Abstract
Study design
Prospective longitudinal study.
Objective
To determine whether systemic cytokines and C-reactive protein (CRP) during an acute episode of low back pain (LBP) differ between individuals who did and did not recover by 6 months and to identify sub-groups based on patterns of inflammatory, psychological, and sleep features associated with recovery/non-recovery.
Summary of background data
Systemic inflammation is observed in chronic LBP and may contribute to the transition from acute to persistent LBP. Longitudinal studies are required to determine whether changes present early or develop over time. Psychological and/or sleep-related factors may be related.
Methods
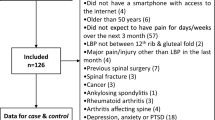
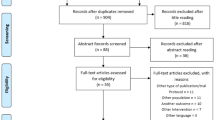
Individuals within 2 weeks of onset of acute LBP (N = 109) and pain-free controls (N = 55) provided blood for assessment of CRP, tumor necrosis factor (TNF), interleukin-6 (IL-6) and interleukin-1β, and completed questionnaires related to pain, disability, sleep, and psychological status. LBP participants repeated measurements at 6 months. Biomarkers were compared between LBP and control participants at baseline, and in longitudinal (baseline/6 months) analysis, between unrecovered (≥pain and disability), partially recovered (reduced pain and/or disability) and recovered (no pain and disability) participants at 6 months. We assessed baseline patterns of inflammatory, psychological, sleep, and pain data using hierarchical clustering and related the clusters to recovery (% change in pain) at 6 months.
Results
CRP was higher in acute LBP than controls at baseline. In LBP, baseline CRP was higher in the recovered than non-recovered groups. Conversely, TNF was higher at both time-points in the non-recovered than recovered groups. Two sub-groups were identified that associated with more (“inflammatory/poor sleep”) or less (“high TNF/depression”) recovery.
Conclusions
This is the first evidence of a relationship between an “acute-phase” systemic inflammatory response and recovery at 6 months. High inflammation (CRP/IL-6) was associated with good recovery, but specific elevation of TNF, along with depressive symptoms, was associated with bad recovery. Depression and TNF may have a two-way relationship.
Graphical abstract
These slides can be retrieved under Electronic Supplementary Material.




Similar content being viewed by others
References
Wang H, Schiltenwolf M, Buchner M (2008) The role of TNF-alpha in patients with chronic low back pain-a prospective comparative longitudinal study. Clin J Pain 24(3):273–278
Wang H, Ahrens C, Rief W, Gantz S, Schiltenwolf M, Richter W (2010) Influence of depression symptoms on serum tumor necrosis factor-alpha of patients with chronic low back pain. Arthritis Res Ther 12(5):R186
Carp SJ, Barbe MF, Winter KA, Amin M, Barr AE (2007) Inflammatory biomarkers increase with severity of upper-extremity overuse disorders. Clin Sci (Lond) 112(5):305–314
Parkitny L, McAuley JH, Di Pietro F, Stanton TR, O’Connell NE, Marinus J, van Hilten JJ, Moseley GL (2013) Inflammation in complex regional pain syndrome A systematic review and meta-analysis. Neurology 80(1):106–117
Della Vedova C, Cathcart S, Dohnalek A, Lee V, Hutchinson MR, Immink MA, Hayball J (2013) Peripheral interleukin-1B levels are elevated in chronic tension-type headache patients. Pain Res Manag 18(6):301–306
Hernandez ME, Becerril E, Perez M, Leff P, Anton B, Estrada S, Estrada I, Sarasa M, Serrano E, Pavon L (2010) Proinflammatory cytokine levels in fibromyalgia patients are independent of body mass index. BMC Res Notes 3(1):156
