Abstract
Purpose
To clarify the prognostic value of the number of metastatic lymph nodes (mLNs) in squamous and non-squamous histologies among women with node-positive cervical cancer.
Methods
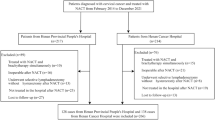
One hundred ninety-one node-positive cervical cancer patients who had undergone radical hysterectomy plus systematic pelvic and para-aortic lymphadenectomy followed by concurrent radiochemotherapy were retrospectively reviewed. The prognostic value of the number of mLNs was investigated in squamous cell carcinoma (SCC) v (n = 148) and non-SCC (n = 43) histologies separately with univariate log-rank test and multivariate Cox regression analyses.
Results
In SCC cohort, mLNs > 2 was significantly associated with decreased 5-year disease-free survival (DFS) [hazard ratio (HR) = 2.06; 95% confidence interval (CI) 1.03–4.09; p = 0.03) and overall survival (OS) (HR = 2.35, 95% CI 1.11–4.99; p = 0.02). However mLNs > 2 had no significant impact on 5-year DFS and 5-year OS rates in non-SCC cohort (p = 0.94 and p = 0.94, respectively). We stratified the entire study population as SCC with mLNs ≤ 2, SCC with mLNs > 2, and non-SCC groups. Thereafter, we compared survival outcomes. The non-SCC group had worse 5-year OS (46.8% vs. 85.3%, respectively; p < 0.001) and 5-year DFS rates (31.6% vs. 82.2%, respectively; p < 0.001) when compared to those of the SCC group with mLNs ≤ 2. However, the non-SCC group and the SCC group with mLNs > 2 had similar 5-year OS (46.8% vs. 65.5%, respectively; p = 0.16) and 5-year DFS rates (31.6% vs. 57.5%, respectively; p = 0.06).
Conclusion
Node-positive cervical cancer patients who have non-SCC histology as well as those who have SCC histology with mLNs > 2 seem to have worse survival outcomes when compared to women who have SCC histology with mLNs ≤ 2.


Similar content being viewed by others
Availability of data and material
Available on request of editor or reviewers.
References
Zhou J, Zhang WW, Wu SG et al (2017) The prognostic value of histologic subtype in node-positive early-stage cervical cancer after hysterectomy and adjuvant radiotherapy. Int J Surg 44:1–6. https://doi.org/10.1016/j.ijsu.2017.05.074
Sakuragi N, Satoh C, Takeda N et al (1999) Incidence and distribution pattern of pelvic and paraaortic lymph node metastasis in patients with Stages LB, IIA, and IIB cervical carcinoma treated with radical hysterectomy. Cancer 85:1547–1554. https://doi.org/10.1002/(SICI)1097-0142(19990401)85:7%3c1547::AID-CNCR16%3e3.0.CO;2-2
Bhatla N, Aoki D, Sharma DN, Sankaranarayanan R (2018) Cancer of the cervix uteri. Int J Gynecol Obstet 143:22–36. https://doi.org/10.1002/ijgo.12611
Hosaka M, Watari H, Mitamura T et al (2011) Survival and prognosticators of node-positive cervical cancer patients treated with radical hysterectomy and systematic lymphadenectomy. Int J Clin Oncol 16:33–38. https://doi.org/10.1007/s10147-010-0123-0
Yan DD, Tang Q, Tu YQ et al (2019) A comprehensive analysis of the factors of positive pelvic lymph nodes on survival of cervical cancer patients with 2018 FIGO stage IIIC1p. Cancer Manag Res 11:4223–4230. https://doi.org/10.2147/cmar.s204154
Park JY, Kim DY, Kim JH et al (2010) Further stratification of risk groups in patients with lymph node metastasis after radical hysterectomy for early-stage cervical cancer. Gynecol Oncol 117:53–58. https://doi.org/10.1016/j.ygyno.2009.12.006
Zhou J, Wu SG, Sun JY et al (2017) Incorporation of the number of positive lymph nodes leads to better prognostic discrimination of node-positive early stage cervical cancer. Oncotarget 8(16):26057–26065
Nakanishi T, Ishikawa H, Suzuki Y et al (2000) A comparison of prognoses of pathologic stage Ib adenocarcinoma and squamous cell carcinoma of the uterine cervix. Gynecol Oncol 79:289–293. https://doi.org/10.1006/gyno.2000.5935
