Abstract
Background
The surgical extent and indication for treatment in patients with papillary thyroid microcarcinoma (PTMC) remain a controversial issue. The aim of this study was to investigate the predictive factor for contralateral occult carcinoma in patients with unilateral PTMC by preoperative ultrasonographic and pathological features.
Methods
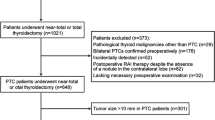
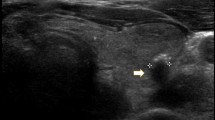
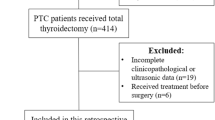
Of the total patients who underwent thyroidectomy, 455 patients with PTMC confined to one unilateral lobe as diagnosed using preoperative ultrasonography (US) were enrolled in the study. Occult contralateral carcinoma was defined as tumor foci in the contralateral lobe that was not detected preoperatively, but was detected pathologically. All patients underwent preoperative US review to investigate the US features of PTMC such as laterality, location, size, internal component, echogenicity, margin, calcification shape, multifocality, bilaterality, extrathyroidal extension, and location with respect to the trachea. Clinicopathological data were also analyzed.
Results
Of the total of 455 patients who underwent total thyroidectomy for preoperatively detected unilateral PTMC, 71 patients (15.6 %) had contralateral occult carcinoma. Clinicopathological characteristics did not significantly differ between patients with and without contralateral occult carcinoma. Multivariate analysis showed that the absence of a well-defined margin and the presence of a probably benign nodule in the contralateral lobe were independent predictive factors for contralateral occult carcinoma in patients with unilateral PTMC in preoperative US images.
Conclusion
We demonstrated that an absence of a well-defined margin and the presence of a probably benign nodule in the contralateral lobe were independent predictive factors for contralateral occult carcinoma in patients with unilateral PTMC in preoperative US. The prediction of contralateral occult carcinoma in unilateral PTMC using preoperative US features could be useful for determining the optical extent of surgery.
Similar content being viewed by others
References
DeLellis R, Lloyd R, Heitz P et al (2004) Thyroid and parathyroid tumours: papillary carcinoma. In: World health organization classification of tumours: pathology and genetics of tumours of endocrine organs, IARC Press, Lyon, pp 49–123
Davies L, Welch HG (2006) Increasing incidence of thyroid cancer in the United States, 1973-2002. JAMA 295:2164–2167
Leenhardt L, Grosclaude P, Cherie-Challine L (2004) Increased incidence of thyroid carcinoma in france: a true epidemic or thyroid nodule management effects? report from the French Thyroid Cancer Committee. Thyroid 14:1056–1060
Vickery AL Jr, Wang CA, Walker AM (1987) Treatment of intrathyroidal papillary carcinoma of the thyroid. Cancer 60:2587–2595
Hay ID, Hutchinson ME, Gonzalez-Losada T et al (2008) Papillary thyroid microcarcinoma: a study of 900 cases observed in a 60-year period. Surgery 144:980–987. doi:10.1016/j.surg.2008.08.035 discussion 987–988
Mercante G, Frasoldati A, Pedroni C et al (2009) Prognostic factors affecting neck lymph node recurrence and distant metastasis in papillary microcarcinoma of the thyroid: results of a study in 445 patients. Thyroid 19:707–716
Ross DS, Litofsky D, Ain KB et al (2009) Recurrence after treatment of micropapillary thyroid cancer. Thyroid 19:1043–1048
Cooper DS, Doherty GM, Haugen BR et al (2009) Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 19:1167–1214
National Comprehensive Cancer Network (2013) Clinical practice guidelines in oncology: thyroid carcinoma. http://www.nccn.org/professionals/physician_gls/f_guidelines.asp
Koo BS, Lim HS, Lim YC et al (2010) Occult contralateral carcinoma in patients with unilateral papillary thyroid microcarcinoma. Ann Surg Oncol 17:1101–1105
Connor MP, Wells D, Schmalbach CE (2011) Variables predictive of bilateral occult papillary microcarcinoma following total thyroidectomy. Otolaryngol Head Neck Surg 144:210–215
Moon WJ, Jung SL, Lee JH et al (2008) Benign and malignant thyroid nodules: US differentiation–multicenter retrospective study. Radiology 247:762–770
Horvath E, Majlis S, Rossi R et al (2009) An ultrasonogram reporting system for thyroid nodules stratifying cancer risk for clinical management. J Clin Endocrinol Metab 94:1748–1751
Park JY, Lee HJ, Jang HW et al (2009) A proposal for a thyroid imaging reporting and data system for ultrasound features of thyroid carcinoma. Thyroid 19:1257–1264
