Abstract
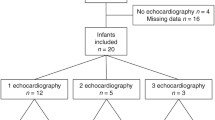
Perfusion index (PI) is a non-invasive marker of peripheral perfusion which is detected by an oximeter. We aimed to assess the correlation between PI and left ventricular output (LVO) in healthy term infants at the time of the screening for congenital heart disease (CHD). PI was measured at 48±2 h of life in the infant’s right hand (PIrh) and in one foot (PIf) contemporary to SpO2 for CHD screening. Heart ultrasound was performed immediately after the screening procedure for measuring LVO. Forty-nine healthy term infants were studied. PIrh and PIf were 1.9 ± 0.6 and 1.9 ± 0.8, respectively, and their values were significantly correlated (p < 0.0001) with a coefficient r = 0.8. Bland–Altman analysis shows a mean difference of −0.06 ± 0.47 (95%LOA −0.98–0.86). PIrh correlates with LVO (r = 0.68) and LVO/kg (r = 0.61) with an increase of 151 mL/min (95%CI 103–198) of LVO and 42 mL/kg/min (95%CI 26–58) of LVO/kg per point of PIrh. PIf correlates with LVO (r = 0.74) and LVO/kg (r = 0.73) with an increase of 123 mL/min (95%CI 90–155) of LVO and 37 mL/kg/min (95%CI 27–47) of LVO/kg per point of PIf.
Conclusion: PI is significantly correlated with LVO in healthy term infants. These results support the theoretical potential role of PI in the CHD screening.
What is Known: • Perfusion index is an indirect measure of perfusion which depends on cardiac output and peripheral vascular resistance whose normal values have been documented in term and preterm infants in the first days of life. • Perfusion index has been proposed for the screening of congenital heart disease with duct-dependent systemic circulation in term infants. |
What is New: • Perfusion index shows a significant correlation with the left ventricular output in term infants at the moment of the screening for congenital heart disease. • Perfusion index might have a theoretical role in improving the accuracy of pulse oximetry in the screening of CHD associated to low systemic flow. |



Similar content being viewed by others
Change history
05 June 2017
An erratum to this article has been published.
Abbreviations
- CHD:
-
Congenital heart disease
- LVO:
-
Left ventricular output
- PI:
-
Perfusion index
- RC:
-
Repeatability coefficient
- RVO:
-
Right ventricular output
- SpO2 :
-
Pulse oximetry
- SVCf:
-
Superior vena cava flow
- VTI:
-
Velocity-time integral
References
Cresi F, Pelle E, Calabrese R, Costa L, Farinasso D, Silvestro L (2010) Perfusion index variations in clinically and hemodynamically stable preterm newborns in the first week of life. Ital J Pediatr 36:6. doi:10.1186/1824-7288-36-6
Ewer AK (2013) Review of pulse oximetry screening for critical congenital heart defects in newborn infants. Curr Opin Cardiol 28:92–6. doi:10.1097/HCO.0b013e32835d7e42
Fixler DE, Xu P, Nembhard WN, Ethen MK, Canfield MA (2014) Age at referral and mortality from critical congenital heart disease. Pediatrics 134:e98–e105
Granelli AD, Östman-Smith I (2007) Noninvasive peripheral perfusion index as a possible tool for screening for critical left heart obstruction. Acta Paediatr 96:1455–1459
Granelli AD, Wennergren M, Sandberg K, Mellander M, Bejlum C, Inganas L, Eriksson M, Segerdahl N, Agren A, Ekman-Joelsson BM, Sunnegardh J, Verdicchio M, Ostman-Smith I (2009) Impact of pulse oximetry screening on the detection of duct dependent congenital heart disease: a Swedish prospective screening study in 39 821 newborns. BMJ 338:a3037
Groves AM, Chiesa G, Durighel G, Goldring ST, Fitzpatrick JA, Uribe S, Razavi R, Hajnal JV, Edwards AD (2011) Functional cardiac MRI in preterm and term newborns. Arch Dis Child Fetale and Neonatal Ed 96:86–91. doi:10.1136/adc.2010.189142
Hoffman JIE, Kaplan S (2002) The incidence of congenital heart disease. J Am Coll Cardiol 39:1890–1900
Kemper AR, Mahle WT, Martin GR, Cooley WC, Kumar P, Morrow WR, Kelm K, Pearson GD, Glidewell J, Grosse SD, Howell RR et al (2011) Strategies for implementing screening for critical congenital heart disease. Pediatrics 128:e1259–e1267