Kodama J, Seki N, Masahiro S et al (2010) Prognostic factors in stage IB–IIB cervical adenocarcinoma patients treated with radical hysterectomy and pelvic lymphadenectomy. J Surg Oncol 101:413–417. https://doi.org/10.1002/jso.21499
Liu Y, Zhao LJ, Li MZ et al (2015) The number of positive pelvic lymph nodes and multiple groups of pelvic lymph node metastasis influence prognosis in stage IA–IIB cervical squamous cell carcinoma. Chin Med J (Engl) 128:2084–2089. https://doi.org/10.4103/0366-6999.161372
Zhou J, Zhang WW, Wu SG et al (2017) The impact of examined lymph node count on survival in squamous cell carcinoma and adenocarcinoma of the uterine cervix. Cancer Manag Res 9:315–322. https://doi.org/10.2147/CMAR.S141335
Pecorelli S (2009) Revised FIGO staging for carcinoma of the vulva, cervix, and endometrium. Int J Gynaecol Obstet 105:103–104
Aslan K, Meydanli MM, Oz M et al (2020) The prognostic value of lymph node ratio in stage IIIC cervical cancer patients triaged to primary treatment by radical hysterectomy with systematic pelvic and para-aortic lymphadenectomy. J Gynecol Oncol. https://doi.org/10.3802/jgo.2020.31.e1
Sakuragi N, Takeda N, Hareyama H et al (2000) A multivariate analysis of blood vessel and lymph vessel invasion as predictors of ovarian and lymph node metastases in patients with cervical carcinoma. Cancer 88:2578–2583
Kurman RJ, Carcangiu ML, Herrington CS (2014) WHO classification of tumours of female reproductive organs. WHO press, 4th edn, vol 6
Pieterse QD, Kenter GG, Gaarenstroom KN et al (2007) The number of pelvic lymph nodes in the quality control and prognosis of radical hysterectomy for the treatment of cervical cancer. Eur J Surg Oncol 33:216–221. https://doi.org/10.1016/j.ejso.2006.09.037
Verleye L, Vergote I, Reed N et al (2009) Quality assurance for radical hysterectomy for cervical cancer: the view of the European Organization for Research and Treatment of Cancer-Gynecological Cancer Group (EORTC-GCG). Ann Oncol 20:1631–1638
Cibula D, Planchamp F, Fischerova D et al (2020) European Society of Gynaecological Oncology quality indicators for surgical treatment of cervical cancer. Int J Gynecol Cancer 30:3–14. https://doi.org/10.1136/ijgc-2019-000878
Peters WA, Liu PY, Barrett RJ et al (2000) Concurrent chemotherapy and pelvic radiation therapy compared with pelvic radiation therapy alone as adjuvant therapy after radical surgery in high-risk early-stage cancer of the cervix. J Clin Oncol 18:1606–1613. https://doi.org/10.1200/JCO.2000.18.8.1606
Barter JF, Soong SJ, Shingleton HM et al (1989) Complications of combined radical hysterectomy-postoperative radiation therapy in women with early stage cervical cancer. Gynecol Oncol 32:292–296. https://doi.org/10.1016/0090-8258(89)90627-6
Cibula D, Pötter R, Planchamp F et al (2018) The European Society of Gynaecological Oncology/European Society for Radiotherapy and Oncology/European Society of Pathology guidelines for the management of patients with cervical cancer. Radiother Oncol 127:404–416. https://doi.org/10.1016/j.radonc.2018.03.003
Potter ME, Alvarez RD, Shingleton HM et al (1990) Early invasive cervical cancer with pelvic lymph node involvement: to complete or not to complete radical hysterectomy? Gynecol Oncol 37:78–81. https://doi.org/10.1016/0090-8258(90)90312-9
Bremer GL, van der Putten HW, Dunselman GA, de Haan J (1992) Early stage cervical cancer: aborted versus completed radical hysterectomy. Eur J Obstet Gynecol Reprod Biol 47:147–151. https://doi.org/10.1016/0028-2243(92)90045-Z
