Abstract
Background
Low back pain (LBP) is a common musculoskeletal condition and a major cause of disability worldwide. Previous studies have found associations of biomarkers with pain and pain-related disability in LBP patients. This study aimed to explore the association between serum biomarkers and pain and disability in patients with acute or subacute axial LBP.
Methods
This study was ancillary to a parent randomized controlled trial. Enrolled participants were randomized into three intervention groups: one of two types of spinal manipulation or medical care. In the parent study, 107 adults who experienced a new episode of LBP within 3 months prior to enrollment were recruited. For this study, 90 of these 107 participants consented to have blood samples obtained, which were drawn immediately before the beginning of treatment. Seven biomarkers were chosen based on previous literature and analyzed. Clinical outcomes were pain and Oswestry Disability Index (ODI) evaluated at baseline and 4 weeks. Spearman’s |r| was used to study the association of initial levels of each biomarker with pain and ODI scores at baseline and with changes in outcome scores from baseline to 4 weeks (end of treatment) within each intervention group.
Results
At baseline, 4 of 7 biomarkers had an association with pain that was |r| ≥ .20: neuropeptide Y (NPY) (r = 0.23, p = .028), E-Selectin (r = 0.22, p = .043), vitamin D ((r = − 0.32, p = .002), and c-reactive protein (CRP) (r = 0.37, p = .001). No baseline biomarker had an association with disability that was |r| ≥ 0.20. For the correlations of baseline biomarkers with 4-week change in outcomes, vitamin D showed a correlation with change in disability and/or pain (|r| ≥ 0.20, p > .05) in manipulation-related groups, while CRP, NPY, and E-selectin along with TNFα, Substance P and RANTES showed at least one correlation with change in pain or disability (|r| ≥ 0.20, p > .05) in at least one of the treatment groups.
Conclusions
In 90 LBP patients, the analyzed biomarkers, especially vitamin D, represent a small set of potential candidates for further research aimed at individualizing patient care. Overall, the associations investigated in the current study are an initial step in identifying the direct mechanisms of LBP and predicting outcomes of manipulation-related treatments or medical care.
Trial registration
ClinicalTrials.gov Identifier: NCT01211613, Date of Registration: September 29, 2010, https://clinicaltrials.gov/ct2/show/NCT01211613?term=schneider&cond=Low+Back+Pain&cntry=US&state=US%3APA&draw=2&rank=1
Similar content being viewed by others
Background
Low back pain (LBP) is one of the most common musculoskeletal conditions requiring medical care and contributing to patient impairment and disability. Over 25% of the general population reports LBP at any given time [1], with a lifetime incidence exceeding 80% and a lifetime prevalence of around 40% [2]. However, the care of LBP represents one of the most significant challenges facing musculoskeletal care today. In the US, estimated annual costs for LBP alone were over $85 billion in 2005 [3], while in 2016, the combined cost for neck and LBP accounted for over $134 billion [4], highlighting the significant spending to treat this condition.
Despite these high costs, treatment outcomes and rates of disability have not improved [5], which may partly explain the growing interest in complementary medical treatments. Data from the 2012 National Health Interview Survey, Alternative Health Supplement demonstrate that 41.2% of the LBP population used complementary and alternative medicine approaches for pain relief, with herbal supplements, massage, and chiropractic manipulation being the most common therapies [6]. Previous data demonstrate short-term reductions in self-reported disability and pain scores in patients treated with manual thrust manipulation compared to usual medical care [7].
Diagnostic tools are necessary to identify patients with LBP who are likely to respond to different treatments, including manual therapy. Currently, a reliable method for selecting the most appropriate care for LBP patients is unavailable; identifying specific subgroups of patients would most likely improve outcomes and make interventions more cost-effective [8]. Biomarkers have the potential to become a valuable and novel tool in establishing individualized treatment plans by providing information about the mechanisms of action of clinical treatments and their related outcomes.
Some biomarkers have already shown an association with pain and pain-related disability in LBP patients, superior to any contribution by imaging studies [9]. Biomarkers have also garnered attention in manipulative treatment in several prior small studies. In a recent systematic review and meta-analysis of randomized clinical trials (RCTs) [10], varying degrees of evidence showed significant associations between spinal manipulation and various biomarkers up to 2 hours after the intervention. Overall, non-pooled results from 8 studies showed moderate evidence that spinal manipulation was associated with short-term biochemical markers changes after receiving spinal manipulation compared to controls (325 participants total). In the three studies (n = 173) investigating the effect of spinal manipulation on inflammatory biomarkers, moderate-quality evidence was found that spinal manipulation is more impactful than the control in influencing the short-term concentrations of tumor necrosis factor-alpha (TNFα) and interleukin 1 and 2 (IL-1, IL-2). These studies are characterized by a short-term assessment period of biomarkers’ levels after spinal manipulation, and they did not assess associations with clinical outcomes.
