Abstract
Purpose
Achieving surgical resection is essential if patients with pancreatic ductal adenocarcinoma (PDAC) have a chance for cure. The objective of this study was to evaluate the effect of time to surgery on resection rates in patients with resectable PDAC.
Methods
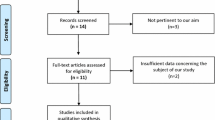
A systematic literature search was performed to identify studies reporting times to surgery and resection rates. Meta-regression models were then produced to assess the relationship between time to surgery and resection rates, using both intra- and inter-study comparisons.
Results
A total of 21 studies were included, comprising n = 2171 patients, with a pooled resection rate of 76%. Intra-study meta-analysis of the five studies that reported comparisons between patients with vs. without preoperative biliary drainage (PBD) or with long vs. short delays to surgery found earlier surgery to be associated with a significantly higher rate of resection (pooled odds ratio 1.93, 95% CI: 1.25–2.97, P = 0.003). Inter-study meta-regression across all studies found a tendency for resection rates to decline with increasing time from CT or ERCP to surgery (gradient − 0.13 log-odds per week, 95% CI − 0.28, 0.03, P = 0.100), although this did not reach statistical significance, in part due to considerable heterogeneity between studies.
Conclusion
Pathways to reduce the time to surgery, primarily by avoiding PBD, demonstrate significantly greater resection rates. Early surgery, including avoidance of PBD, not only provides patients with the benefit of avoiding harm associated with PBD but also with a greater chance of undergoing resection.





Similar content being viewed by others
Abbreviations
- CT:
-
Computed tomography
- CE:
-
Contrast-enhanced
- ERCP:
-
Endoscopic retrograde cholangio-pancreatography
- PDAC:
-
Pancreatic ductal adenocarcinoma
- PBD:
-
Preoperative biliary drainage
- NHS:
-
National health service
- RCTs:
-
Randomized controlled trials
References
Allen VB, Gurusamy KS, Takwoingi Y et al (2016) Diagnostic accuracy of laparoscopy following computed tomography (CT) scanning for assessing the resectability with curative intent in pancreatic and periampullary cancer. Cochrane Database Syst Rev 7:CD009323. https://doi.org/10.1002/14651858.CD009323.pub3
Fujioka S, Misawa T, Okamoto T, Gocho T, Futagawa Y, Ishida Y, Yanaga K (2007) Preoperative serum carcinoembryonic antigen and carbohydrate antigen 19-9 levels for the evaluation of curability and resectability in patients with pancreatic adenocarcinoma. J Hepatobiliary Pancreat Surg 14:539–544. https://doi.org/10.1007/s00534-006-1184-3
Manak E, Merkel S, Klein P, Papadopoulos T, Bautz WA, Baum U (2009) Resectability of pancreatic adenocarcinoma: assessment using multidetector-row computed tomography with multiplanar reformations. Abdom Imaging 34:75–80. https://doi.org/10.1007/s00261-007-9285-2
Valls C, Andía E, Sanchez A, Fabregat J, Pozuelo O, Quintero JC, Serrano T, Garcia-Borobia F, Jorba R (2002) Dual-phase helical CT of pancreatic adenocarcinoma: assessment of resectability before surgery. AJR Am J Roentgenol 178:821–826. https://doi.org/10.2214/ajr.178.4.1780821
Ellsmere J, Mortele K, Sahani D, Maher M, Cantisani V, Wells W, Brooks D, Rattner D (2005) Does multidetector-row CT eliminate the role of diagnostic laparoscopy in assessing the resectability of pancreatic head adenocarcinoma? Surg Endosc 19:369–373. https://doi.org/10.1007/s00464-004-8712-5
Kneuertz PJ, Cunningham SC, Cameron JL, Torrez S, Tapazoglou N, Herman JM, Makary MA, Eckhauser F, Wang J, Hirose K, Edil BH, Choti MA, Schulick RD, Wolfgang CL, Pawlik TM (2011) Palliative surgical management of patients with unresectable pancreatic adenocarcinoma: trends and lessons learned from a large, single institution experience. J Gastrointest Surg Off J Soc Surg Aliment Tract 15:1917–1927. https://doi.org/10.1007/s11605-011-1665-9
Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA, the PRISMA-P Group (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 349:g7647
Goossen K, Tenckhoff S, Probst P, Grummich K, Mihaljevic AL, Büchler MW, Diener MK (2018) Optimal literature search for systematic reviews in surgery. Langenbecks Arch Surg 403:119–129. https://doi.org/10.1007/s00423-017-1646-x
Green S (ed) (2011) HJ Cochrane handbook for systematic reviews of interventions version 5.1.0 [updated March 2011]. Cochrane Collab. Available from http://handbook.cochrane.org
Sterne JA, Hernán MA, Reeves BC et al (2016) ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 355:i4919. https://doi.org/10.1136/bmj.i4919
Eshuis WJ, van der Gaag NA, Rauws EAJ, van Eijck CHJ, Bruno MJ, Kuipers EJ, Coene PP, Kubben FJGM, Gerritsen JJGM, Greve JW, Gerhards MF, de Hingh IHJT, Klinkenbijl JH, Nio CY, de Castro SMM, Busch ORC, van Gulik TM, Bossuyt PMM, Gouma DJ (2010) Therapeutic delay and survival after surgery for cancer of the pancreatic head with or without preoperative biliary drainage. Ann Surg 252:840–849. https://doi.org/10.1097/SLA.0b013e3181fd36a2
Siddiqui AA, Mehendiratta V, Loren D, Hong SK, Kowalski T (2011) Fully covered self-expandable metal stents are effective and safe to treat distal malignant biliary strictures, irrespective of surgical resectability status. J Clin Gastroenterol 45:824–827. https://doi.org/10.1097/MCG.0b013e318211f96f
Ong SL, Garcea G, Thomasset SC, Mann CD, Neal CP, Abu Amara M, Dennison AR, Berry DP (2008) Surrogate markers of resectability in patients undergoing exploration of potentially resectable pancreatic adenocarcinoma. J Gastrointest Surg Off J Soc Surg Aliment Tract 12:1068–1073. https://doi.org/10.1007/s11605-007-0422-6
Brown EG, Canter RJ, Bold RJ (2015) Preoperative CA 19-9 kinetics as a prognostic variable in radiographically resectable pancreatic adenocarcinoma. J Surg Oncol 111:293–298. https://doi.org/10.1002/jso.23812
Cazauran J-B, Perinel J, Kepenekian V, el Bechwaty M, Nappo G, Pioche M, Ponchon T, Adham M (2017) Unnecessary preoperative biliary drainage: impact on perioperative outcomes of resectable periampullary tumors. Langenbecks Arch Surg 402:1187–1196. https://doi.org/10.1007/s00423-017-1635-0
Olsson G, Frozanpor F, Lundell L, Enochsson L, Ansorge C, del Chiaro M, Reuterwall-Hansson M, Shetye A, Arnelo U (2017) Preoperative biliary drainage by plastic or self-expandable metal stents in patients with periampullary tumors: results of a randomized clinical study. Endosc Int Open 5:E798–E808. https://doi.org/10.1055/s-0043-110565
Roberts KJ, Prasad P, Steele Y, Marcon F, Faulkner T, Cilliers H, Dasari B, Abradelo M, Marudanayagam R, Sutcliffe RP, Muiesan P, Mirza DF, Isaac J (2017) A reduced time to surgery within a “fast track” pathway for periampullary malignancy is associated with an increased rate of pancreatoduodenectomy. HPB 19:713–720. https://doi.org/10.1016/j.hpb.2017.04.011
van der Gaag NA, Rauws EAJ, van Eijck CHJ, Bruno MJ, van der Harst E, Kubben FJGM, Gerritsen JJGM, Greve JW, Gerhards MF, de Hingh IHJT, Klinkenbijl JH, Nio CY, de Castro SMM, Busch ORC, van Gulik TM, Bossuyt PMM, Gouma DJ (2010) Preoperative biliary drainage for cancer of the head of the pancreas. N Engl J Med 362:129–137. https://doi.org/10.1056/NEJMoa0903230
Song TJ, Lee JH, Lee SS, Jang JW, Kim JW, Ok TJ, Oh DW, Park DH, Seo DW, Lee SK, Kim MH, Kim SC, Kim CN, Yun SC (2016) Metal versus plastic stents for drainage of malignant biliary obstruction before primary surgical resection. Gastrointest Endosc 84:814–821. https://doi.org/10.1016/j.gie.2016.04.018
Yu J, Blackford AL, Dal Molin M et al (2015) Time to progression of pancreatic ductal adenocarcinoma from low-to-high tumour stages. Gut 64:1783–1789. https://doi.org/10.1136/gutjnl-2014-308653