Shimura Y, Kurosawa H, Sugawara Y, Tsuchiya M, Sawa M, Kaneko H, Futami I, Liu L, Sadatsuki R, Hada S, Iwase Y, Kaneko K, Ishijima M (2013) The factors associated with pain severity in patients with knee osteoarthritis vary according to the radiographic disease severity: a cross-sectional study. Osteoarthr Cartilage 21(9):1179–1184
Asanuma Y, Oeser A, Stanley E, Bailey DG, Shintani A, Stein CM (2008) Effects of C-reactive protein and homocysteine on cytokine production: modulation by pravastatin. Arch Drug Inf 1(1):14–22
Moshage HJ, Roelofs HMJ, Vanpelt JF, Hazenberg BPC, Vanleeuwen MA, Limburg PC, Aarden LA, Yap SH (1988) The effect of interleukin-1, interleukin-6 and its interrelationship on the synthesis of serum amyloid a-reactive and C-reactive protein in primary cultures of adult human hepatocytes. Biochem Bioph Res Co 155(1):112–117
Anty R, Bekri S, Luciani N, Saint-Paul MC, Dahman M, Iannelli A, Ben Amor I, Staccini-Myx A, Huet PM, Gugenheim J, Sadoul JL, Le Marchand-Brustel Y, Tran A, Gual P (2006) The inflammatory C-reactive protein is increased in both liver and adipose tissue in severely obese patients independently from metabolic syndrome, type 2 diabetes, and NASH. Am J Gastroenterol 101(8):1824–1833
Koch A, Zacharowski K, Boehm O, Stevens M, Lipfert P, von Giesen HJ, Wolf A, Freynhagen R (2007) Nitric oxide and pro-inflammatory cytokines correlate with pain intensity in chronic pain patients. Inflamm Res 56(1):32–37
Mukai E, Nagashima M, Hirano D, Yoshino S (2000) Comparative study of symptoms and neuroendocrine-immune network mediator levels between rheumatoid arthritis patients and healthy subjects. Clin Exp Rheumatol 18(5):585–590
Rannou F, Ouanes W, Boutron I, Lovisi B, Fayad F, Mace Y, Borderie D, Guerini H, Poiraudeau S, Revel M (2007) High-sensitivity C-reactive protein in chronic low pack pain with vertebral end-plate modic signal changes. Arthrit Rheum-Arthr 57(7):1311–1315
Edwards RR, Calahan C, Mensing G, Smith M, Haythornthwaite JA (2011) Pain, catastrophizing, and depression in the rheumatic diseases. Nat Rev Rheumatol 7(4):216–224
Mullington JM, Simpson NS, Meier-Ewert HK, Haack M (2010) Sleep loss and inflammation. Best Pract Res Cl En 24(5):775–784
Okifuji A, Hare BD (2015) The association between chronic pain and obesity. J Pain Res 8:399–408
Kelly GA, Blake C, Power CK, O’Keeffe D, Fullen BM (2011) The association between chronic low back pain and sleep a systematic review. Clin J Pain 27(2):169–181
Shiri R, Karppinen J, Leino-Arjas P, Solovieva S, Viikari-Juntura E (2010) The association between obesity and low back pain: a meta-analysis. Am J Epidemiol 171(2):135–154
Henschke N, Maher CG, Refshauge KM, Herbert RD, Cumming RG, Bleasel J, York J, Das A, McAuley JH (2008) Prognosis in patients with recent onset low back pain in Australian primary care: inception cohort study. Br Med J 337(7662):154–157
Opp MR (2005) Cytokines and sleep. Sleep Med Rev 9(5):355–364
Felger JC, Lotrich FE (2013) Inflammatory cytokines in depression: neurobiological mechanisms and therapeutic implications. Neuroscience 246:199–229
Haack M, Sanchez E, Mullington JM (2007) Elevated inflammatory markers in response to prolonged sleep restriction are associated with increased pain experience in healthy volunteers. Sleep 30(9):1145–1152
Edwards RR, Kronfli T, Haythornthwaite JA, Smith MT, Mcguire L, Page GG (2008) Association of catastrophizing with interleukin-6 responses to acute pain. Pain 140(1):135–144
Kubera M, Obuchowicz E, Goehler L, Brzeszcz J, Maes M (2011) In animal models, psychosocial stress-induced (neuro)inflammation, apoptosis and reduced neurogenesis are associated to the onset of depression. Prog Neuro-Psychoph 35(3):744–759