A more recent systematic review that focused on the effect of spinal manipulation and markers of immune function [11] found that the evidence is too weak to draw definite conclusions on the effect of spinal manipulation on immune system outcomes. The review acknowledged that short-term changes in immunological markers exist after spinal manipulation; yet, the only study that included specific blood markers of inflammation was a 2006 study by Teodorczyk-Injeyan et al., which was also included in the Kovanur-Sampath et al. review from 2017 mentioned previously. The authors also concluded that the clinical implications of such findings were unclear.
A non-randomized clinical trial [12] showed that IL-6 and C-reactive protein (CRP) levels decreased towards the levels of the healthy, pain-free control group in a small study of 10 patients with chronic LBP treated with nine sessions of mechanical-assisted manipulation. However, this study did not include any control subjects with LBP. Moreover, a study comparing 10 subjects with chronic LBP to 10 non-LBP controls showed decreased circulating levels of 5-hydroxyindoleacetic acid and serotonin4 hours after osteopathic manipulative treatment [13]. A case report shows a reduction in TNFα levels after manipulative therapy in two cervicogenic headache patients [14] [12]..
Two systematic reviews were recently published on the relationship between inflammatory biomarkers and LBP. In one [15], the authors concluded that CRP, TNFs, and IL-6 were positively associated with non-specific LBP. In the other study [16], the authors found that CRP levels were associated with acute non-specific LBP and TNFαwith chronic non-specific LBP. These reviews did not look at clinical effects or changes specific to spinal manipulation treatments. Interestingly, a newly published study found that a cluster of subjects with acute LBP characterized by an early combined presence of both IL-6 and CRP was associated with better recovery at 12 months than a different group characterized by elevated TNFα and depressive symptoms. Even though this study was observational, the association between inflammatory markers and clinical outcomes points to a potential role for such markers in determining the trajectory of recovery for individuals with acute LBP.
Overall, as pointed out in the most recent systematic reviews [15, 16], the current literature is characterized by numerous limitations that affect study quality, such as small sample size and lack of proper control groups. Two others are particularly relevant to our work. The first is not examining the changes in biomarker levels outside a narrow time window immediately before and after the intervention. The second limitation is focusing only on changes in biomarker levels without correlating these changes with clinically relevant outcomes such as reducing pain intensity or physical function. These limitations leave potentially relevant questions unanswered about the spinal manipulation’s medium- to long-term impact on homeostasis, physiological variances, and clinically meaningful outcomes. The current study aimed to explore the association of serum biomarkers with baseline and changes in self-reported pain and disability in LBP patients treated with spinal manipulation or standard medical care for acute and subacute axial LBP.
Methods
Recruitment
This biomarkers study was ancillary to a parent RCT that investigated patient outcomes in response to two types of spinal manipulation and medical care [7]. In the parent RCT, 107 adults (18 years or older) who experienced a new episode of LBP within the 3 months prior to enrollment were recruited from a single academic center. The study was conducted between November 2010 and March 2013, and was designed to adhere to CONSORT guidelines. Eligible subjects (Table 1) had an Oswestry Disability Index score between 20 and 70 points (0–100 scale) and a numeric pain rating score between 3 and 8 points (0–10 scale). Patients were excluded if they had: 1) prior history of lumbar spine surgery, unstable spondylolisthesis, spinal stenosis, or scoliosis > 20°; 2) signs or symptoms suggestive of nerve root tension or neurological deficit in the lower extremity; 3) red flag findings (including a history of metastatic cancer, osteoporosis, long-term corticosteroid use, unexplained weight loss of > 10% of body weight, spinal pain associated with fever, and severe night pain unrelieved by medication); 4) were receiving any physical therapy, chiropractic therapy, or any other manual therapy for this episode of LBP (within the past 3 months) or any on-going medical care for this episode of LBP; or 5) had a current use of opiate or other prescription medications for LBP, or were pregnant.
