Abstract
Background
Chronic pain may be a long-term problem related to operative trauma and mesh material in Lichtenstein hernioplasty.
Study design
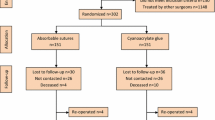
Inguinal hernioplasty was performed under local anesthesia in 228 patients (232 hernias) in day-case surgery by the same surgeon and exactly by the same surgical technique. The patients were randomized to receive either a partly absorbable polypropylene–polyglactin mesh (Vypro IIR 50 g/m2, 79 hernias), a lightweight polypropylene mesh (Premilene Mesh LPR 55 g/m2, 75 hernias) or a conventional densely woven polypropylene mesh (PremileneR 82 g/m2, 78 hernias). Pain, patients discomfort and recurrences of hernias were carefully followed at days 1, 7, 1 month, 1 and 2 years after surgery.
Results
The duration of operation (29–33 min) and the amount of local anesthetic (55–57 ml) were similar in the three groups. Two wound infections and four hematomas were detected with no difference between the meshes. Immediate pain reaction up to 1 month was statistically equal among the three meshes. After 2 years of follow-up, there were five recurrences (two in the Vypro group, one in the Premilene LP and two in the Premilene). A feeling of a foreign body, sensation of pain and patient’s discomfort were similar with all meshes.
Conclusion
There was no difference of pain and quality of life among a conventional polypropylene mesh, lightweight mesh or partly absorbable mesh in 2 years of follow-up, when the same surgeon operated on all patients with exactly the same technique.

Similar content being viewed by others
References
Heikkinen TJ (1998) Costs and early outcome of laparoscopic and open operation in three common surgical conditions. Doctoral Thesis, University of Oulu, Finland
Cheek CM, Black NA, Devlin HB (1998) Groin hernia surgery: a systematic review. Ann R Coll Surg Engl 80(Suppl 1):S1–S20
Rutkow IM (2003) Demographic and socioeconomic aspects of hernia repair in the United States in 2003. Surg Clin NA 83:1045–52
Callesen T, Bech K, Kehlet H (1999) Prospective study of chronic pain after groin hernia repair. Br J Surg 86:1528–31
Bay-Nielsen M, Perkins FM, Kehlet H (2001) Pain and functional impairment 1 year after inguinal herniorraphy: a nationwide questionnaire study. Ann Surg 233:1–7
Poobalan AS, Bruce J, King PM (2001) Chronic pain and quality of life following open inguinal hernia repair. Br J Surg 88:1122–26
Heise CP, Starling JR. (1998) Mesh inguinodynia: a new clinical syndrome after inguinal herniorraphy?. J Am Coll Surg 187:514–518
Di Vita G, Milano S, Frazzetta M (2000) Tension-free hernia repair is associated with an increase in inflammatory response markers against the mesh. Am J Surg 180:203–207
Nahabedian MY, Dellon AL (1997) Outcome of the operative management of nerve injuries in the ilioinguinal region. J Am Coll Surg 184:265–268
Morris-Stiff GJ, Hughes LE (1998) The outcomes of nonabsorbable mesh placed within the abdominal cavity: literature review and clinical experience. Am Coll Surg 186:352–367
Stulz P, Pfeiffer KM (1982) Peripheral nerve injuries resulting from common surgical procedures in the lower portion of the abdomen. Arch Surg 117:324–327
Grant A, Hernia EU (2000) Trialists collaboration mesh compared with non-mesh methods of open groin hernia repair: systematic review of randomized controlled trials. Br J Surg 87:854–859
Lichtenstein IL, Shulman AG, Amid PK, Montllor MM (1989) The tension-free hernioplasty. Am J Surg 157:188–193
Amid PK, Shulman AG, Lichtenstein IL (1996) Open “tension-free” repair of inguinal hernias: the Lichtenstein technique. Eur J Surg 162:447–453
Bay-Nielsen M, Kehlet H, Strand L (2001) Quality assessment of 26,304 herniorraphies in Denmark: a prospective nationwide study. Lancet 358:1124–1128
O’Dwyer PJ, Kingsnorth AN, Molloy RG, Small PK, Lammers B, Horeyseck G (2005) Randomized clinical trial assessing impact of a lightweight or heavyweight mesh on chronic pain after inguinal hernia repair. Br J Surg 92:166–170
Bringman S, Wollert S, Osterberg J, Smedberg S, Granlund H, Heikkinen T (2006) Three-year results of a randomized clinical trial of lightweight or standard polypropylene mesh in Lichtenstein repair of primary inguinal hernia. Br J Surg 96:1056–1059
Nienhuijs SW, van Oort I, Keemers-Gels ME, Strobbe LJ, Rosman C (2005) Randomized trial comparing the prolene hernia system, mesh plug repair and Lichtenstein method for open inguinal hernia repair. Br J Surg 92:33–38
Post S, Weiss B, Willer M, Neufang T, Lorenz D (2004) Randomized clinical trial of lightweight composite mesh for Lichtenstein inguinal hernia repair. Br J Surg 91:44–8
Paajanen H (2001) Lichtenstein inguinal herniorraphy under local infiltration anaestesia as rapid outpatient procedure. Ann Chir Gyn 90:51–54
Paajanen H (2003) Groin hernia repair under local anaesthesia: effect of surgeon’s training level on long-term results. J Ambulatory Surg 10:143–146
Finley RK, Miller SF, Jones LM (1999) Elimination of urinary retention following inguinal herniorraphy. Am Surg 57:486–488
Horstmann R, Hellwig M, Classen C, Röttgermann S, Palmes D (2006) Impact of polypropylene amount on functional outcome and quality of life after inguinal hernia repair by the TAPP procedure using pure, mixed, and titanium-coated meshes. World J Surg 30:1742–1749
Amid PK (2004) Causes, prevention, and surgical treatment of postherniorraphy neuropathic inguinodynia: triple neurectomy with proximal end implantation. Hernia 8:343–349
Franneby U, Sandblom G, Nordin P, Nyren O, Gunnarsson U (2006) Risk factors for long-term pain after hernia surgery. Ann Surg 244:212–219
Acknowledgments
The technical assistance of Mrs. Tellervo Summanen (technical assistance and Mrs. Pirjo Halonen (biostatistical analysis) are greatly appreciated. I thank Mrs. Lisa Kivela for revising the English. The experiments comply with the current laws of Finland.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Paajanen, H. A single-surgeon randomized trial comparing three composite meshes on chronic pain after Lichtenstein hernia repair in local anesthesia. Hernia 11, 335–339 (2007). https://doi.org/10.1007/s10029-007-0236-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-007-0236-1