Abstract
Background
Pink urine syndrome (PUS) is attributed to the precipitation of uric acid caused by low urinary pH (U-pH). However, the reasons for the lower U-pH are unclear.
Objectives
To investigate the occurrence of PUS and verified the cause of U-pH reduction.
Methods
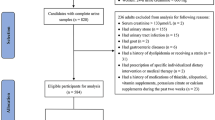
Participants comprised 4,940 students who had undergone a physical examination. Data on the presence [PUS (+)] or absence [PUS (−)] of PUS, as well as age, gender, body mass index (BMI), blood pressure (BP), heart rate (HR), and U-pH were collected. Of these participants, 300 randomly selected individuals were evaluated for their waist circumference, as well as their levels of urinary C-peptide, angiotensinogen, methylglyoxal, thiobarbituric acid-reactive substances (TBARS), and Na+ excretion. Independent risk factors of lower U-pH were decided by a multiple-regression analysis.
Results
PUS was observed in 216 students (4.4 %). A greater number of men comprised the PUS (+) group compared with the PUS (−) group, and subjects in this group had high BMI, BP, and HR values, as well as low U-pH. A logistic regression analysis revealed that the BMI and U-pH were independent risk factors for PUS (+). The decrease of U-pH was closely related to the progress of chronic kidney disease (CKD). BMI value was related to PUS (+) in the CKD (−) subjects. On the other hand, low U-pH was related to PUS (+) in the CKD (+) subjects. All factors other than HR showed a significant negative correlation with U-pH. However, multiple-regression analysis revealed that TBARS and angiotensinogen were independent risk factors.
Conclusion
Obesity and lower U-pH were each independently related to PUS, whereas increased intrarenal oxidative stress and exacerbation of the renin–angiotensin system activation were associated with the lowering of U-pH. U-pH low value is related to potential CKD.


Similar content being viewed by others
Abbreviations
- PUS:
-
Pink urine syndrome
- BMI:
-
Body mass index
- U-pH:
-
Urinary pH
- SBP:
-
Systolic blood pressure
- DBP:
-
Diastolic blood pressure
- HR:
-
Heart rate
- RAS:
-
Renin–angiotensin system
- ROS:
-
Reactive oxygen species
- TBARS:
-
Thiobarbituric acid-reactive substances
- NHE:
-
Na+–H+ exchanger
- CKD:
-
Chronic kidney disease
- Cre:
-
Creatinine
References
Deitel M, Thompson DA, Saldanha CF, Ramshaw PJ, Patterson MC, Pritzker KP. “Pink urine” in morbidly obese patients following gastric partitioning. Can Med Assoc J. 1984;130:1007–11.
Saran R, Abdullah S, Goel S, Nolph KD, Terry BE. An unusual cause of pink urine. Nephrol Dial Transpl. 1998;13:1579–80.
Scialla JJ, Anderson CA. Dietary acid load: a novel nutritional target in chronic kidney disease? Adv Chronic Kidney Dis. 2013;20:141–9.
Adeva MM, Souto G. Diet-induced metabolic acidosis. Clin Nutr. 2011;30:416–21.
Miyazawa N, Abe M, Souma T, Tanemoto M, Abe T, Nakayama M, Ito S. Methylglyoxal augments intracellular oxidative stress in human aortic endothelial cells. Free Radic Res. 2010;44:101–7.
Gaens KH, Stehouwer CD, Schalkwijk CG. Advanced glycation endproducts and its receptor for advanced glycation endproducts in obesity. Curr Opin Lipidol. 2013;24:4–11.
Ogawa S, Kobori H, Ohashi N, Urushihara M, Nishiyama A, Mori T, Ishizuka T, Nako K, Ito S. Angiotensin II type 1 receptor blockers reduce urinary angiotensinogen excretion and the levels of urinary markers of oxidative stress and inflammation in patients with Type 2 diabetic nephropathy. Biomark Insights. 2009;4:97–102.
Dhar I, Dhar A, Wu L, Desai KM. Increased methylglyoxal formation with upregulation of renin angiotensin system in fructose fed Sprague Dawley rats. PLoS One. 2013;8:e74212.
Tanaka T, Okamura T, Miura K, Kadowaki T, Ueshima H, Nakagawa H, Hashimoto T. A simple method to estimate populational 24-h urinary sodium and potassium excretion using a casual urine specimen. J Hum Hypertens. 2002;16:97–103.
Azuma K, Minami Y, Ippoushi K, Terao J. Lowering effects of onion intake on oxidative stress biomarkers in streptozotocin-induced diabetic rats. J Clin Biochem Nutr. 2007;40:131–40.
Ogawa S, Nakayama K, Nakayama M, Mori T, Matsushima M, Okamura M, Senda M, Nako K, Miyata T, Ito S. Methylglyoxal is a predictor in type 2 diabetic patients of intima-media thickening and elevation of blood pressure. Hypertension. 2010;56:471–6.
Zuckerman JM, Assimos DG. Hypocitraturia: pathophysiology and medical management. Rev Urol. 2009;11:134–44.
Krupp D, Shi L, Remer T. Longitudinal relationships between diet-dependent renal acid load and blood pressure development in healthy children. Kidney Int. 2014;85:204–10.