Individuals were randomized into one of three intervention groups: manual-thrust manipulation, using high-velocity, low-amplitude thrust manipulation using standard chiropractic methods by a licensed chiropractor (group 1); mechanically-assisted manipulation using an Activator IV Instrument (Activator Methods International Ltd., Phoenix, AZ) (group 2); or standard medical care provided by a board-certified physician in physical medicine and rehabilitation (group 3) [7]. The high-velocity, low-amplitude thrust manipulation varied from patient to patient but was either side posture, diversified, or drop table technique. Furthermore, the location of the adjustment (manipulation technique) varied from patient to patient, based upon their individual needs. The clinicians were allowed to adjust the sacroiliac joints and/or any facet joints from L5-S1 up to T6–7. The protocol did not allow for any manipulation of the cervical or upper thoracic segments or any extremity joints. Moreover, all patients assigned to manipulation were seen twice a week for 4 weeks. The standard medical care approach consisted of a protocol in line with guidelines for the clinical management of non-specific LBP [17]. Randomization was performed using a rank-based adaptive allocation approach; more information on the methodology can be found in the published manuscript from the parent study [7]. Blinding was not possible due to the study design.
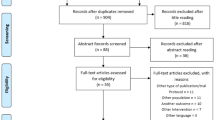
Before randomization, subjects were asked if they were willing to participate in the ancillary biomarkers study, which would require them to have blood drawn upon initiating the course of treatment. Subjects who agreed to participate in the ancillary study were taken through a separate consent process, and a separate University of Pittsburgh Institutional Review Board approval was obtained for the biomarker study. Participation in the biomarker study did not influence participation in the parent RCT. Of the 107 adults with LBP who participated in the parent RCT, 90 agreed to participate in the ancillary biomarker study (group 1, n = 33; group 2, n = 27; group 3, n = 30). For the analysis of the 4-week change in pain and disability scores, 4 subjects were lost to follow-up, one data was missing for the change in pain variable, and two data were missing for change in Oswestry Disability Index (ODI) (group 1, n = 30; group 2, n = 26; group 3, n = 29 for pain and n = 28 for ODI). No other subjects were excluded for any other reasons.
No power calculation was performed for this secondary analysis since a convenience sample was used. All investigators involved in the biomarker analysis remained blinded to treatment assignment until after the completion of the trial.
Blood sampling and assays
Blood samples were drawn from participants immediately before the first treatment session at baseline. About 10 ml of venous blood was collected into Serum Separation Tubes Vacutainers (4 ml, Ref# 367977) and EDTA pre-coated vacutainers (6 ml, Ref# 367863), both from BD (Fullerton, CA) and kept in ice. Serum Separation Tubes Vacutainers were immediately sent to the nearby clinical lab to measure Vitamin D and CRP, whereas the samples in the EDTA vacutainers were centrifuged within 2 hours at 1000 g for 10 min for enzyme-linked immunosorbent assay (ELISA). The resulting plasma was pipetted out and divided into Eppendorf tubes, which were pre-labeled with patients ID, and immediately frozen at -80oC. Plasma samples were analyzed by ELISA using a commercially available 96-well ELISA kits: Neuropeptide Y (NPY) and E-selectin from (RayBiotech Inc., Norcross, GA), and Substance P, TNF-a, and RANTES (regulated on activation, normal T cell expressed and secreted, also known as C-C Motif Chemokine Ligand 5 (CCL5)) from Cayman Chemical (Ann Arbor, MI). All assays were performed in duplicate and following the manufacturer’s instructions, and the intraassay and interassay coefficients of variation are < 10% for all ELISAs. The selection of biomarkers was based on previous reports of their association with LBP [9, 18,19,20,21,22]. Vitamin D and CRP levels were also obtained from the samples taken immediately before treatment; a local clinical lab performed their standard analysis.
Clinical data collection
Baseline demographic and clinical information, including age, BMI, gender, race, employment status, general health, presence/absence of metabolic syndrome, tobacco use, fear-avoidance beliefs [23], baseline NSAID use, treatment expectancy as measured by the Treatment Credibility Expectancy Questionnaire and intermittent vs. constant nature of symptoms were collected. Primary clinical outcomes were pain measured by the von Korff pain scale [24] and disability measured by the Oswestry Disability Index (ODI) [25]. Pain and ODI scores were measured at the beginning of the first (baseline) and last (4-weeks) treatment sessions.
Statistical analysis
The strength of the relationship between the pain/disability variables and each of the biomarkers was quantified using non-parametric Spearman’s rank-order correlation (Spearman’s rho [r]). Baseline correlations were computed using all 90 subjects because the data from the parent RCT were collected prior to randomization and interventions.
The correlations of improvement of pain and disability outcomes with baseline biomarkers were evaluated by treatment type. This approach was chosen because of the effects of the interventions on the outcomes [7]. Scatterplots were visually inspected for apparent violation of the assumption of a monotonically increasing or decreasing association between variables. None were noted.
