Abstract
Background
Intraoperative magnetic resonance imaging (iMRI) is proven to be advantageous in transsphenoidal surgery (TSS) for pituitary adenomas. We evaluated the efficacy of low-field iMRI. Also, we described several techniques to enhance the visibility of the tumor resection margin.
Methods
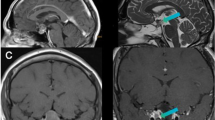
Two hundred twenty-nine patients who underwent TSS using low-field iMRI were analyzed. iMRI was acquired in cases where the tumor removal was thought to meet the surgical goal after the tumor resection cavity had been packed with contrast-soaked cotton pledgets to improve the visibility of the tumor resection margin. Suspicious remnants were localized and explored using updated iMRI-based semi-real-time navigation. A merging technique was adopted for very small tumors. The final outcome was evaluated using postoperative 3-T diagnostic magnetic resonance imaging (MRI).
Results
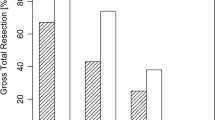
Among 198 patients in whom total resection was attempted, total resection seemed to have been achieved in 184 patients based on iMRI findings. However, immediate postoperative MRI revealed remnant tumors in 4 out of 184 patients (false-negative rate, 2.2 %). The other 31 patients underwent intended subtotal resection of the tumors. Overall, in 47 patients (20.5 %), the use of iMRI led to further resection. Those patients benefited from the use of iMRI to achieve the planned extent of tumor resection.
Conclusions
iMRI maximizes the extent of resection and minimizes the possibility of unexpected tumor remnants in TSS for pituitary adenomas. It is essential to reduce imaging artifacts and enhance the visibility of the tumor resection margin during the use of low-field iMRI.





Similar content being viewed by others
References
Ahn JY, Jung JY, Kim J, Lee KS, Kim SH (2008) How to overcome the limitations to determine the resection margin of pituitary tumours with low-field intra-operative MRI during trans-sphenoidal surgery: usefulness of Gadolinium-soaked cotton pledgets. Acta Neurochir (Wien) 150:763–771
Baumann F, Schmid C, Bernays R (2010) Intraoperative magnetic resonance imaging-guided transsphenoidal surgery for giant pituitary adenomas. Neurosurg Rev 33:83–90
Bellut D, Hlavica M, Schmid C, Bernays R (2010) Intraoperative magnetic resonance imaging-assisted transsphenoidal pituitary surgery in patients with acromegaly. Neurosurg Focus 29:E9
Bohinski RJ, Warnick RE, Gaskill-Shipley MF, Zuccarello M, van Loveren HR, Kormos DW, Tew JM (2001) Intraoperative magnetic resonance imaging to determine the extent of resection of pituitary macroadenomas during transsphenoidal microsurgery. Neurosurgery 49:1133–1143
Bradley W (2002) Achieving gross total resection of brain tumors: Intraoperative MR imaging can make a big difference. AJNR Am J Neuroradiol 23:348–349
Claus E, Horlacher A, Hsu L, Schwartz R, Dellolacono D, Talos F, Jolesz F, Black P (2005) Survival rates in patients with low grade glioma after intraoperative magnetic resonance image guidance. Cancer 103:1227–1233
De Witte O, Makiese O, Wikler D, Levivier M, Vandensteene A, Pandin P, Baleriaux D, Brotchi J (2005) Transsphenoidal approach with low field MRI for pituitary adenoma. Neurochirurgie 51:577–583
Fahlbusch R, Ganslandt O, Buchfelder M, Schott W, Nimsky C (2001) Intraoperative magnetic resonance imaging during transsphenoidal surgery. J Neurosurg 95:381–390
Fahlbusch R, Keller B, Ganslandt O, Kreutzer J, Nimsky C (2005) Transsphenoidal surgery in acromegaly investigated by intraoperative high-field magnetic resonance imaging. Eur J Endocrinol 153:239–248
Gering D, Nabavi A, Kikinis R, Hata N, O’Donnell L, Grimson E, Jolesz F, Black P, Wells W (2001) An integrated visualization system for surgical planning and guidance using image fusion and an open MR. J Magn Reson Imaging 13:967–975
Gerlach R, Rochemont R, Gasser T, Marquardt G, Imoehl L, Seifert V (2011) Implementation of the ultra low field intraoperative MRI PoleStar N20 during resection control of pituitary adenomas. Acta Neurochir Suppl 109:73–79