Roland M, Morris R (1983) A study of the natural history of back pain. Part I: development of a reliable and sensitive measure of disability in low-back pain. Spine (Phila Pa 1976) 8(2):141–144
Boonstra AM, Schiphorst Preuper HR, Balk GA, Stewart RE (2014) Cut-off points for mild, moderate, and severe pain on the visual analogue scale for pain in patients with chronic musculoskeletal pain. Pain 155(12):2545–2550
Backhaus J, Junghanns K, Broocks A, Riemann D, Hohagen F (2002) Test–retest reliability and validity of the Pittsburgh Sleep Quality Index in primary insomnia. J Psychosom Res 53(3):737–740
Carpenter JS, Andrykowski MA (1998) Psychometric evaluation of the Pittsburgh Sleep Quality Index. J Psychosom Res 45(1):5–13
Boersma K, Linton SJ (2005) How does persistent pain develop? An analysis of the relationship between psychological variables, pain and function across stages of chronicity. Behav Res Ther 43(11):1495–1507
Linton SJ (2000) A review of psychological risk factors in back and neck pain. Spine (Phila Pa 1976) 25(9):1148–1156
Mallen CD, Peat G, Thomas E, Dunn KM, Croft PR (2007) Prognostic factors for musculoskeletal pain in primary care: a systematic review. Brit J Gen Pract 57(541):655–661
Pincus T, Burton AK, Vogel S, Field AP (2002) A systematic review of psychological factors as predictors of chronicity/disability in prospective cohorts of low back pain. Spine (Phila Pa 1976) 27(5):E109–120
Metsalu T, Vilo J (2015) ClustVis: a web tool for visualizing clustering of multivariate data using principal component analysis and heatmap. Nucleic Acids Res 43(W1):W566–W570
Sterne JA, White IR, Carlin JB, Spratt M, Royston P, Kenward MG, Wood AM, Carpenter JR (2009) Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ 338:b2393
Moons KGM, Donders RART, Stijnen T, Harrell FE (2006) Using the outcome for imputation of missing predictor values was preferred. J Clin Epidemiol 59(10):1092–1101
Clyne B, Olshaker JS (1999) The C-reactive protein. J Emerg Med 17(6):1019–1025
Sarma JV, Ward PA (2011) The complement system. Cell Tissue Res 343(1):227–235
Lawrence T (2009) The nuclear factor NF-kappaB pathway in inflammation. Cold Spring Harb Perspect Biol 1(6):a001651
Liu N, Liu JT, Ji YY, Lu PP (2010) C-reactive protein triggers inflammatory responses partly via TLR4/IRF3/NF-kappaB signaling pathway in rat vascular smooth muscle cells. Life Sci 87(11–12):367–374
Wu Y, Potempa LA, El Kebir D, Filep JG (2015) C-reactive protein and inflammation: conformational changes affect function. Biol Chem 396(11):1181–1197
Volanakis JE (2001) Human C-reactive protein: expression, structure, and function. Mol Immunol 38(2–3):189–197
Ansar W, Ghosh S (2013) C-reactive protein and the biology of disease. Immunol Res 56(1):131–142
Thiele JR, Zeller J, Bannasch H, Stark GB, Peter K, Eisenhardt SU (2015) Targeting C-reactive protein in inflammatory disease by preventing conformational changes. Mediators Inflamm 2015. https://doi.org/10.1155/2015/372432
Braig D, Nero TL, Koch HG, Kaiser B, Wang X, Thiele JR, Morton CJ, Zeller J, Kiefer J, Potempa LA, Mellett NA, Miles LA, Du XJ, Meikle PJ, Huber-Lang M, Stark GB, Parker MW, Peter K, Eisenhardt SU (2017) Transitional changes in the CRP structure lead to the exposure of proinflammatory binding sites. Nat Commun 8:14188
Klyne DM, Barbe MF, Hodges PW (2017) Systemic inflammatory profiles and their relationships with demographic, behavioural and clinical features in acute low back pain. Brain Behav Immun 60:84–92
Pritchett JW (1996) C-reactive protein levels determine the severity of soft-tissue injuries. Am J Orthop (Belle Mead NJ) 25(11):759–761