Results
The majority of participants from the randomized trial agreed to join the biomarker study (90/107 = 84%) (Table 2). A chi-square test showed no significant difference between the study groups in the proportion of participants from the parent study who enrolled (p = .358): group 1 = 33/35 (85%), group 2 = 27/37 (89%), and group 3 = 30/35 (77%).
In the baseline analysis of all 90 subjects as a whole (Table 3), an association of r ≥ 0.20 was found for pain with NPY(r = 0.23, p = .028) and E-Selectin (r = 0.22, p = .043). Additionally, an association of |r| ≥ 0.30 was found for pain with vitamin D (r = − 0.32, p = .002) and CRP (r = 0.37, p = .001). At baseline, there were no correlations of the 7 biomarkers with disability at the level of |r| ≥ 0.20.
The associations between baseline biomarkers levels and changes in pain from baseline to 4 weeks by treatment group are presented in Table 4. Ten correlations of biomarkers with disability improvement and 6 with pain improvement had a magnitude of |r| ≥ 0.20 (p > .05). Of these, 4 biomarkers had correlations with disability improvement that reached |r| ≥ 0.30 (p > .05).
Discussion
This study was the first to examine molecular biomarkers and clinical metrics in patients with axial LBP randomized to manipulation versus standard medical care. As a secondary analysis of an RCT dataset, the goal was to examine and identify potential biomarkers of interest related to pain and functional disability for future validation.
The initial CRP levels were correlated with baseline pain values, with a |r| value of 0.37.; however, the correlation between CRP and baseline function showed a much smaller correlation. CRP also showed correlation coefficients of magnitude between |r| = 0.20 and |r| = 0.31 across the 3 treatment groups associated with changes in pain and in the manual manipulation and mechanical manipulation groups associated with changes in ODI. Previous literature has shown an association between CRP and LBP [15, 16, 26]. Interestingly, higher CRP levels in the acute phase have been associated with better recovery than initial lower CRP levels (when lower levels are associated with other comorbidities, such as depression or sleep disturbances) [26]; similar findings were replicated in the 12-months outcomes of a recent prospective cohort [27]. Our findings partially align with previous results and may eventually translate into clinical practice [28].
The current lack of understanding of the mechanisms by which these markers affect pain and treatment trajectory underscores the need for studying this potential marker in future studies. This could potentially provide further insight into the interaction between CRP levels and LBP and potential mechanisms of action of manipulation. Nonetheless, this result highlights the need to consider this biomarker for future research on its mechanistic role in spinal manipulation.
The second important finding was that baseline Vitamin D concentrations were inversely correlated with baseline pain (r = − 0.32). This baseline correlation is in line with growing evidence on the contributing role of vitamin D on musculoskeletal pain and, more specifically, on LBP [29]. Even though the evidence is not conclusive, there is growing consensus that decreased levels of vitamin D are associated with pain syndromes [30] and that vitamin D could be administered to people to help decrease pain [31], especially if their initial vitamin D levels are low [32]. Vitamin D levels were also correlated with pain changes and ODI changes in the manual manipulation group and with changes in ODI in the mechanical manipulation group, with coefficients ranging between |r| = 0.24 and |r| = 0.31.
The evidence from the current study suggests that vitamin D could be a potential predictive biomarker for physical treatment outcomes. Besides its effects on the skeletal system, vitamin D also influences nervous, immune, and cardiovascular systems through its vital role in calcium metabolism. Therefore, the explanation for the possible correlation between baseline vitamin D with the manipulation outcomes could be multifactorial and prompts further investigations. Unfortunately, and to the best of our knowledge, no research on this topic has been performed yet. However, a review article has pointed out that vitamin D presurgical levels could predict surgical outcomes [33]. Though manipulation is not an intervention as invasive as surgery, the outcomes of manipulation may similarly be impacted by the baseline vitamin D levels. We suggest that vitamin D should be included in future studies on pain, biomarkers, and treatment outcomes, with particular attention to manipulation treatment to investigate this relationship further.
Both CRP and vitamin D had a Spearman’s Rho above 0.30; while this value is generally acknowledged in research as low to moderate strength, further discussion is warranted within the context of biomarkers and LBP. Regarding biomarkers’ association with clinical features, previous literature has been published with a similar correlation coefficient when looking at clinical variables such as pain and change in functional score (also assessed with ODI) [9, 34]. It could be that the strength of correlation of a single blood marker should be considered within the context of how it correlates with clinical features and their application in the decision-making process for clinical treatment. In addition, it is implausible that any single biomarker alone would be able to determine the clinical course of action, but rather should be considered in the context of a complex clinical presentation. In this light, even a 0.20 correlation may contribute to making impactful decisions regarding clinically complex patients. This is particularly true when considering that the approach often used for clinical decision-making for LBP treatment relies heavily on diagnostic imaging, which has not been found to be correlated with pain and function [9, 35, 36]. While these associations are not sufficient independently to impact clinical guidelines, they represent an important contribution to potentially supplementing diagnostic and prognostic tools.
