Abstract
Background
Although cut-off values used in high-resolution manometry (HRM) to diagnose esophageal motility disorders are based on representative samples of the US population and assume a supine position, differences in population and body positioning can reportedly affect results.
Aims
To establish normal HRM values for Thai people in both supine and upright positions.
Methods
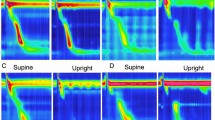
Forty-one healthy subjects were recruited, each of whom underwent solid-state HRM with ten 5-mL swallows of water in both the supine and upright positions. Measuring parameters according to the Chicago classification criteria (CC v3.0) were included, for which the mean, median and 5th and 95th percentiles (PCTLs) were calculated.
Results
The results corresponded with the CC v3.0 criteria, except for the mean, and 5th PCTL of the distal contractile integral (DCI), which were lower for this population. In the upright position, the mean and median values for DCI, intrabolus pressure and integrated relaxation pressure were significantly decreased, whereas the length of the transitional zone was significantly increased. The limitations of this study include: (1) the relatively low number of participants, (2) the limited recruitment of participants only at Ramathibodi Hospital and (3) the limited recruitment of only young and middle-aged participants.
Conclusions
We established normal values for the HRM parameters in a representative sample of the Thai population. Our supine results still prove that the use of the CC v3.0 is preferable. HRM testing in patients measured in the upright position should be analyzed based on the normative values obtained from upright swallow studies.
Similar content being viewed by others
References
Clouse RE, Staiano A, Alrakawi A. Development of a topographic analysis system for manometric studies in the gastrointestinal tract. Gastrointest Endosc. 1998;48:395–401.
Pandolfino JE, Fox MR, Bredenoord AJ, Kahrilas PJ. High-resolution manometry in clinical practice: utilizing pressure topography to classify oesophageal motility abnormalities. Neurogastroenterol Motil. 2009;21:796–806.
Kahrilas PJ, Bredenoord AJ, Fox M, et al. The Chicago classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil. 2015;27:160–174.
Ghosh SK, Pandolfino JE, Zhang Q, Jarosz A, Shah N, Kahrilas PJ. Quantifying esophageal peristalsis with high-resolution manometry: a study of 75 asymptomatic volunteers. Am J Physiol Gastrointest Liver Physiol. 2006;290:G988–G997.
Pandolfino JE, Ghosh SK, Zhang Q, Jarosz A, Shah N, Kahrilas PJ. Quantifying EGJ morphology and relaxation with high-resolution manometry: a study of 75 asymptomatic volunteers. Am J Physiol Gastrointest Liver Physiol. 2006;290:G1033–G1040.
Vega KJ, Langford-Legg T, Jamal MM. Ethnic variation in lower oesophageal sphincter pressure and length. Aliment Pharmacol Ther. 2008;28:655–659.
Xiang XL, Wang A, Tu L, et al. The motility of esophageal sphincters during liquid and solid bolus swallows: a multicenter normative value study of high-resolution manometry in China. Neurogastroenterol Motil. 2017. https://doi.org/10.1111/nmo.12914.
Sweis R, Anggiansah A, Wong T, Kaufman E, Obrecht S, Fox M. Normative values and inter-observer agreement for liquid and solid bolus swallows in upright and supine positions as assessed by esophageal high resolution manometry. Neurogastroenterol Motil. 2011;23:509-e198.
Xiao Y, Read A, Nicodeme F, Roman S, Kahrilas PJ, Pandolfino JE. The effect of a sitting vs supine posture on normative esophageal pressure topography metrics and Chicago classification diagnosis of esophageal motility disorders. Neurogastroenterol Motil. 2012;24:e509–e516.
Bernhard A, Pohl D, Fried M, Castell DO, Tutuian R. Influence of bolus consistency and position on esophageal high-resolution manometry findings. Dig Dis Sci. 2008;53:1198–1205.
Roman S, Damon H, Pellissier PE, Mion F. Does body position modify the results of oesophageal high resolution manometry? Neurogastroenterol Motil. 2010;22:271–275.
Zhang X, Xiang X, Tu L, Xie X, Hou X. Esophageal motility in the supine and upright positions for liquid and solid swallows through high-resolution manometry. J Neurogastroenterol Motil. 2013;19:467–472.
Pandolfino JE, El-Serag HB, Zhang Q, Shah N, Ghosh SK, Kahrilas PJ. Obesity: a challenge to esophagogastric junction integrity. Gastroenterology. 2006;130:639–649.
Garn SM, Smith NJ, Clark DC. Lifelong differences in hemoglobin levels between blacks and whites. J Natl Med Assoc. 1975;67:91–96.
Kraemer MJ, Hunter R, Rosse C, Smith NJ. Race-related differences in peripheral blood and bone marrow cell populations of American black and American white infants. J Natl Med Assoc. 1977;69:327–331.
Lee J, Anggiansah A, Anggiansah R, Young A, Wong T, Fox M. Effects of age on the gastroesophageal junction, esophageal motility, and reflux disease. Clin Gastroenterol Hepatol. 2007;5:1392–1398.
Clouse RE, Staiano A, Landau DW, Schlachter JL. Manometric findings during spontaneous chest pain in patients with presumed esophageal ‘‘spasms’’. Gastroenterology. 1983;85:395–402.