Suprasert P, Srisomboon J, Charoenkwan K et al (2005) Outcomes of abandoned radical hysterectomy in patients with stages IB–IIA cervical cancer found to have positive nodes during the operation. Int J Gynecol Cancer 15:498–502. https://doi.org/10.1111/j.1525-1438.2005.15315.x
Gray HJ, Seifert E, Saly Rosas VG et al (2010) The abandoned radical hysterectomy for cervical cancer: clinical predictors and outcomes. Obstet Gynecol Int 2010:1–6. https://doi.org/10.1155/2010/743794
Richard SD, Krivak TC, Castleberry A et al (2008) Survival for stage IB cervical cancer with positive lymph node involvement: a comparison of completed vs. abandoned radical hysterectomy. Gynecol Oncol 109:43–48. https://doi.org/10.1016/j.ygyno.2007.12.002
Gubbala PK, Laios A, Wang Z et al (2016) Routine intraoperative frozen section examination to minimize bimodal treatment in early-stage cervical cancer. Int J Gynecol Cancer 26:1148–1153. https://doi.org/10.1097/IGC.0000000000000738
Garg G, Shah JP, Toy EP et al (2011) Intra-operative detection of nodal metastasis in early stage cervical cancer: a survey of the practice patterns of SGO members. Gynecol Oncol 121:143–147. https://doi.org/10.1016/j.ygyno.2010.12.337
Ganesan R, Brown LJR, Kehoe S et al (2013) The role of frozen sections in gynaecological oncology: survey of practice in the United Kingdom. Eur J Obstet Gynecol Reprod Biol 166:204–208. https://doi.org/10.1016/j.ejogrb.2012.10.024
Liu B, Gao S, Li S (2017) A comprehensive comparison of CT, MRI, positron emission tomography or positron emission tomography/CT, and diffusion weighted imaging-MRI for detecting the lymph nodes metastases in patients with cervical cancer: a meta-analysis based on 67 studies. Gynecol Obstet Invest 82:209–222
Zigras T, Lennox G, Willows K et al (2017) Early cervical cancer: current dilemmas of staging and surgery. Curr Oncol, Rep, p 19
Petrelli F, De Stefani A, Raspagliesi F et al (2014) Radiotherapy with concurrent cisplatin-based doublet or weekly cisplatin for cervical cancer: a systematic review and meta-analysis. Gynecol Oncol 134:166–171
Mabuchi S, Isohashi F, Yokoi T et al (2016) A phase II study of postoperative concurrent carboplatin and paclitaxel combined with intensity-modulated pelvic radiotherapy followed by consolidation chemotherapy in surgically treated cervical cancer patients with positive pelvic lymph nodes. Gynecol Oncol 141:240–246. https://doi.org/10.1016/j.ygyno.2016.02.011
Author information
Authors and Affiliations
Contributions
KA protocol/project development,data collection or management, data analysis, manuscript writing/editing, approved the version to be published. AH protocol/project development, manuscript writing/editing, approved the version to be published. HA data collection or management, manuscript writing/editing, approved the version to be published; MMM protocol/project development, data analysis, manuscript writing/editing, approved the version to be published. AA protocol/project development, manuscript writing/editing, approved the version to be published.
Corresponding author
Ethics declarations
Conflict of interest
None.
Ethics approval
The Institutional Review Board of Başkent University approved this study (IRB Approval Number:nKA 19/427).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent to publish
Additional informed consent was obtained from all individual participants for whom identifying information is included in this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Aslan, K., Haberal, A., Akıllı, H. et al. Prognostic value of the number of the metastatic lymph nodes in locally early-stage cervical cancer: squamous cell carcinoma versus non-squamous cell carcinoma. Arch Gynecol Obstet 304, 1279–1289 (2021). https://doi.org/10.1007/s00404-021-06030-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-021-06030-w