Furthermore, we found associations between baseline levels of NPY and E-Selectin, both of which had a correlation coefficient above 0.20. NPY levels have been found in previous literature to be correlated with chronic pain [37], though our finding in acute and subacute LBP subjects is novel, warranting further research involving this biomarker. The literature on E-Selectin and pain shows an unclear trend. There is evidence of a significant correlation between baseline E-Selectin and pain levels for patients with chronic LBP (but not acute) [19]. However, another study found no association between E-selectin levels and pain or pain-related function in an older adult cohort with disc degeneration [9]. Our study highlights that pain levels in acute and subacute LBP patients may be associated with heightened levels of E-selectin, thus adding evidence to an area of research that needs clarification [37,38,39,40].
This study allowed us to explore the potential association between biomarkers and treatment outcomes. This topic has been gaining increasing attention in the literature, having been explored across this population and by treatment groups. The examined biomarkers represent only a sampling of potential biomarkers that may show important associations. We chose to study well-known inflammatory and pain biomarkers in this initial effort to identify candidate predictive biomarkers. While clearly, additional validation and an examination of a broader array of biomarkers are needed, these findings support future research on the potential utility of circulating biomarkers in this population.
Considering the small numbers of patients in each treatment group, though no significant correlations were found, even a 0.20 correlation may contribute to making impactful decisions when choosing manipulation-related treatments over usual medical care for LBP. Interestingly, vitamin D showed a change in disability and/or change in pain (|r| ≥ 0.20) in manipulation-related treatment groups only. This pattern warrants further study with a larger study population. The correlation coefficient of the other analyzed biomarkers was at least 0.20 associated with pain and/or ODI changes at 4 weeks in one of three treatment groups. These results are difficult to interpret since they present across different treatment groups.
The small sample sizes for each group are clear limitations to these results. These limitations are even more relevant because we used this exploratory analysis for multiple comparisons. However, this limitation is tempered by the need for novel targets and the risk of missed findings. This study had some other limitations, including its small sample size and exploratory nature. The data distribution could not be considered normal, which was addressed using non-parametric statistical analysis. Furthermore, the average BMI value for the included population was elevated (29 ± 5.9), which has potential implications for the inflammatory markers. Nonetheless, numerous studies have presented similar average BMI values [38,39,40,41], which point to the complexity of controlling for such a variable when older age and higher BMI are closely confounded.
Another limitation of this study was the absence of a control group that received no treatment, which would have allowed for observation of changes in biomarker levels over time via natural history. This improvement could have been possible by having participants assigned to a wait-list control group and would have added a layer of information in comparing the various interventions. Additional work should be pursued in this area to gain further insight into the role of biomarkers and changes in clinical outcomes. Another limitation was the lack of a blood draw immediately after the first intervention session; this would have made the study more comparable to previous research in this article’s literature review section and could help form future research questions. However, on the contrary, the inclusion of later time points for clinical outcomes is a strength of this study since they support the association between baseline biomarkers and clinical outcomes. Last, confounders could have impacted the analysis results, such as medications, supplements, and other conditions which could contribute to the biomarker pool, even though the RCT design is generally accepted to address this potential issue.
In identifying relevant serum biomarkers, previous work suggests that panels of biomarkers may provide greater predictive power than any single biomarker alone [9]. Also, combining molecular biomarkers with clinical metrics may likely prove to be the most helpful approach in identifying those patients most expected to benefit from a given treatment. This combined approach represents a potential new avenue for sub-classifying patients and developing individualized treatment plans to address sub-group differences. Overall, the associations we observed do not point at robust, direct mechanisms but likely depend on a more comprehensive set of physiological and clinical interactions that are still not understood. More research is thus warranted in this area.
Conclusion
We found small correlations of vitamin D, CRP, NPY, and E-selectin with pain and disability at baseline and weak correlations of baseline vitamin D with improvement in outcomes following a four-week course of treatment with manipulative-related therapies. For acute and subacute LBP. We believe these data make an important contribution to the field of research on biomarkers and pain, suggesting that these serum biomarkers could have a potential role in further study of the mechanisms of prevalent LBP and prediction in related treatment outcomes and therefore warrant further evaluation. Future biomarkers research may help inform a personalized medicine approach to LBP management.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request and with a properly executed data use agreement.