Goraya N, Simoni J, Jo CH, Wesson DE. A comparison of treating metabolic acidosis in CKD stage 4 hypertensive kidney disease with fruits and vegetables or sodium bicarbonate. Clin J Am Soc Nephrol. 2013;8:371–81.
Mandel EI, Taylor EN, Curhan GC. Dietary and lifestyle factors and medical conditions associated with urinary citrate excretion. Clin J Am Soc Nephrol. 2013;8:901–8.
Otsuki M, Kitamura T, Goya K, Saito H, Mukai M, Kasayama S, Shimomura I, Koga M. Association of urine acidification with visceral obesity and the metabolic syndrome. Endocr J. 2011;58:363–7.
Archibeque SL, Freetly HC, Cole NA, Ferrell CL. The influence of oscillating dietary protein concentrations on finishing cattle. II. Nutrient retention and ammonia emissions. J Anim Sci. 2007;85:1496–503.
Odunewu A, Fliegel L. Acidosis-mediated regulation of the NHE1 isoform of the Na+/H+ exchanger in renal cells. Am J Physiol Ren Physiol. 2013;305:F370–81.
Odani H, Shinzato T, Matsumoto Y, Usami J, Maeda K. Increase in three alpha, beta-dicarbonyl compound levels in human uremic plasma: specific in vivo determination of intermediates in advanced Maillard reaction. Biochem Biophys Res Commun. 1999;256:89–93.
Chang T, Wu L. Methylglyoxal, oxidative stress, and hypertension. Can J Physiol Pharmacol. 2006;84:1229–38.
Guo Q, Mori T, Jiang Y, Hu C, Osaki Y, Yoneki Y, Sun Y, Hosoya T, Kawamata A, Ogawa S, Nakayama M, Miyata T, Ito S. Methylglyoxal contributes to the development of insulin resistance and salt sensitivity in Sprague-Dawley rats. J Hypertens. 2009;27:1664–71.
Wang X, Jia X, Chang T, Desai K, Wu L. Attenuation of hypertension development by scavenging methylglyoxal in fructose-treated rats. J Hypertens. 2008;26:765–72.
Gekle M, Knaus P, Nielsen R, Mildenberger S, Freudinger R, Wohlfarth V, Sauvant C, Christensen EI. Transforming growth factor-beta1 reduces megalin- and cubilin-mediated endocytosis of albumin in proximal-tubule-derived opossum kidney cells. J Physiol. 2003;552:471–81.
Yamagishi S, Inagaki Y, Okamoto T, Amano S, Koga K, Takeuchi M. Advanced glycation end products inhibit de novo protein synthesis and induce TGF-beta overexpression in proximal tubular cells. Kidney Int. 2003;63:464–73.
Saito A, Takeda T, Sato K, Hama H, Tanuma A, Kaseda R, Suzuki Y, Gejyo F. Significance of proximal tubular metabolism of advanced glycation end products in kidney diseases. Ann NY Acad Sci. 2005;1043:637–43.
Ozdemir AM, Hopfer U, Rosca MV, Fan XJ, Monnier VM, Weiss MF. Effects of advanced glycation end product modification on proximal tubule epithelial cell processing of albumin. Am J Nephrol. 2008;28:14–24.
Biemesderfer D, Nagy T, DeGray B, Aronson PS. Specific association of megalin and the Na+/H+ exchanger isoform NHE3 in the proximal tubule. J Biol Chem. 1999;274:17518–24.
Li XC, Hopfer U, Zhuo JL. AT1 receptor-mediated uptake of angiotensin II and NHE-3 expression in proximal tubule cells through a microtubule-dependent endocytic pathway. Am J Physiol Ren Physiol. 2009;297:F1342–52.
Hosojima M, Sato H, Yamamoto K, Kaseda R, Soma T, Kobayashi A, Suzuki A, Kabasawa H, Takeyama A, Ikuyama K, Iino N, Nishiyama A, Thekkumkara TJ, Takeda T, Suzuki Y, Gejyo F, Saito A. Regulation of megalin expression in cultured proximal tubule cells by angiotensin II type 1A receptor- and insulin-mediated signaling cross talk. Endocrinology. 2009;150:871–8.
Acknowledgments
The authors acknowledge the editorial assistance and clinical support of Miss Manami Shimizu for her help with preparing the references and for her expert assistance in the preparation of the tables and figures. The authors wish to thank Miss Manami Shimizu, Miss Asako Chiba and Mrs. Yasuko Sato for their assistance with gathering the urine samples for the study. We also wish to thank nurses Eiko Mitsui, Yoko Hasegawa, Michiko Ota, Megumi Ito and Hiromi Sato for their efforts in gathering student data. This work was supported by a 21st Century Center of Excellence Program Special Research Grant from the Ministry of Education, Sports and Culture, and Tohoku University’s Center for the Advancement of Higher Education President’s Research Fund.
Conflict of interest
All authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Ogawa, S., Takiguchi, J., Nako, K. et al. Elucidation of the etiology and characteristics of pink urine in young healthy subjects. Clin Exp Nephrol 19, 822–829 (2015). https://doi.org/10.1007/s10157-014-1066-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-014-1066-y