Abstract
Background
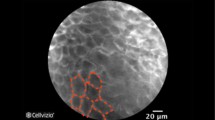
Probe-based confocal laser endomicroscopy (pCLE) is a new technique allowing in vivo detection of neoplastic tissue using a standard endoscope.
Aims
Our aim was to compare the incident dysplasia detection rate of biopsies obtained by high-definition white light endoscopy (HD-WLE) or by pCLE in a cohort of patients with Barrett’s esophagus (BE) participating in a surveillance program.
Methods
Fifty of 100 patients underwent pCLE in addition to HD-WLE. Four-quadrant biopsy specimens according to the Seattle biopsy protocol were obtained in all patients to ensure standard-of-care. Diagnosis of dysplasia/neoplasia was made by a blinded gastrointestinal pathologist.
Results
Incident high-grade dysplasia (HGD) and low-grade dysplasia (LGD) were diagnosed in 3/100 and in 16/100 cases. In the HD-WLE group, areas suspicious for neoplasia were not observed and dysplasia was diagnosed in 5/50 (10 %) patients (one with HGD). In the pCLE group, areas suspicious for neoplasia were observed by pCLE in 21/50 (42 %) patients; dysplasia was confirmed in 14 cases (28 %) (two with HGD). The dysplasia detection rate was significantly higher in the pCLE group than in the HD-WLE group (P = 0.04). The sensitivity, specificity, positive and negative predictive values of pCLE for dysplasia were 100, 83, 67, and 100 %, respectively.
Conclusions
Incident dysplasia can be more frequently detected by pCLE than by HD-WLE in BE. The higher dysplasia detection rate provided by pCLE could improve the efficacy of BE surveillance programs.



Similar content being viewed by others
References
Wang KK, Sampliner RE. Updated guidelines 2008 for the diagnosis, surveillance and therapy of Barrett’s esophagus. Am J Gastroenterol. 2008;103:788–797.
Prasad GA, Bansal A, Sharma P, et al. Predictors of progression in Barrett’s esophagus: current knowledge and future directions. Am J Gastroenterol. 2010;105:1490–1502.
American Gastroenterological Association medical position statement on the management of Barrett’s esophagus. Gastroenterology 2011;140:1084–1091.
Boyer J, Laugier R, Chemali M, et al. French Society of Digestive Endoscopy guideline: monitoring of patients with Barrett’s esophagus. Endoscopy. 2007;39:840–842.
Harrison R, Perry I, Haddadin W, et al. Detection of intestinal metaplasia in Barrett’s esophagus: an observational comparator study suggests the need for a minimum of eight biopsies. Am J Gastroenterol. 2007;102:1154–1161.
Abela JE, Going JJ, Mackenzie JF, et al. Systematic four-quadrant biopsy detects Barrett’s dysplasia in more patients than nonsystematic biopsy. Am J Gastroenterol. 2008;103:850–855.
Kariv R, Plesec TP, Goldblum JR, et al. The Seattle protocol does not more reliably predict the detection of cancer at the time of esophagectomy than a less intensive surveillance protocol. Clin Gastroenterol Hepatol. 2009;7:653–658.
Kiesslich R, Gossner L, Goetz M, et al. In vivo histology of Barrett’s esophagus and associated neoplasia by confocal laser endomicroscopy. Clin Gastroenterol Hepatol. 2006;4:979–987.
Dunbar KB, Okolo P, Montgomery E, Canto MI. Confocal laser endomicroscopy in Barrett’s esophagus and endoscopically inapparent Barrett’s neoplasia: a prospective, randomized, double-blind, controlled, crossover trial. Gastrointest Endosc. 2009;70:645–654.
Pohl H, Rosch T, Vieth M, et al. Miniprobe confocal laser microscopy for the detection of invisible neoplasia in patients with Barrett’s esophagus. Gut. 2008;57:1648–1653.
Wallace MB, Sharma P, Lightdale C, et al. Preliminary accuracy and interobserver agreement for the detection of intraepithelial neoplasia in Barrett’s esophagus with probe-based confocal laser endomicroscopy. Gastrointest Endosc. 2010;72:19–24.
Bajbouj M, Vieth M, Rosch T, et al. Probe-based confocal laser endomicroscopy compared with standard four-quadrant biopsy for evaluation of neoplasia in Barrett’s esophagus. Endoscopy. 2010;42:435–440.