Abbreviations
- NPY:
-
Neuropeptide Y
- TNFα:
-
Tumor necrosis factor-alpha
- SubP:
-
Substance P
- RANTES:
-
Regulated upon activation, normal t-cell expressed and presumably secreted
- CRP:
-
C-reactive protein
- ODI:
-
Oswestry Disability Index
- LBP:
-
Low back Pain
- RCT:
-
Randomized clinical trial
- BMI:
-
Body Mass Index
- EDTA:
-
Ethylene-diamine-tetraacetic acid
- CCL5:
-
C-C Motif Chemokine Ligand 5
References
The burden of musculoskeletal diseases in the United States. 2011.
Manchikanti L, Singh V, Falco FJE, Benyamin RM, Hirsch JA. Epidemiology of low back pain in adults. Neuromodulation. 2014;17(Suppl 2):3–10.
Davies C, Nitz AJ, Mattacola CG, Kitzman P, Howell D, Viele K, et al. Practice patterns when treating patients with low back pain: a survey of physical therapists. Physiother Theory Pract. 2014;30(6):399–408.
George SZ, Goertz C, Hastings SN, Fritz JM. Transforming low back pain care delivery in the United States. Pain. 2020;161(12):2667–73.
Deyo RA, Mirza SK, Turner JA, Martin BI. Overtreating chronic back pain: time to back off? J Am Board Fam Med. 2009;22(1):62–8.
Ghildayal N, Johnson PJ, Evans RL, Kreitzer MJ. Complementary and alternative medicine use in the US adult low Back pain population. Glob Adv Health Med. 2016;5(1):69–78.
Schneider M, Haas M, Glick R, Stevans J, Landsittel D. Comparison of spinal manipulation methods and usual medical Care for Acute and Subacute low Back Pain: a randomized clinical trial. Spine (Phila Pa 1976). 2015;40(4):209–17.
Lehtola V, Leinonen V, Gibbons S, Airaksinen O. LH. Sub-classification based specific movement control exercises are superior to general exercise in sub-acute low back pain when both are combined with manual therapy: a randomized controlled trial. BMC Musculoskelet Disord. 2016;17(1):135.
Sowa GA, Perera S, Bechara B, Agarwal V, Boardman J, Huang W, et al. Associations between serum biomarkers and pain and pain-related function in older adults with low back pain: a pilot study. J Am Geriatr Soc. 2014;62(11):2047–55.
Kovanur-Sampath K, Mani R, Cotter J, Gisselman AS, Tumilty S. Changes in biochemical markers following spinal manipulation-a systematic review and meta-analysis. Musculoskelet Sci Pract. 2017;29:120–31.
Chow N, Hogg-Johnson S, Mior S, Cancelliere C, Injeyan S, Teodorczyk-Injeyan J, et al. Assessment of Studies Evaluating Spinal Manipulative Therapy and Infectious Disease and Immune System Outcomes: A Systematic Review. JAMA Netw Open. 2021;4(4):e215493 Available from: https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2778522. [cited 2022 Apr 20].
Roy RA, Boucher JP, Comtois AS. Inflammatory response following a short-term course of chiropractic treatment in subjects with and without chronic low back pain. J Chiropr Med. 2010;9(3):107–14.
Degenhardt BF, Darmani NA, Johnson JC, Towns LC, Rhodes DCJ, Trinh C, et al. Role of osteopathic manipulative treatment in altering pain biomarkers: a pilot study. J Am Osteopath Assoc. 2007;107(9):387–400.
Ormos G, Mehrishi JN, Bakács T. Reduction in high blood tumor necrosis factor-alpha levels after manipulative therapy in 2 cervicogenic headache patients. J Manip Physiol Ther. 2009;32(7):586–91.
Lim YZ, Wang Y, Cicuttini FM, Hughes HJ, Chou L, Urquhart DM, et al. Association between inflammatory biomarkers and non-specific low Back pain: a systematic review. Clin J Pain [Internet]. 2020;36(5):379–89 Available from: https://pubmed.ncbi.nlm.nih.gov/31990692/. [cited 2022 Apr 20].
Morris P, Ali K, Merritt M, Pelletier J, Macedo LG. A systematic review of the role of inflammatory biomarkers in acute, subacute and chronic non-specific low back pain. BMC Musculoskelet Disord. 2020;21(1):1–12 Available from: https://bmcmusculoskeletdisord.biomedcentral.com/articles/10.1186/s12891-020-3154-3. [cited 2022 Apr 20].
Koes BW, van Tulder M, Lin CWC, Macedo LG, McAuley J, Maher C. An updated overview of clinical guidelines for the management of non-specific low back pain in primary care. Eur Spine J. 2010;19(12):2075–94 Available from: https://pubmed.ncbi.nlm.nih.gov/20602122/. [cited 2022 Jan 25].