Rechardt M, Shiri R, Matikainen S, Viikari-Juntura E, Karppinen J, Alenius H (2011) Soluble IL-1RII and IL-18 are associated with incipient upper extremity soft tissue disorders. Cytokine 54(2):149–153
Ackerman WE 3rd, Zhang JM (2006) Serum hs-CRP as a useful marker for predicting the efficacy of lumbar epidural steroid injections on pain relief in patients with lumbar disc herniations. J Ky Med Assoc 104(7):295–299
Sugimori K, Kawaguchi Y, Morita M, Kitajima I, Kimura T (2003) High-sensitivity analysis of serum C-reactive protein in young patients with lumbar disc herniation. J Bone Joint Surg Br 85(8):1151–1154
Takahashi H, Suguro T, Okazima Y, Motegi M, Okada Y, Kakiuchi T (1996) Inflammatory cytokines in the herniated disc of the lumbar spine. Spine (Phila Pa 1976) 21(2):218–224
Shamji MF, Setton LA, Jarvis W, So S, Chen J, Jing L, Bullock R, Isaacs RE, Brown C, Richardson WJ (2010) Proinflammatory cytokine expression profile in degenerated and herniated human intervertebral disc tissues. Arthritis Rheum 62(7):1974–1982
Risbud MV, Shapiro IM (2014) Role of cytokines in intervertebral disc degeneration: pain and disc content. Nat Rev Rheumatol 10(1):44–56
Kraychete DC, Sakata RK, Issy AM, Bacellar O, Santos-Jesus R, Carvalho EM (2010) Serum cytokine levels in patients with chronic low back pain due to herniated disc: analytical cross-sectional study. Sao Paulo Med J 128(5):259–262
Gillett A, Marta M, Jin T, Tuncel J, Leclerc P, Nohra R, Lange S, Holmdahl R, Olsson T, Harris RA, Jagodic M (2010) TNF production in macrophages is genetically determined and regulates inflammatory disease in rats. J Immunol 185(1):442–450
Louis E, Franchimont D, Piron A, Gevaert Y, Schaaf-Lafontaine N, Roland S, Mahieu P, Malaise M, De Groote D, Louis R, Belaiche J (1998) Tumour necrosis factor (TNF) gene polymorphism influences TNF-alpha production in lipopolysaccharide (LPS)-stimulated whole blood cell culture in healthy humans. Clin Exp Immunol 113(3):401–406
McGuire W, Hill AV, Allsopp CE, Greenwood BM, Kwiatkowski D (1994) Variation in the TNF-alpha promoter region associated with susceptibility to cerebral malaria. Nature 371(6497):508–510
Fernandez-Arquero M, Arroyo R, Rubio A, Martin C, Vigil P, Conejero L, Figueredo MA, de la Concha EG (1999) Primary association of a TNF gene polymorphism with susceptibility to multiple sclerosis. Neurology 53(6):1361–1363
Martinez A, Fernandez-Arquero M, Pascual-Salcedo D, Conejero L, Alves H, Balsa A, de la Concha EG (2000) Primary association of tumor necrosis factor-region genetic markers with susceptibility to rheumatoid arthritis. Arthritis Rheum 43(6):1366–1370
Biffl WL, Moore EE, Moore FA, Peterson VM (1996) Interleukin-6 in the injured patient marker of injury or mediator of inflammation? Ann Surg 224(5):647–664
Kalliolias GD, Ivashkiv LB (2016) TNF biology, pathogenic mechanisms and emerging therapeutic strategies. Nat Rev Rheumatol 12(1):49–62
Hehlgans T, Pfeffer K (2005) The intriguing biology of the tumour necrosis factor/tumour necrosis factor receptor superfamily: players, rules and the games. Immunology 115(1):1–20
McDermott MF (2001) TNF and TNFR biology in health and disease. Cell Mol Biol 47(4):619–635
Konig C, Zharsky M, Moller C, Schaible HG, Ebersberger A (2014) Involvement of peripheral and spinal tumor necrosis factor alpha in spinal cord hyperexcitability during knee joint inflammation in rats. Arthritis Rheumatol 66(3):599–609
Boettger MK, Weber K, Grossmann D, Gajda M, Bauer R, Bar KJ, Schulz S, Voss A, Geis C, Brauer R, Schaible HG (2010) Spinal tumor necrosis factor alpha neutralization reduces peripheral inflammation and hyperalgesia and suppresses autonomic responses in experimental arthritis: a role for spinal tumor necrosis factor alpha during induction and maintenance of peripheral inflammation. Arthritis Rheum 62(5):1308–1318
