Abstract
Purpose
Previous studies have reported similar survival between segmentectomy and lobectomy for patients with small-sized non-small cell lung cancer. However, part of those patients were with adenocarcinoma in situ or minimally invasive adenocarcinoma, which were considered to have a favorable prognosis. We compared survival outcomes of patients with clinical N0 invasive lung adenocarcinomas of no more than 2 cm who underwent segmentectomy or lobectomy.
Methods
Between June 1, 2008, and May 31, 2018, 1018 patients with clinical N0 invasive lung adenocarcinomas of no more than 2 cm in diameter on thin-section chest CT scans were retrospectively included in this study. Of them, 214 underwent segmentectomy and 804 underwent lobectomy. Propensity-score matching of preoperative factors, such as gender, age, smoking status, forced expiratory volume in 1 s predicted%, tumor’s CT appearance, tumor size on CT scan and tumor location was used to compare survival outcomes of those patients receiving different surgical treatments. Cox proportional hazard regression model was used to identify independent prognostic factors. This study was approved by the Committee for Ethical Review of Research (Fudan University Shanghai Cancer Center IRB# 090977–1). Informed consent was waived because of the retrospective nature of this study.
Results
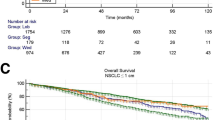
Average follow-up time was 42.5 months. Before matching, the lobectomy group had a shorter recurrence-free survival (P = 0.02), but similar overall survival (P = 0.60). After matching, no significant difference of overall survival or recurrence-free survival was found between the two groups (P = 0.70 and P = 0.40, respectively).
Conclusions
Our results suggest that segmentectomy achieved similar recurrence-free and overall survival compared with lobectomy for patients with clinical N0 invasive lung adenocarcinomas of no more than 2 cm. Therefore, segmentectomy could be an alternative approach. These results need to be further validated by randomized trials.





Similar content being viewed by others
References
Altorki NK, Wang X, Wigle D, Gu L, Darling G, Ashrafi AS, Landrenau R, Miller D, Liberman M, Jones DR, Keenan R, Conti M, Wright G, Veit LJ, Ramalingam SS, Kamel M, Pass HI, Mitchell JD, Stinchcombe T, Vokes E, Kohman LJ (2018) Perioperative mortality and morbidity after sublobar versus lobar resection for early-stage non-small-cell lung cancer: post-hoc analysis of an international, randomised, phase 3 trial (CALGB/Alliance 140503). Lancet Respir Med 6(12):915–924
Bedetti B, Bertolaccini L, Rocco R, Schmidt J, Solli P, Scarci M (2017) Segmentectomy versus lobectomy for stage I non-small cell lung cancer: a systematic review and meta-analysis. J Thorac Dis 9(6):1615–1623
Behera M, Owonikoko TK, Gal AA, Steuer CE, Kim S, Pillai RN, Khuri FR, Ramalingam SS, Sica GL (2016) Lung adenocarcinoma staging using the 2011 IASLC/ATS/ERS classification: a pooled analysis of adenocarcinoma in situ and minimally invasive adenocarcinoma. Clin Lung Cancer 17(5):e57–e64
Borczuk AC (2012) Assessment of invasion in lung adenocarcinoma classification, including adenocarcinoma in situ and minimally invasive adenocarcinoma. Mod Pathol 25(Suppl 1):S1–10
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68(6):394–424
Dai C, Shen J, Ren Y, Zhong S, Zheng H, He J, Xie D, Fei K, Liang W, Jiang G, Yang P, Petersen RH, Ng CS, Liu CC, Rocco G, Brunelli A, Shen Y, Chen C, He J (2016) Choice of surgical procedure for patients with non-small-cell lung cancer %3c/= 1 cm or %3e 1 to 2 cm among lobectomy, segmentectomy, and wedge resection: a population-based study. J Clin Oncol 34(26):3175–3182
Ginsberg RJ, Rubinstein LV (1995) Randomized trial of lobectomy versus limited resection for T1 N0 non-small cell lung cancer. Ann Thorac Surg 60(3):615–621
Goldstraw P, Chansky K, Crowley J, Rami-Porta R, Asamura H, Eberhardt WE, Nicholson AG, Groome P, Mitchell A, Bolejack V (2016) International Association for the Study of Lung Cancer S, Prognostic Factors Committee AB, Participating I, International Association for the Study of Lung Cancer S, Prognostic Factors Committee Advisory B, participating I. The IASLC lung cancer staging project: proposals for revision of the TNM stage groupings in the forthcoming (Eighth) edition of the TNM classification for lung cancer. J Thorac Oncol 11(1):39–51
Harpole DH, Herndon JE, Young WG, Wolfe WG, Sabiston DC (1995) Stage-I nonsmall cell lung-cancer: a multivariate-analysis of treatment methods and patterns of recurrence. Cancer 76(5):787–796