Bredenoord AJ, Fox M, Kahrilas PJ, et al. Chicago classification criteria of esophageal motility disorders defined in high resolution esophageal pressure topography. Neurogastroenterol Motil. 2012;24:57–65.
Niebisch S, Wilshire CL, Peters JH. Systematic analysis of esophageal pressure topography in high-resolution manometry of 68 normal volunteers. Dis Esophagus. 2013;26:651–660.
Kuribayashi S, Iwakiri K, Kawada A, et al. Variant parameter values-as defined by the Chicago Criteria-produced by ManoScan and a new system with Unisensor catheter. Neurogastroenterol Motil. 2015;27:188–194.
Weijenborg PW, Kessing BF, Smout AJ, Bredenoord AJ. Normal values for solid-state esophageal high-resolution manometry in a European population; an overview of all current metrics. Neurogastroenterol Motil. 2014;26:654–659.
Kwiatek MA, Mirza F, Kahrilas PJ, Pandolfino JE. Hyperdynamic upper esophageal sphincter pressure: a manometric observation in patients reporting globus sensation. Am J Gastroenterol. 2009;104:289–298.
Roman S, Lin Z, Pandolfino JE, Kahrilas PJ. Distal contraction latency: a measure of propagation velocity optimized for esophageal pressure topography studies. Am J Gastroenterol. 2011;106:443–451.
Xiao Y, Kahrilas PJ, Kwasny MJ, et al. High-resolution manometry correlates of ineffective esophageal motility. Am J Gastroenterol. 2012;107:1647–1654.
Shi Y, Xiao Y, Peng S, Lin J, Xiong L, Chen M. Normative data of high-resolution impedance manometry in the Chinese population. J Gastroenterol Hepatol. 2013;28:1611–1615.
Blonski W, Vela M, Safder A, Hila A, Castell DO. Revised criterion for diagnosis of ineffective esophageal motility is associated with more frequent dysphagia and greater bolus transit abnormalities. Am J Gastroenterol. 2008;103:699–704.
Ho SC, Chang CS, Wu CY, Chen GH. Ineffective esophageal motility is a primary motility disorder in gastroesophageal reflux disease. Dig Dis Sci. 2002;47:652–656.
Ravi K, Friesen L, Issaka R, Kahrilas PJ, Pandolfino JE. Long-term outcomes of patients with normal or minor motor function abnormalities detected by high-resolution esophageal manometry. Clin Gastroenterol Hepatol. 2015;13:1416–1423.
Kasamatsu S, Matsumura T, Ohta Y, et al. The effect of ineffective esophageal motility on gastroesophageal reflux disease. Digestion. 2017;95:221–228.
Ghosh SK, Pandolfino JE, Kwiatek MA, Kahrilas PJ. Oesophageal peristaltic transition zone defects: real but few and far between. Neurogastroenterol Motil. 2008;20:1283–1290.
Bogte A, Bredenoord AJ, Oors J, Siersema PD, Smout AJ. Normal values for esophageal high-resolution manometry. Neurogastroenterol Motil. 2013;25:762-e579.
Kessing BF, Weijenborg PW, Smout AJ, Hillenius S, Bredenoord AJ. Water-perfused esophageal high-resolution manometry: normal values and validation. Am J Physiol Gastrointest Liver Physiol. 2014;306:G491–G495.
Gao F, Gao Y, Hobson AR, Huang WN, Shang ZM. Normal esophageal high-resolution manometry and impedance values in the supine and sitting positions in the population of Northern China. Dis Esophagus. 2016;29:267–272.
Do Carmo GC, Jafari J, Sifrim D, de Oliveira RB. Normal esophageal pressure topography metrics for data derived from the Sandhill-Unisensor high-resolution manometry assembly in supine and sitting positions. Neurogastroenterol Motil. 2015;27:285–292.
Herregods TV, Roman S, Kahrilas PJ, Smout AJ, Bredenoord AJ. Normative values in esophageal high-resolution manometry. Neurogastroenterol Motil. 2015;27:175–187.
Nishimura N, Hongo M, Yamada M, et al. Effect of aging on the esophageal motor functions. J Smooth Muscle Res. 1996;32:43–50.
Grande L, Lacima G, Ros E, et al. Deterioration of esophageal motility with age: a manometric study of 79 healthy subjects. Am J Gastroenterol. 1999;94:1795–1801.
Clouse RE, Staiano A, Alrakawi A. Topographic analysis of esophageal double-peaked waves. Gastroenterology. 2000;118:469–476.
Sampath NJ, Bhargava V, Mittal RK. Genesis of multipeaked waves of the esophagus: repetitive contractions or motion artifact? Am J Physiol Gastrointest Liver Physiol. 2010;298:G927–G933.
Acknowledgments
The authors wish to thank Dr. Thanomnual Hiranyatheb, PhD, Faculty of Arts, Chulalongkorn University, for her kind assistance in revising the manuscript.
Funding
This research was supported by the Faculty of Medicine, Ramathibodi Hospital, Mahidol University.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare the total absence of any conflict of interest.
Rights and permissions
About this article
Cite this article
Hiranyatheb, P., Chakkaphak, S., Chirnaksorn, S. et al. Normal Values of High-Resolution Manometry in Supine and Upright Positions in a Thai Population. Dig Dis Sci 63, 173–183 (2018). https://doi.org/10.1007/s10620-017-4838-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-017-4838-x