (PI). We postulated that changes in PI (deltaPI) may reflect deltaSV during brief modifications of cardiac preload. We studied 47 patients undergoing neurosurgery and ventilated with a tidal volume of 6–8 ml/kg. All patients were monitored with a pulse contour system enabling the continuous monitoring of SV and with a pulse oximeter enabling the continuous monitoring of PI. LRMs were performed by increasing airway pressure up to 30 cmH20 for 30 s. Fluid loads (250 ml of saline 0.9% in 10 min) were performed only in patients who experienced a deltaSV > 30% during LRMs (potential fluid responders). LRMs induced a 26% decrease in SV (p < 0.05) and a 27% decrease in PI (p < 0.05). We observed a fair relationship between deltaPI and deltaSV (r2 = 0.34). A deltaPI ≥ 26% predicted a deltaSV > 30% with a sensitivity of 83% and a specificity of 78% (AUC = 0.84, 95%CI 0.71–0.93). 24 patients experienced a deltaSV > 30% and subsequently received fluid. Fluid loads induced a 16% increase in SV and a 17% increase in PI, but fluid-induced deltaPI and deltaSV were weakly correlated (r2 = 0.19). In neurosurgical patients, we conclude that deltaPI may be used as a surrogate for deltaSV during LRMs but not during fluid loading.




Similar content being viewed by others
References
Corsini I, Cecchi A, Coviello C, Dani C. Perfusion index and left ventricular output correlation in healthy term infants. Eur J Pediatr. 2017;176:1013–8.
Van Genderen ME, Bartels SA, Lima A, et al. Peripheral perfusion index as an early predictor for central hypovolemia in awake healthy volunteers. Anesth Analg. 2013;116:351–6.
Toyama S, Kakumoto M, Morioka M, et al. Perfusion index derived from a pulse oximeter can predict the incidence of hypotension during spinal anaesthesia for Caesarean delivery. Brit J Anaesth. 2013;111:235–41.
Abdelnasser A, Abdelhamid B, Elsonbaty A, Hasanin A, Rady A. Predicting successful supraclavicular brachial plexus block using pulse oximeter perfusion index. Brit J Anaesth. 2017;119:276–80.
Kus A, Gurkan Y, Gormus SK, Solak M, Toker K. Usefulness of perfusion index to detect the effect of brachial plexus block. J Clin Monit Comput. 2013;27:325–8.
Jeng EIH, Gravenstein N, Klodell CT. Perfusion index: an indicator of success during endoscopic thoracic sympathectomy for hyperhidrosis. Ann Thorac Surg. 2017;104:426–30.
Ginosar Y, Weiniger CF, Meroz Y, et al. Pulse oximeter perfusion index as an early indicator of sympathectomy after epidural anesthesia. Acta Anaesthesiol Scand. 2009;53:1018–26.
Beurton A, Teboul JL, Gavelli F, et al. The effects of passive leg raising may be detected by the plethysmographic oxygen saturation signal in critically ill patients. Crit Care. 2019;23:1–10.
Monnet X, Teboul JL. Passive leg raising: Five rules, not a drop of fluid! Crit Care. 2015;19:18–20.
Michard F, Biais M. Rational fluid management: dissecting facts from fiction. Brit J Anaesth. 2012;108:369–71.
Benes J, Giglio M, Brienza N, Michard F. The effects of goal-directed fluid therapy based on dynamic parameters on post-surgical outcome: a meta-analysis of randomized controlled trials. Crit Care. 2014;18:584.
Georges D, de Courson H, Lanchon R, Sesay M, Nouette-Gaulain K, Biais M. End-expiratory occlusion maneuver to predict fluid responsiveness in the intensive care unit: an echocardiographic study. Crit Care. 2018;22:1–8.
Biais M, Ph D, Lanchon R, et al. Changes in stroke volume induced by lung recruitment maneuver predict fluid responsiveness in mechanically ventilated patients in the operating room. Anesthesiology. 2017;126:260–67.
Futier E, Constantin J-M, Paugam-Burtz C, et al. A trial of intraoperative low-tidal-volume ventilation in abdominal surgery. N Engl J Med. 2013;369:428–37.
Ray P, Ph D, Manach Y, Le, et al. Statistical evaluation of a biomarker. Anesthesiology. 2010;112:1023–40.
Cannesson M, Le Manach Y, Hofer CK, et al. Assessing the diagnostic accuracy of pulse pressure variations for the prediction of fluid responsiveness: a “gray zone” approach. Anesthesiology. 2011;115:231–41.
Jourdain P, Pouchot J. A gray zone assigned to inconclusive results of quantitative diagnostic tests: application to the use of brain natriuretic peptide for diagnosis of heart failure in acute dyspneic patients. Clin Chem. 2006;2235:2229–35.
Carpenter J, Bithell J. Bootstrap confidence intervals: when, which, what ? A practical guide for medical statisticians. Stat Med. 2000;19:1141–64.
Michard F, Teboul JL. Predicting fluid responsiveness in ICU patients: a critical analysis of the evidence. Chest. 2002;121:2000–8.
Michard F. Changes in arterial pressure during mechanical ventilation. Anesthesiology. 2005;103:419–28.
Michard F, Chemla D, Teboul JL. Applicability of pulse pressure variation: how many shades of grey? Crit Care. 2015;19:15–7.
Biais M, Mazocky E, Stecken L, et al. Impact of systemic vascular resistance on the accuracy of the pulsioflex device. Anesth Analg. 2017;124:487–93.
Monnet X, Vaquer S, Anguel N, et al. Comparison of pulse contour analysis by Pulsioflex and Vigileo to measure and track changes of cardiac output in critically ill patients. Brit J Anaesth. 2015;114:235–43.
Funding
Support was provided solely from institutional and/or departmental sources.
Author information
Authors and Affiliations
Contributions
All authors made substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data; or the creation of new software used in the work; drafted the work or revised it critically for important intellectual content; approved the version to be published; and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
M.B received honoraria from Edwards Lifesciences and Pulsion Medical System as a lecturer. F.M is managing director of MiCo, a Swiss consulting firm. MiCo does not sell any medical products and FM does not own any shares and does not receive any royalties from any MedTech companies. Other authors have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the national research committee (Comité d’Ethique pour la recherche en Anesthésie-Réanimation, IRB-00010254-2018-118) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
de Courson, H., Michard, F., Chavignier, C. et al. Do changes in perfusion index reflect changes in stroke volume during preload-modifying manoeuvres?. J Clin Monit Comput 34, 1193–1198 (2020). https://doi.org/10.1007/s10877-019-00445-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-019-00445-2