Kluckow M, Evans N (2000) Superior vena cava flow in newborn infants: a novel marker of systemic blood flow. Arch Dis Child Fetal Neonatal Ed 82:F182–F187
Kroese JK, van Vonderen JJ, Narayen IC, Walther FJ, Hooper S, Te Pas AB (2015) The perfusion index of healthy term infants during transition at birth. Eur J Pediatr 175(4):475–479
Mellander M, Sunnegårdh J (2006) Failure to diagnose critical heart malformations in newborns before discharge—an increasing problem? Acta Paediatr 95:407–413
Mertens L, Seri I, Marek J, Arlettaz R, Braker P, McNamara P, Moon-Grady AJ, Coon PD, Noori S, Simpson J, Lai WW, Writing group of the American Society of Echocardiography (ASE), European Association of Echocardiography (EAE), Association for European Pediatric Cardiologists (AEPC) (2011) Targeted neonatal echocardiography in the neonatal intensive care unit: practice guidelines and recommendations for training. Eur J Echocardiogr 12:715–736
Patel N, Dodsworth M, Mills JF (2011) Cardiac output measurement in newborn infants using the ultrasonic cardiac output monitor: an assessment of agreement with conventional echocardiography, repeatability and new user experience. Arch Dis Child - Fetal Neonatal Ed 96:F206–F211. doi:10.1136/adc.2009.170704
Piasek CZ, Van Bel F, Sola A (2014) Perfusion index in newborn infants: a noninvasive tool for neonatal monitoring. Acta Paediatr 103:468–473
Singh A, Rasiah SV, Ewer AK (2014) The impact of routine predischarge pulse oximetry screening in a regional neonatal unit. Arch Dis Child Fetal Neonatal Ed 99(4):F297–F302
Sommers R, Stonestreet BS, Oh W, et al (2012) Hemodynamic Effects of Delayed Cord Clamping in Premature Infants. Pediatrics 129:e667–e672. doi:10.1542/peds.2011-2550
Takahashi S, Kakiuchi S, Nanba Y, Tsukamoto K, Nakamura T, Ito Y (2010) The perfusion index derived from a pulse oximeter for predicting low superior vena cava flow in very low birth weight infants. J Perinatol 30:265–269
Thangaratinam S, Brown K, Zamora J, et al (2012) Pulse oximetry screening for critical congenital heart defects in asymptomatic newborn babies: A systematic review and metaanalysis. Lancet. doi:10.1016/S0140-6736(12)60107-X
Vidal M, Ferragu F, Durand S, Baleine J, Batista-Novais AR, Cambonie G (2013) Perfusion index and its dynamic changes in preterm neonates with patent ductus arteriosus. Acta Paediatr 102:373–378
van Vonderen JJ, Pas te AB, Kolster-Bijdevaate C, van Lith JM, Blom NA, Hooper SB, Roest AA (2014) Non-invasive measurements of ductus arteriosus flow directly after birth. Arch Dis Child Fetal Neonatal Ed 99:F408–F412
Author information
Authors and Affiliations
Contributions
IC designed the study, performed the data collection and analysis, carried out the analyses, drafted the manuscript, and approved the final manuscript as submitted. AC and CC participated in data analysis, reviewed and revised the manuscript, and approved the final manuscript as submitted. CD participated to study design, supervised data collection and analysis, reviewed and revised the manuscript, and approved the final manuscript as submitted.
Corresponding author
Ethics declarations
Funding
This study was carried out without specific funding.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Additional information
Communicated by Patrick Van Reempts
The original version of this article was revised: The published version of the manuscript was not the revised version thus the changes were made in this article.
An erratum to this article is available at https://doi.org/10.1007/s00431-017-2939-3.
Rights and permissions
About this article
Cite this article
Corsini, I., Cecchi, A., Coviello, C. et al. Perfusion index and left ventricular output correlation in healthy term infants. Eur J Pediatr 176, 1013–1018 (2017). https://doi.org/10.1007/s00431-017-2920-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-017-2920-1