Richter F, Natura G, Loser S, Schmidt K, Viisanen H, Schaible HG (2010) Tumor necrosis factor causes persistent sensitization of joint nociceptors to mechanical stimuli in rats. Arthritis Rheum 62(12):3806–3814
Boettger MK, Hensellek S, Richter F, Gajda M, Stockigt R, von Banchet GS, Brauer R, Schaible HG (2008) Antinociceptive effects of tumor necrosis factor alpha neutralization in a rat model of antigen-induced arthritis. Arthritis Rheum 58(8):2368–2378
Inglis JJ, Notley CA, Essex D, Wilson AW, Feldmann M, Anand P, Williams R (2007) Collagen-induced arthritis as a model of hyperalgesia. Arthritis Rheum 56(12):4015–4023
Hess A, Axmann R, Rech J, Finzel S, Heindl C, Kreitz S, Sergeeva M, Saake M, Garcia M, Kollias G, Straub RH, Sporns O, Doerfler A, Brune K, Schett G (2011) Blockade of TNF-alpha rapidly inhibits pain responses in the central nervous system. Proc Natl Acad Sci USA 108(9):3731–3736
Andrade P, Visser-Vandewalle V, Hoffmann C, Steinbusch HW, Daemen MA, Hoogland G (2011) Role of TNF-alpha during central sensitization in preclinical studies. Neurol Sci 32(5):757–771
Zhang L, Berta T, Xu ZZ, Liu T, Park JY, Ji RR (2011) TNF-alpha contributes to spinal cord synaptic plasticity and inflammatory pain: distinct role of TNF receptor subtypes 1 and 2. Pain 152(2):419–427
Marchand F, Perretti M, McMahon SB (2005) Role of the immune system in chronic pain. Nat Rev Neurosci 6(7):521–532
McMahon SB, Cafferty WBJ, Marchand F (2005) Immune and glial cell factors as pain mediators and modulators. Exp Neurol 192(2):444–462
O’Sullivan P, Waller R, Wright A, Gardner J, Johnston R, Payne C, Shannon A, Ware B, Smith A (2014) Sensory characteristics of chronic non-specific low back pain: a subgroup investigation. Man Ther 19(4):311–318
O’Neill S, Manniche C, Graven-Nielsen T, Arendt-Nielsen L (2007) Generalized deep-tissue hyperalgesia in patients with chronic low-back pain. Eur J Pain 11(4):415–420
Edwards RR, Wasan AD, Michna E, Greenbaum S, Ross E, Jamison RN (2011) Elevated pain sensitivity in chronic pain patients at risk for opioid misuse. J Pain 12(9):953–963
Li SP, Goldman ND (1996) Regulation of human C-reactive protein gene expression by two synergistic IL-6 responsive elements. Biochemistry-Us 35(28):9060–9068
Friedman EM, Herd P (2010) Income, education, and inflammation: differential associations in a national probability sample (The MIDUS Study). Psychosom Med 72(3):290–300
Howren MB, Lamkin DM, Suls J (2009) Associations of depression with C-reactive protein, IL-1, and IL-6: a meta-analysis. Psychosom Med 71(2):171–186
Slaats J, ten Oever J, van de Veerdonk FL, Netea MG (2016) IL-1β/IL-6/CRP and IL-18/ferritin: distinct inflammatory programs in infections. Plos Pathog 12(12):e1005973
Kopf M, Baumann H, Freer G, Freudenberg M, Lamers M, Kishimoto T, Zinkernagel R, Bluethmann H, Kohler G (1994) Impaired immune and acute-phase responses in interleukin-6-deficient mice. Nature 368(6469):339–342
McLoughlin RM, Jenkins BJ, Grail D, Williams AS, Fielding CA, Parker CR, Ernst M, Topley N, Jones SA (2005) IL-6 trans-signaling via STAT3 directs T cell infiltration in acute inflammation. Proc Natl Acad Sci USA 102(27):9589–9594
Scheller J, Chalaris A, Schmidt-Arras D, Rose-John S (2011) The pro- and anti-inflammatory properties of the cytokine interleukin-6. BBA-Mol Cell Res 1813(5):878–888
Ulich TR, Yin SM, Guo KZ, Yi EHS, Remick D, Delcastillo J (1991) Intratracheal injection of endotoxin and cytokines. 2. interleukin-6 and transforming growth-factor-beta inhibit acute-inflammation. Am J Pathol 138(5):1097–1101