Khan AN, Jacobsen HE, Khan J, Filippi CG, Levine M, Lehman RA, et al. Inflammatory biomarkers of low back pain and disc degeneration: a review. Ann N Y Acad Sci. 2017;1410(1):68 Available from: /pmc/articles/PMC5744892/. [cited 2022 Jan 27].
Teodorczyk-Injeyan JA, McGregor M, Triano JJ, Injeyan SH. Elevated Production of Nociceptive CC Chemokines and sE-Selectin in Patients With Low Back Pain and the Effects of Spinal Manipulation: A Nonrandomized Clinical Trial. Clin J Pain. 2018;34(1):68–75 Available from: https://pubmed.ncbi.nlm.nih.gov/29200015/. [cited 2022 Apr 21].
Zheng J, Zhang J, Zhang X, Guo Z, Wu W, Chen Z, et al. Reactive Oxygen Species Mediate Low Back Pain by Upregulating Substance P in Intervertebral Disc Degeneration. Oxid Med Cell Longev. 2021;2021 Available from: https://pubmed.ncbi.nlm.nih.gov/34093962/. [cited 2022 Apr 21].
Kanaujia V, Yadav R, Verma S, Jain S, Patra B, Neyaz O. Correlation between Vitamin D deficiency and non-specific chronic low back pain: A retrospective observational study. J Family Med Prim Care. 2021;10(2):893 Available from: https://pubmed.ncbi.nlm.nih.gov/34041094/. [cited 2022 Apr 21].
Xu HW, Zhang SB, Yi YY, Chen H, Hu T, Wang SJ, et al. Relationship between vitamin D and non-specific low Back pain may be mediated by inflammatory markers. Pain Physician. 2021;24(7):E1015–23 Available from: https://pubmed.ncbi.nlm.nih.gov/34704712/. [cited 2022 Apr 21].
Waddell G, Newton M, Henderson I, Somerville D, Main CJ. A fear-avoidance beliefs questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain. 1993;52(2):157–68.
Von Korff M, Deyo RA, Cherkin D, Barlow W. Back pain in primary care. Outcomes at 1 year. Spine (Phila Pa 1976). 1993;18(7):855–62.
Fairbank JC, Pynsent PB. The Oswestry disability index. Spine (Phila Pa 1976). 2000;25(22):2940–52 discussion 2952.
Klyne DM, Barbe MF, van den Hoorn W, Hodges PW. ISSLS PRIZE IN CLINICAL SCIENCE 2018: longitudinal analysis of inflammatory, psychological, and sleep-related factors following an acute low back pain episode-the good, the bad, and the ugly. Eur Spine J. 2018;27(4):763–77.
Klyne DM, Barbe MF, Hodges PW. Relationship between systemic inflammation and recovery over 12 months after an acute episode of low back pain. Spine J. 2022;22(2):214–25.
da Cruz Fernandes IM, Pinto RZ, Ferreira P, Lira FS. Low back pain, obesity, and inflammatory markers: exercise as potential treatment. J Exerc Rehabil. 2018;14(2):168–74.
Zadro J, Shirley D, Ferreira M, Carvalho-Silva AP, Lamb SE, Cooper C, et al. Mapping the association between vitamin D and low Back pain: a systematic review and Meta-analysis of observational studies. Pain Physician. 2017;20(7):611–40.
de Oliveira DL, Hirotsu C, Tufik S, Andersen ML. The interfaces between vitamin D, sleep and pain. J Endocrinol. 2017;234(1):R23–36.
Wu Z, Malihi Z, Stewart AW, Lawes CM, Scragg R. Effect of vitamin D supplementation on pain: a systematic review and Meta-analysis. Pain Physician. 2016;19(7):415–27.
Helde-Frankling M, Björkhem-Bergman L. Vitamin D in Pain Management. Int J Mol Sci. 2017;18(10):2170.
Iglar PJ, Hogan KJ. Vitamin D status and surgical outcomes: a systematic review. Patient Saf Surg. 2015;9(1):1–10 Available from: https://pssjournal.biomedcentral.com/articles/10.1186/s13037-015-0060-y. [cited 2022 Sep 2].
Schaaf S, Huang W, Perera S, Conley Y, Belfer I, Jayabalan P, et al. Association of Protein and Genetic Biomarkers With Response to Lumbar Epidural Steroid Injections in Subjects With Axial Low Back Pain. Am J Phys Med Rehabil. 2021;100(1):48 Available from: /pmc/articles/PMC8128510/. [cited 2022 Apr 21].