McLean SR, Karsanji D, Wilson J et al (2013) The effect of wait times on oncological outcomes from periampullary adenocarcinomas. J Surg Oncol 107:853–858. https://doi.org/10.1002/jso.23338
Marchegiani G, Andrianello S, Perri G, Secchettin E, Maggino L, Malleo G, Bassi C, Salvia R (2018) Does the surgical waiting list affect pathological and survival outcome in resectable pancreatic ductal adenocarcinoma? HPB 20:411–417. https://doi.org/10.1016/j.hpb.2017.10.017
Kulkarni GS, Urbach DR, Austin PC, Fleshner NE, Laupacis A (2009) Longer wait times increase overall mortality in patients with bladder cancer. J Urol 182:1318–1324. https://doi.org/10.1016/j.juro.2009.06.041
Langenbach MR, Schmidt J, Neumann J, Zirngibl H (2003) Delay in treatment of colorectal cancer: multifactorial problem. World J Surg 27:304–308. https://doi.org/10.1007/s00268-002-6678-9
Sainsbury R, Johnston C, Haward B (1999) Effect on survival of delays in referral of patients with breast-cancer symptoms: a retrospective analysis. Lancet Lond Engl 353:1132–1135. https://doi.org/10.1016/s0140-6736(99)02374-0
Sanjeevi S, Ivanics T, Lundell L, Kartalis N, Andrén-Sandberg Å, Blomberg J, del Chiaro M, Ansorge C (2016) Impact of delay between imaging and treatment in patients with potentially curable pancreatic cancer. Br J Surg 103:267–275. https://doi.org/10.1002/bjs.10046
Seo HK, Hwang DW, Park SY, Park Y, Lee SJ, Lee JH, Song KB, Lee YJ, Kim SC (2018) The survival impact of surgical waiting time in patients with resectable pancreatic head cancer. Ann Hepato-Biliary-Pancreat Surg 22:405–411. https://doi.org/10.14701/ahbps.2018.22.4.405
Versteijne E, Vogel JA, Besselink MG, Busch ORC, Wilmink JW, Daams JG, van Eijck CHJ, Groot Koerkamp B, Rasch CRN, van Tienhoven G, the Dutch Pancreatic Cancer Group (2018) Meta-analysis comparing upfront surgery with neoadjuvant treatment in patients with resectable or borderline resectable pancreatic cancer. Br J Surg 105:946–958. https://doi.org/10.1002/bjs.10870
Marchegiani G, Andrianello S, Malleo G, de Gregorio L, Scarpa A, Mino-Kenudson M, Maggino L, Ferrone CR, Lillemoe KD, Bassi C, Castillo CFD, Salvia R (2017) Does size matter in pancreatic cancer?: reappraisal of tumour dimension as a predictor of outcome beyond the TNM. Ann Surg 266:142–148. https://doi.org/10.1097/SLA.0000000000001837
Glant JA, Waters JA, House MG et al (2011) Does the interval from imaging to operation affect the rate of unanticipated metastasis encountered during operation for pancreatic adenocarcinoma? Surgery 150:607–616. https://doi.org/10.1016/j.surg.2011.07.048
Raman SP, Reddy S, Weiss MJ, Manos LL, Cameron JL, Zheng L, Herman JM, Hruban RH, Fishman EK, Wolfgang CL (2015) Impact of the time interval between MDCT imaging and surgery on the accuracy of identifying metastatic disease in patients with pancreatic cancer. AJR Am J Roentgenol 204:W37–W42. https://doi.org/10.2214/AJR.13.12439
Funding
The study was funded by institutional means.
Author information
Authors and Affiliations
Contributions
PCM: study design, literature search, data extraction, writing the manuscript; JH: study design, statistical analysis, writing the manuscript; CK: literature search, data extraction, critical revision of the manuscript; MK, RP: literature search, interpretation of data, critical revision of the manuscript; KJR: study design, interpretation of data, writing the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Not applicable due to the nature of the study design.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Supplementary figure 1
(DOCX 56 kb)
Supplementary figure 2
(DOCX 22 kb)
Rights and permissions
About this article
Cite this article
Müller, P.C., Hodson, J., Kuemmerli, C. et al. Effect of time to surgery in resectable pancreatic cancer: a systematic review and meta-analysis. Langenbecks Arch Surg 405, 293–302 (2020). https://doi.org/10.1007/s00423-020-01893-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-020-01893-0