Tilg H, Trehu E, Atkins MB, Dinarello CA, Mier JW (1994) Interleukin-6 (Il-6) as an antiinflammatory cytokine—induction of circulating Il-1-receptor antagonist and soluble tumor-necrosis-factor receptor-P55. Blood 83(1):113–118
Schindler R, Mancilla J, Endres S, Ghorbani R, Clark SC, Dinarello CA (1990) Correlations and interactions in the production of interleukin-6 (Il-6), Il-1, and tumor necrosis factor (Tnf) in human-blood mononuclear-cells—Il-6 suppresses Il-1 and TNF. Blood 75(1):40–47
Aderka D, Le JM, Vilcek J (1989) Il-6 inhibits lipopolysaccharide-induced tumor necrosis factor production in cultured human-monocytes, U937 cells, and in mice. J Immunol 143(11):3517–3523
McGeachy MJ, Bak-Jensen KS, Chen Y, Tato CM, Blumenschein W, McClanahan T, Cua DJ (2007) TGF-beta and IL-6 drive the production of IL-17 and IL-10 by T cells and restrain TH-17 cell-mediated pathology. Nat Immunol 8(12):1390–1397
Stumhofer JS, Silver JS, Laurence A, Porrett PM, Harris TH, Turka LA, Ernst M, Saris CJM, O’Shea JJ, Hunter CA (2007) Interleukins 27 and 6 induce STAT3-mediated T cell production of interleukin 10. Nat Immunol 8(12):1363–U1365
Xing Z, Gauldie J, Cox G, Baumann H, Jordana M, Lei XF, Achong MK (1998) IL-6 is an antiinflammatory cytokine required for controlling local or systemic acute inflammatory responses. J Clin Invest 101(2):311–320
Adser H, Wojtaszewski JFP, Jakobsen AH, Kiilerich K, Hidalgo J, Pilegaard H (2011) Interleukin-6 modifies mRNA expression in mouse skeletal muscle. Acta Physiol 202(2):165–173
Chennaoui M, Sauvet F, Drogou C, Van Beers P, Langrume C, Guillard M, Gourby B, Bourrilhon C, Florence G, Gomez-Merino D (2011) Effect of one night of sleep loss on changes in tumor necrosis factor alpha (TNF-alpha) levels in healthy men. Cytokine 56(2):318–324
Irwin MR, Olmstead R, Carroll JE (2016) Sleep disturbance, sleep duration, and inflammation: a systematic review and meta-analysis of cohort studies and experimental sleep deprivation. Biol Psychiat 80(1):40–52
Irwin MR, Wang M, Campomayor CO, Collado-Hidalgo A, Cole S (2006) Sleep deprivation and activation of morning levels of cellular and genomic markers of inflammation. Arch Intern Med 166(16):1756–1762
Vgontzas AN, Bixler EO, Lin HM, Prolo P, Trakada G, Chrousos GP (2005) IL-6 and its circadian secretion in humans. Neuroimmunomodulat 12(3):131–140
Vgontzas AN, Papanicolaou DA, Bixler EO, Lotsikas A, Zachman K, Kales A, Prolo P, Wong ML, Licinio J, Gold PW, Hermida RC, Mastorakos G, Chrousos GP (1999) Circadian interleukin-6 secretion and quantity and depth of sleep. J Clin Endocrinol Metab 84(8):2603–2607
Irwin MR, Cole SW (2011) Reciprocal regulation of the neural and innate immune systems. Nat Rev Immunol 11(9):625–632
Slavich GM, Irwin MR (2014) From stress to inflammation and major depressive disorder: a social signal transduction theory of depression. Psychol Bull 140(3):774–815
Hogan D, Morrow JD, Smith EM, Opp MR (2003) Interleukin-6 alters sleep of rats. J Neuroimmunol 137(1–2):59–66
Hurtado-Alvarado G, Pavon L, Castillo-Garcia SA, Hernandez ME, Dominguez-Salazar E, Velazquez-Moctezuma J, Gomez-Gonzalez B (2013) Sleep loss as a factor to induce cellular and molecular inflammatory variations. Clin Dev Immunol 2013:801341. https://doi.org/10.1155/2013/801341
Krueger JM, Clinton JM, Winters BD, Zielinski MR, Taishi P, Jewett KA, Davis CJ (2011) Involvement of cytokines in slow wave sleep. Prog Brain Res 193:39–47
Rohleder N, Aringer M, Boentert M (2012) Role of interleukin-6 in stress, sleep, and fatigue. Ann N Y Acad Sci 1261:88–96
Davis CJ, Krueger JM (2012) Sleep and cytokines. Sleep Med Clin 7(3):517–527