Hansen BB, Hansen P, Carrino JA, Fournier G, Rasti Z, Boesen M. Imaging in mechanical back pain: Anything new? Best Pract Res Clin Rheumatol. 2016;30(4):766–85 Available from: https://pubmed.ncbi.nlm.nih.gov/27931967/. [cited 2022 Apr 21].
Burgstaller JM, Schüffler PJ, Buhmann JM, Andreisek G, Winklhofer S, del Grande F, et al. Is There an Association Between Pain and Magnetic Resonance Imaging Parameters in Patients With Lumbar Spinal Stenosis? Spine (Phila Pa 1976). 2016;41(17):E1053–62 Available from: https://pubmed.ncbi.nlm.nih.gov/26953669/. [cited 2022 Apr 21].
Diaz-delCastillo M, Woldbye DPD, Heegaard AM. Neuropeptide Y and its Involvement in Chronic Pain. Neuroscience. 2018;387:162–9 Available from: https://pubmed.ncbi.nlm.nih.gov/28890052/. [cited 2022 Apr 21].
McIlroy S, Jadhakhan F, Bell D, Rushton A. Prediction of walking ability following posterior decompression for lumbar spinal stenosis. Eur Spine J. 2021;30(11):3307 Available from: /pmc/articles/PMC8550110/. [cited 2022 Apr 22].
Zhang Y, Mandelli F, Mündermann A, Nüesch C, Kovacs B, Schären S, et al. Association between fatty infiltration of paraspinal muscle, sagittal spinopelvic alignment and stenosis grade in patients with degenerative lumbar spinal stenosis. North Am Spine Soc J. 2021;5:100054 Available from: /pmc/articles/PMC8820068/. [cited 2022 Apr 22].
Mandelli F, Nüesch C, Zhang Y, Halbeisen F, Schären S, Mündermann A, et al. Assessing Fatty Infiltration of Paraspinal Muscles in Patients With Lumbar Spinal Stenosis: Goutallier Classification and Quantitative MRI Measurements. Front Neurol. 2021;12:656487 Available from: /pmc/articles/PMC8446197/. [cited 2022 Apr 22].
Akpinar B, Lin LJ, Bloom DA, Youm T. Concomitant lumbar spinal stenosis negatively affects outcomes after hip arthroscopy for Femoroacetabular impingement. Arthroscopy: the journal of Arthroscopic & Related. Surgery. 2021;37(7):2102–9.
Acknowledgements
Not Applicable.
Funding
This publication was made possible by grant number R00AT004196–03 from the National Center for Complementary and Integrative Health (NCCIH) at the National Institutes of Health, and the UPMC Rehabilitation Institute. Its contents are solely the authors’ responsibility and do not necessarily represent the official views of NCCIH. Further funding was obtained through the Virginia Kaufman pilot project program in pain research from the University of Pittsburgh.
Author information
Authors and Affiliations
Contributions
VTE analyzed and interpreted the data, drafted the manuscript, critically revised the manuscript for important intellectual content, and performed statistical analysis. NV conceptualized and designed the study, participated in acquisition of data and data management, critically revised the manuscript for important intellectual content, obtained funding, assisted with Administrative, Technical or Material Support, supervised. MS conceptualized and designed the study, participated in acquisition of data and data management, performed statistical analysis, analyzed and interpreted the data, critically revised the manuscript for important intellectual content, obtained funding, supervised. NW participated in acquisition of data and data management, critically revised the manuscript for important intellectual content, assisted with Administrative, Technical or Material Support. HW participated in acquisition of data and data management, critically revised the manuscript for important intellectual content, assisted with Administrative, Technical or Material Support. HM analyzed and interpreted the data, drafted the manuscript, critically revised the manuscript for important intellectual content, performed statistical analysis, and supervised. CM participated in acquisition of data and data management, critically revised the manuscript for important intellectual content, assisted with Administrative, Technical or Material Support, GS conceptualized and designed the study, participated in acquisition of data and data management, performed statistical analysis, analyzed and interpreted the data, critically revised the manuscript for important intellectual content, obtained funding, supervised. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The parent study was approved by the University of Pittsburgh Institutional Review Board (PRO10040327). Written informed consent was obtained from all study participants.
Consent for publication
Not Applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Tonelli Enrico, V., Schneider, M., Haas, M. et al. The association of biomarkers with pain and function in acute and subacute low back pain: a secondary analysis of an RCT. BMC Musculoskelet Disord 23, 1059 (2022). https://doi.org/10.1186/s12891-022-06027-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-022-06027-9