Jane J Jr, Laws E Jr (2010) Endoscopy versus MR imaging. J Neurosurg Pediatr 112:734–735
Lee E, Ahn J, Noh T, Kim S, Kim T (2009) Tumor tissue identification in the pseudocapsule of pituitary adenoma: should the pseudocapsule be removed for total resection of pituitary adenoma? Neurosurgery 64:62–69
Nimsky C, Ganslandt O, Fahlbusch R (2005) Comparing 0.2 Tesla with 1.5 Tesla intraoperative magnetic resonance imaging analysis of setup, workflow, and efficiency. Acad Radiol 12:1065–1079
Nimsky C, Ganslandt O, Keller B, Fahlbusch R (2003) Preliminary experience in glioma surgery with intraoperative high-field MRI. Acta Neurochir Suppl 88:21–29
Nimsky C, Ganslandt O, Tomandl B, Buchfelder M, Fahlbusch R (2002) Low-field magnetic resonance imaging for intraoperative use in neurosurgery: a 5-year experience. Eur Radiol 12:2690–2703
Nimsky C, von Keller B, Ganslandt O, Fahlbusch R (2006) Intraoperative high-field magnetic resonance imaging in transsphenoidal surgery of hormonally inactive pituitary macroadenomas. Neurosurgery 59:105–114
Onizuka M, Tokunaga Y, Shibayama A, Miyazaki H (2001) Computer-assisted neurosurgical navigational system for transsphenoidal surgery. Neurol Med Chir (Tokyo) 41:565–569
Pergolizzi R Jr, Nabavi A, Schwartz R, Hsu L, Wong T, Martin C, Black P, Jolesz F (2001) Intra-operative MR guidance during trans-sphenoidal pituitary resection: preliminary results. J Magn Reson Imaging 13:136–141
Schneider J, Trantakis C, Rubach M, Schulz T, Dietrich J, Winkler D, Renner C, Schober R, Geiger K, Brosteanu O (2005) Intraoperative MRI to guide the resection of primary supratentorial glioblastoma multiforme—a quantitative radiological analysis. Neuroradiology 47:489–500
Schulder M, Carmel P (2003) Intraoperative magnetic resonance imaging: impact on brain tumor surgery. Cancer Control 10:115–124
Senft C, Seifert V, Hermann E, Franz K, Gasser T (2008) Usefulness of intraoperative ultra low-field magnetic resonance imaging in glioma surgery. Neurosurgery 63:257–267
Wolfsberger S, Ba Ssalamah A, Pinker K, Mlynarik V, Czech T, Knosp E, Trattnig S (2004) Application of three-tesla magnetic resonance imaging for diagnosis and surgery of sellar lesions. J Neurosurg 100:278–286
Wu J, Shou X, Yao C, Wang Y, Zhuang D, Mao Y, Li S, Zhou L (2009) Transsphenoidal pituitary macroadenomas resection guided by PoleStar N20 low-field intraoperative magnetic resonance imaging: comparison with early postoperative high-field magnetic resonance imaging. Neurosurgery 65:63–71
Acknowledgments
The authors appreciate Mr. Dong Su Jang, a medical illustrator, for his beautiful work on the figures in this paper.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Comment
Dr. Kim and colleagues have reviewed a large series of patients with pituitary ademonas in whom they used low-field intraoperative magnetic resonance imaging to monitor tumor removal. They found that when checking the scan after surgery to attempt complete removal, a small percentage of patients had not achieved complete resection (2/2 % false-negative rate). Furthermore, they used the results of the scan to extend the resection in over 20 % of patients (including those with subtotal resections). When reviewing this latter number, one questions whether the initial surgery would have been more aggressive if the MRI had not been available. However, given the number of patients analyzed and the surgeons' experience, this study will represent the gold standard for reference. It will make a great addition to the literature.
William Couldwell
USA
Rights and permissions
About this article
Cite this article
Kim, E.H., Oh, M.C. & Kim, S.H. Application of low-field intraoperative magnetic resonance imaging in transsphenoidal surgery for pituitary adenomas: technical points to improve the visibility of the tumor resection margin. Acta Neurochir 155, 485–493 (2013). https://doi.org/10.1007/s00701-012-1608-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-012-1608-6