Vgontzas AN, Papanicolaou DA, Bixler EO, Kales A, Tyson K, Chrousos GP (1997) Elevation of plasma cytokines in disorders of excessive daytime sleepiness: role of sleep disturbance and obesity. J Clin Endocrinol Metab 82(5):1313–1316
Fasick V, Spengler RN, Samankan S, Nader ND, Ignatowski TA (2015) The hippocampus and TNF: common links between chronic pain and depression. Neurosci Biobehav R 53:139–159
Tuglu C, Kara SH, Caliyurt O, Vardar E, Abay E (2003) Increased serum tumor necrosis factor-alpha levels and treatment response in major depressive disorder. Psychopharmacology 170(4):429–433
Liu Y, Ho RC, Mak A (2012) Interleukin (IL)-6, tumour necrosis factor alpha (TNF-alpha) and soluble interleukin-2 receptors (sIL-2R) are elevated in patients with major depressive disorder: a meta-analysis and meta-regression. J Affect Disord 139(3):230–239
Blackburn-Munro G, Blackburn-Munro RE (2001) Chronic pain, chronic stress and depression: coincidence or consequence? J Neuroendocrinol 13(12):1009–1023
de Kloet ER, DeRijk RH, Meijer OC (2007) Therapy insight: is there an imbalanced response of mineralocorticoid and glucocorticoid receptors in depression? Nat Clin Pract Endoc 3(2):168–179
Mirescu C, Gould E (2006) Stress and adult neurogenesis. Hippocampus 16(3):233–238
Raison CL, Miller AH (2003) When not enough is too much: the role of insufficient glucocorticoid signaling in the pathophysiology of stress-related disorders. Am J Psychiatry 160(9):1554–1565
McEwen BS, Biron CA, Brunson KW, Bulloch K, Chambers WH, Dhabhar FS, Goldfarb RH, Kitson RP, Miller AH, Spencer RL, Weiss JM (1997) The role of adrenocorticoids as modulators of immune function in health and disease: neural, endocrine and immune interactions. Brain Res Rev 23(1–2):79–133
Reynolds JL, Ignatowski TA, Sud R, Spengler RN (2005) An antidepressant mechanism of desipramine is to decrease tumor necrosis factor-alpha production culminating in increases in noradrenergic neurotransmission. Neuroscience 133(2):519–531
Harro J, Oreland L (2001) Depression as a spreading adjustment disorder of monoaminergic neurons: a case for primary implication of the locus coeruleus. Brain Res Rev 38(1–2):79–128
Meyer JH, Ginovart N, Boovariwala A, Sagrati S, Hussey D, Garcia A, Young T, Praschak-Rieder N, Wilson AA, Houle S (2006) Elevated monoamine oxidase a levels in the brain: an explanation for the monoamine imbalance of major depression. Arch Gen Psychiatry 63(11):1209–1216
Hoogland IC, Houbolt C, van Westerloo DJ, van Gool WA, van de Beek D (2015) Systemic inflammation and microglial activation: systematic review of animal experiments. J Neuroinflammation 12:114
Capuron L, Miller AH (2011) Immune system to brain signaling: neuropsychopharmacological implications. Pharmacol Ther 130(2):226–238
Reynolds JL, Ignatowski TA, Sud R, Spengler RN (2004) Brain-derived tumor necrosis factor-alpha and its involvement in noradrenergic neuron functioning involved in the mechanism of action of an antidepressant. J Pharmacol Exp Ther 310(3):1216–1225
Martuscello RT, Spengler RN, Bonoiu AC, Davidson BA, Helinski J, Ding H, Mahajan S, Kumar R, Bergey EJ, Knight PR, Prasad PN, Ignatowski TA (2012) Increasing TNF levels solely in the rat hippocampus produces persistent pain-like symptoms. Pain 153(9):1871–1882
Sud R, Ignatowski TA, Lo CP, Spengler RN (2007) Uncovering molecular elements of brain-body communication during development and treatment of neuropathic pain. Brain Behav Immun 21(1):112–124
Ignatowski TA, Covey WC, Knight PR, Severin CM, Nickola TJ, Spengler RN (1999) Brain-derived TNFalpha mediates neuropathic pain. Brain Res 841(1–2):70–77