Kim EK, Park CS, Chung WY et al (2002) New sonographic criteria for recommending fine-needle aspiration biopsy of nonpalpable solid nodules of the thyroid. AJR Am J Roentgenol 178:687–691
Alexander EK, Hurwitz S, Heering JP et al (2003) Natural history of benign solid and cystic thyroid nodules. Ann Intern Med 138:315–318
Bellantone R, Lombardi CP, Raffaelli M et al (2004) Management of cystic or predominantly cystic thyroid nodules: the role of ultrasound-guided fine-needle aspiration biopsy. Thyroid 14:43–47
Braga M, Cavalcanti TC, Collaco LM et al (2001) Efficacy of ultrasound-guided fine-needle aspiration biopsy in the diagnosis of complex thyroid nodules. J Clin Endocrinol Metab 86:4089–4091
McHenry CR, Slusarczyk SJ, Khiyami A (1999) Recommendations for management of cystic thyroid disease. Surgery 126:1167–1171 discussion 1171-1162
Kwak JY, Kim EK, Youk JH et al (2008) Extrathyroid extension of well-differentiated papillary thyroid microcarcinoma on US. Thyroid 18:609–614
Kwak JY, Kim EK, Kim MJ et al (2009) Papillary microcarcinoma of the thyroid: predicting factors of lateral neck node metastasis. Ann Surg Oncol 16:1348–1355
Lupi C, Giannini R, Ugolini C et al (2007) Association of BRAF V600E mutation with poor clinicopathological outcomes in 500 consecutive cases of papillary thyroid carcinoma. J Clin Endocrinol Metab 92:4085–4090
Noguchi S, Yamashita H, Murakami N et al (1996) Small carcinomas of the thyroid. A long-term follow-up of 867 patients. Arch Surg 131:187–191
Ito Y, Miyauchi A (2015) Nonoperative management of low-risk differentiated thyroid carcinoma. Curr Opin Oncol 27:15–20
Sugitani I, Fujimoto Y, Yamada K (2014) Association between serum thyrotropin concentration and growth of asymptomatic papillary thyroid microcarcinoma. World J Surg 38:673–678. doi:10.1007/s00268-013-2335-8
Wang W, Zhao W, Wang H et al (2012) Poorer prognosis and higher prevalence of BRAF (V600E) mutation in synchronous bilateral papillary thyroid carcinoma. Ann Surg Oncol 19:31–36
Pasieka JL, Thompson NW, McLeod MK et al (1992) The incidence of bilateral well-differentiated thyroid cancer found at completion thyroidectomy. World J Surg 16:711–716. doi:10.1007/BF02067365
Pitt SC, Sippel RS, Chen H (2009) Contralateral papillary thyroid cancer: does size matter? Am J Surg 197:342–347
Kim GR, Kim MH, Moon HJ et al (2013) Sonographic characteristics suggesting papillary thyroid carcinoma according to nodule size. Ann Surg Oncol 20:906–913
Hoang JK, Lee WK, Lee M et al (2007) US Features of thyroid malignancy: pearls and pitfalls. Radiographics 27:847–860 discussion 861-845
Shattuck TM, Westra WH, Ladenson PW et al (2005) Independent clonal origins of distinct tumor foci in multifocal papillary thyroid carcinoma. N Engl J Med 352:2406–2412
Wang W, Wang H, Teng X et al (2010) Clonal analysis of bilateral, recurrent, and metastatic papillary thyroid carcinomas. Hum Pathol 41:1299–1309
McCarthy RP, Wang M, Jones TD et al (2006) Molecular evidence for the same clonal origin of multifocal papillary thyroid carcinomas. Clin Cancer Res 12:2414–2418
Jovanovic L, Delahunt B, McIver B et al (2008) Most multifocal papillary thyroid carcinomas acquire genetic and morphotype diversity through subclonal evolution following the intra-glandular spread of the initial neoplastic clone. J Pathol 215:145–154
Zhao Q, Ming J, Liu C et al (2013) Multifocality and total tumor diameter predict central neck lymph node metastases in papillary thyroid microcarcinoma. Ann Surg Oncol 20:746–752
Ito Y, Higashiyama T, Takamura Y et al (2007) Long-term follow-up for patients with papillary thyroid carcinoma treated as benign nodules. Anticancer Res 27:1039–1043
Iacobone M, Jansson S, Barczynski M et al (2014) Multifocal papillary thyroid carcinoma—a consensus report of the European Society of Endocrine Surgeons (ESES). Langenbecks Arch Surg 399:141–154
Ito Y, Tomoda C, Uruno T et al (2004) Papillary microcarcinoma of the thyroid: how should it be treated? World J Surg 28:1115–1121. doi:10.1007/s00268-004-7644-5
Pellegriti G, Scollo C, Lumera G et al (2004) Clinical behavior and outcome of papillary thyroid cancers smaller than 1.5 cm in diameter: study of 299 cases. J Clin Endocrinol Metab 89:3713–3720
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Lee, Y.C., Eun, Y.G., Sohn, YM. et al. Predictive Factors for Occult Contralateral Carcinoma in Patients with Unilateral Papillary Thyroid Microcarcinoma by Preoperative Ultrasonographic and Pathological Features. World J Surg 39, 1736–1741 (2015). https://doi.org/10.1007/s00268-015-3024-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-015-3024-6