Frazzoni M, Savarino E, Manno M, et al. Reflux patterns in patients with short segment Barrett’s oesophagus: a study using impedance-pH monitoring off and on proton pump inhibitor therapy. Aliment Pharmacol Ther. 2009;30:508–515.
Lundell LR, Dent J, Bennett JR, et al. Endoscopic assessment of oesophagitis: clinical and functional correlates and further validation of the Los Angeles classification. Gut. 1999;45:172–180.
Sharma P, Dent J, Armstrong D, et al. The development and validation of an endoscopic grading system for Barrett’s esophagus: the Prague C & M criteria. Gastroenterology. 2006;131:1392–1399.
Wallace M, Lauwers GY, Chen Y, et al. Miami classification for probe-based confocal laser endomicroscopy. Endoscopy. 2011;43:882–891.
Haggitt RC. Barrett’s esophagus, dysplasia, and adenocarcinoma. Hum Pathol. 1994;25:982–993.
Montgomery E, Bronner MP, Goldblum JR, et al. Reproducibility of the diagnosis of dysplasia in Barrett esophagus: a reaffirmation. Hum Pathol. 2001;32:368–378.
Spechler SJ, Sharma P, Souza RF, et al. American Gastroenterological Association technical review on the management of Barrett’s esophagus. Gastroenterology. 2011;140:e18–e52.
Sharma P, Meining A, Coron E, et al. Real-time increased detection of neoplastic tissue in Barrett’s esophagus with probe-based confocal laser endomicroscopy: final results of an international multicenter, prospective, randomized, controlled trial. Gastrointest Endosc. 2011;74:465–472.
Ronkainen J, Aro P, Storskrubb T, et al. Prevalence of Barrett’s esophagus in the general population: an endoscopic study. Gastroenterology. 2005;129:1825–1831.
Zagari RM, Fuccio L, Wallander M-A, et al. Gastro-oesophageal reflux symptoms, oesophagitis and Barrett’s oesophagus in the general population: the Loiano–Monghidoro study. Gut. 2008;57:1354–1359.
Iftikhar SY, James PD, Steele RJ, et al. Length of Barrett’s oesophagus: an important factor in the development of dysplasia and adenocarcinoma. Gut. 1992;33:1155–1158.
Wolfsen HC, Hemminger LL, Wallace MB, et al. Clinical experience of patients undergoing photodynamic therapy for Barrett’s dysplasia or cancer. Aliment Pharmacol Ther. 2004;20:1125–1131.
Wani S, Falk JW, Hall M, et al. Patients with nondysplastic Barrett’s esophagus have low risks for developing dysplasia or esophageal adenocarcinoma. Clin Gastroenterol Hepatol. 2011;9:220–227.
Sikkema M, Looman CWN, Steyerberg EW, et al. Predictors for neoplastic progression in patients with Barrett’ s esophagus: a prospective cohort study. Am J Gastroenterol. 2011;106:1231–1238.
Lim CH, Treanor D, Dixon MF, et al. Low grade dysplasia in Barrett’s esophagus has a high risk of progression. Endoscopy. 2007;39:581–587.
Curvers WL, Kate FJ, Krishnadath KK, et al. Low-grade dysplasia in Barrett’s esophagus: overdiagnosed and underestimated. Am J Gastroenterol. 2010;105:1523–1530.
Wani S, Falk JW, Post J, et al. Risk factors for progression of low-grade dysplasia in patients with Barrett’s esophagus. Gastroenterology. 2011;141:1179–1186.
Hvid-Jensen F, Pedersen L, Mohr Drewes A, et al. Incidence of adenocarcinoma among patients with Barrett’s esophagus. N Engl J Med. 2011;365:1375–1383.
Acknowledgments
This study was conducted without any financial support.
Conflict of interest
The authors certify that there is no conflict of interest with any financial organization regarding the material discussed in the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bertani, H., Frazzoni, M., Dabizzi, E. et al. Improved Detection of Incident Dysplasia by Probe-Based Confocal Laser Endomicroscopy in a Barrett’s Esophagus Surveillance Program. Dig Dis Sci 58, 188–193 (2013). https://doi.org/10.1007/s10620-012-2332-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-012-2332-z