Hou H, Tapias LF, Gaissert HA, Muniappan A, Wright CD, Wain JC, Donahue DM, Morse CR, Mathisen DJ, Lanuti M (2015) Lymph node assessment and impact on survival in video-assisted thoracoscopic lobectomy or segmentectomy. Ann Thorac Surg 100(3):910–916
Kodama K, Higashiyama M, Okami J, Tokunaga T, Imamura F, Nakayama T, Inoue A, Kuriyama K (2016) Oncologic outcomes of segmentectomy versus lobectomy for clinical T1a N0 M0 non-small cell lung cancer. Ann Thorac Surg 101(2):504–511
Landreneau RJ, Normolle DP, Christie NA, Awais O, Wizorek JJ, Abbas G, Pennathur A, Shende M, Weksler B, Luketich JD, Schuchert MJ (2014) Recurrence and survival outcomes after anatomic segmentectomy versus lobectomy for clinical stage I non-small-cell lung cancer: a propensity-matched analysis. J Clin Oncol 32(23):2449–2455
Liang H, Liang W, Zhao L, Chen D, Zhang J, Zhang Y, Tang S, He J (2018) Robotic versus video-assisted lobectomy/segmentectomy for lung cancer: a meta-analysis. Ann Surg 268(2):254–259
Moon MH, Moon YK, Moon SW (2018) Segmentectomy versus lobectomy in early non-small cell lung cancer of 2 cm or less in size: a population-based study. Respirology 23(7):695–703
Nomori H, Shiraishi A, Cong Y, Sugimura H, Mishima S (2018) Differences in postoperative changes in pulmonary functions following segmentectomy compared with lobectomy. Eur J Cardiothorac Surg 53(3):640–647
Shimada Y, Saji H, Yoshida K, Kakihana M, Honda H, Nomura M, Usuda J, Kajiwara N, Ohira T, Ikeda N (2012) Pathological vascular invasion and tumor differentiation predict cancer recurrence in stage IA non-small-cell lung cancer after complete surgical resection. J Thorac Oncol 7(8):1263–1270
Sica G, Yoshizawa A, Sima CS, Azzoli CG, Downey RJ, Rusch VW, Travis WD, Moreira AL (2010) A grading system of lung adenocarcinomas based on histologic pattern is predictive of disease recurrence in stage I tumors. Am J Surg Pathol 34(8):1155–1162
Song CY, Sakai T, Kimura D, Tsushima T, Fukuda I (2018) Comparison of perioperative and oncological outcomes between video-assisted segmentectomy and lobectomy for patients with clinical stage IA non-small cell lung cancer: a propensity score matching study. J Thorac Dis 10(8):4891–4901
Suzuki K, Saji H, Aokage K, Watanabe SI, Okada M, Mizusawa J, Nakajima R, Tsuboi M, Nakamura S, Nakamura K, Mitsudomi T, Asamura H, West Japan Oncology G, Japan Clinical Oncology G (2019) Comparison of pulmonary segmentectomy and lobectomy: safety results of a randomized trial. J Thorac Cardiovasc Surg 158(3):895–907
Tsutani Y, Miyata Y, Nakayama H, Okumura S, Adachi S, Yoshimura M, Okada M (2013) Oncologic outcomes of segmentectomy compared with lobectomy for clinical stage IA lung adenocarcinoma: propensity score-matched analysis in a multicenter study. J Thorac Cardiovasc Surg 146(2):358–364
Tsutani Y, Miyata Y, Nakayama H, Okumura S, Adachi S, Yoshimura M, Okada M (2014) Appropriate sublobar resection choice for ground glass opacity-dominant clinical stage IA lung adenocarcinoma: wedge resection or segmentectomy. Chest 145(1):66–71
Widder J, Van De Wauwer C, Langendijk JA (2017) Lobectomy or sublobectomy for small non-small-cell lung cancer: the question remains. J Clin Oncol 35(5):572–573
Yoshizawa A, Motoi N, Riely GJ, Sima CS, Gerald WL, Kris MG, Park BJ, Rusch VW, Travis WD (2011) Impact of proposed IASLC/ATS/ERS classification of lung adenocarcinoma: prognostic subgroups and implications for further revision of staging based on analysis of 514 stage I cases. Mod Pathol 24(5):653–664
Funding
The study was supported by the National Natural Science Foundation of China (81930073), Shanghai Shenkang Hospital Development Center City Hospital Emerging Cutting-edge Technology Joint Research Project (SHDC12017102) and Shanghai Municipal Health Commission Key Discipline Project (2017ZZ02025 and 2017ZZ01019).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
This study was approved by the Committee for Ethical Review of Research (Fudan University Shanghai Cancer Center IRB# 090977–1).
Informed consent
Informed consent was waived because of the retrospective nature of this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wen, Z., Zhao, Y., Fu, F. et al. Comparison of outcomes following segmentectomy or lobectomy for patients with clinical N0 invasive lung adenocarcinoma of 2 cm or less in diameter. J Cancer Res Clin Oncol 146, 1603–1613 (2020). https://doi.org/10.1007/s00432-020-03180-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-020-03180-3