Covey WC, Ignatowski TA, Knight PR, Spengler RN (2000) Brain-derived TNFalpha: involvement in neuroplastic changes implicated in the conscious perception of persistent pain. Brain Res 859(1):113–122
Strouse TB (2007) The Relationship between cytokines and pain/depression. Curr Pain Headache Rep 11(2):98–103
Darnall BD, Aickin M, Zwickey H (2010) pilot study of inflammatory responses following a negative imaginal focus in persons with chronic pain: analysis by sex/gender. Gender Med 7(3):247–260
Kemp DE, Ganocy SJ, Brecher M, Carlson BX, Edwards S, Eudicone JM, Evoniuk G, Jansen W, Leon AC, Minkwitz M, Pikalov A, Stassen HH, Szegedi A, Tohen M, Van Willigenburg AP, Calabrese JR (2011) Clinical value of early partial symptomatic improvement in the prediction of response and remission during short-term treatment trials in 3369 subjects with bipolar I or II depression. J Affect Disord 130(1–2):171–179
Katz MM, Koslow SH, Frazer A (1996) Onset of antidepressant activity: reexamining the structure of depression and multiple actions of drugs. Depress Anxiety 4(6):257–267
Katz MM, Bowden C, Stokes P, Casper R, Frazer A, Koslow SH, Kocsis J, Secunda S, Swann A, Berman N (1997) Can the effects of antidepressants be observed in the first two weeks of treatment? Neuropsychopharmacol 17(2):110–112
O’Brien SM, Scully P, Fitzgerald P, Scott LV, Dinan TG (2007) Plasma cytokine profiles in depressed patients who fail to respond to selective serotonin reuptake inhibitor therapy. J Psychiatr Res 41(3–4):326–331
Maletic V, Robinson M, Oakes T, Iyengar S, Ball SG, Russell J (2007) Neurobiology of depression: an integrated view of key findings. Int J Clin Pract 61(12):2030–2040
O’Connor JC, Lawson MA, Andre C, Moreau M, Lestage J, Castanon N, Kelley KW, Dantzer R (2009) Lipopolysaccharide-induced depressive-like behavior is mediated by indoleamine 2,3-dioxygenase activation in mice. Mol Psychiatr 14(5):511–522
Kaster MP, Gadotti VM, Calixto JB, Santos AR, Rodrigues AL (2012) Depressive-like behavior induced by tumor necrosis factor-alpha in mice. Neuropharmacology 62(1):419–426
Scheff JD, Calvano SE, Lowry SF, Androulakis IP (2010) Modeling the influence of circadian rhythms on the acute inflammatory response. J Theor Biol 264(3):1068–1076
Petrovsky N, McNair P, Harrison LC (1998) Diurnal rhythms of pro-inflammatory cytokines: regulation by plasma cortisol and therapeutic implications. Cytokine 10(4):307–312
Sitton NG, Taggart AJ, Dixon JS, Surrall KE, Bird HA (1984) Circadian variation in biochemical assessments used to monitor rheumatoid-arthritis. Ann Rheum Dis 43(3):444–450
Meier-Ewert HK, Ridker PM, Rifai N, Price N, Dinges DF, Mullington JM (2001) Absence of diurnal variation of C-reactive protein concentrations in healthy human subjects. Clin Chem 47(3):426–430
Funding
This research was funded by the National Health and Medical Research Council (NHMRC) of Australia (Program Grant: ID631717; Project Grant ID631369). PWH supported by NHMRC Fellowship ID1002190. The manuscript submitted does not contain information about medical device(s)/drug(s).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There are no conflicts of interest related to this work.
Ethical approval
Approved by The University of Queensland Institutional Medical Research Ethics Committee.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Klyne, D.M., Barbe, M.F., van den Hoorn, W. et al. ISSLS PRIZE IN CLINICAL SCIENCE 2018: longitudinal analysis of inflammatory, psychological, and sleep-related factors following an acute low back pain episode—the good, the bad, and the ugly. Eur Spine J 27, 763–777 (2018). https://doi.org/10.1007/s00586-018-5490-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-018-5490-7