Abstract
Background
Renal hyperparathyroidism (rHPT) almost inevitably develops in pediatric patients with end-stage chronic kidney disease (CKD) and may require parathyroidectomy (PTX) despite intensified conservative therapy. Long-term duration of uncontrolled rHPT may result in disabling osteodystrophy and vascular calcifications. Only a few reports on children undergoing PTX for rHPT are available and mainly consist of case reports with short follow-up periods. To study this entity, we analyzed the course of 23 pediatic patients who underwent PTX for rHPT.
Methods
Twenty-three patients with a mean age of 15 years and who underwent PTX for rHPT between 1986 and 2006 were evaluated. Surgical indications and techniques, specific postoperative management, and follow-up courses are described.
Results
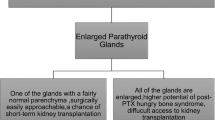
Preoperative mean serum (s-) calcium was 2.7 ± 0.05 mmol/L (normal range = 2.2–2.7 mmol/L); s-phosphate was 1.8 ± 0.1 mmol/L (normal range = 0.8–1.6 mmol/L), and mean intact parathyroid hormone (PTH) level was 1240.1 ± 160.1 pg/ml (normal range = 11–65 pg/ml). Twenty-one patients underwent initial PTX and two patients underwent reoperative PTX. Total PTX with parathyroid autotransplantation (AT) was performed in 18 patients. In three patients less than four parathyroid glands were identified and no AT was performed consecutively. Postoperatively, no complications with respect to bleeding or vocal cord damage were recorded. The postoperative values of s-calcium, s-phosphate, and PTH decreased to or below normal range (s-calcium = 2.0 ± 0.1 mmol/L, s-phosphate = 1.2 ± 0.1 mmol/L, PTH = 50.1 ± 11.2 pg/ml). All 15 children below the age of 15 years required calcium intravenously. Follow-up was obtained in all patients 69.6 ± 11.4 months after PTX. Bone pain resolved in all previously symptomatic patients. S-calcium was 2.2 ± 0.2 mmol/L, s-phosphate was 1.4 ± 0.3 mmol/L, and PTH was 90.2 ± 21.5 pg/ml. No patient required repeated parathyroid autografting, and only one underwent an explantation of his AT six years after initial PTX.
Conclusion
Total PTX with AT in pediatric patients with rHPT is a safe and effective procedure. It should be considered if rHPT is refractory to conservative treatment, in view of the risk of potentially lethal vascular calcifications developing in the majority of adults with childhood onset of CKD.


Similar content being viewed by others
References
Frei U, Schober-Halstenberg HJ (2006) Summary of the Annual Report on Dialysis Treatment and Renal Transplantation in Germany for 2005/2006. QuaSi-Niere 14(5):1085–1090
Ardissino G, Dacco V, Testa S, et al. (2003) Epidemiology of chronic renal failure in children: data from the ItalKid project. Pediatrics 111(4 Pt 1):e382–e387
Zachariou Z, Buhr H, von Herbay A, et al. (1995) Preoperative diagnostics and surgical management of tertiary hyperparathyroidism after chronic renal failure in a child. Eur J Pediatr Surg 5(5):288–291
Sanchez CP (2003) Secondary hyperparathyroidism in children with chronic renal failure: pathogenesis and treatment. Paediatr Drugs 5(11):763–776
Klaus G, Watson A, Edefonti A, et al. (2006) Prevention and treatment of renal osteodystrophy in children on chronic renal failure: European guidelines. Pediatr Nephrol 21(2):151–159
Berard E, Crosca G, Broyer M, et al. (1989) Parathyroidectomy in children with renal failure. Retrospective study of 17 cases. Arch Fr Pediatr 46(6):417–424
National Kidney Foundation (2007) Counahan-Barratt method to calculate GFR in children and adolescents. Available at http://www.kidney.org/professionals/kdoqi/gfr_calculatorPed.cfm. Accessed 20 May 2007
Nelson AW, Mackinnon B, Traynor J, et al. (2006) The relationship between serum creatinine and estimated glomerular filtration rate: implications for clinical practice. Scott Med J 51(4):5–9
Kuizon BD, Goodman WG, Juppner H, et al. (1998) Diminished linear growth during intermittent calcitriol therapy in children undergoing CCPD. Kidney Int 53(1):205–211
Schmitt CP, Ardissino G, Testa S, et al. (2003) Growth in children with chronic renal failure on intermittent versus daily calcitriol. Pediatr Nephrol 18(5):440–444
National Kidney Foundation (2005) Kidney Disease Outcomes Quality Intitiative (K/DOQI) clinical practice guidelines for bone metabolism and disease in children with chronic kidney disease. Am J Kidney Dis 46(Suppl 1):xxx-xxx
Storms LE, Chicella MF, Dice JE (2006) Sevelamer therapy for pediatric end-stage renal disease. Pharmacotherapy 26(3):410–413
Pieper AK, Haffner D, Hoppe B, et al. (2006) A randomized crossover trial comparing sevelamer with calcium acetate in children with CKD. Am J Kidney Dis 47(4):625–635
Seeherunvong W, Nwobi O, Abitbol CL, et al. (2006) Paricalcitol versus calcitriol treatment for hyperparathyroidism in pediatric hemodialysis patients. Pediatr Nephrol 21(10):1434–1439
Chang W, Tu C, Chen TH, et al. (1999) Expression and signal transduction of calcium-sensing receptors in cartilage and bone. Endocrinology 140(12):5883–5893
National Institutes of Health, Cinacalcet (Sensipar TM): a brief review. Available at http://clinicalcenter.nih.gov/phar/updates/pdf/pharmacyupdatemayjun04.pdf. Pharmacy Update May/June 2004
Riley TN, DeRuiter J (2004) What are the actions of cinacalcet hydrochloride (Sensipar) in the treatment of secondary hyperparathyroidism? US Pharm 29(12):HS8–HS16
Amgen Inc. (2004) Prescribing information for Sensipar™ (Cinacalcet HCl) tablets
Yang JY, Yao Y (2004) Analysis of 1268 patients with chronic renal failure in childhood: a report from 91 hospitals in China from 1990 to 2002. Zhonghua Er Ke Za Zhi 42(10):724–730
Firor HV, Moore ES, Levitsky LL, et al. (1972) Parathyroidectomy in children with chronic renal failure. J Pediatr Surg 7(5):565–572
Fine RN (1973) Severe renal osteodystrophy (ROD) in small children: treatment with total parathyroidectomy (PTX). Pediatr Res 7(1):45–67
Talwalkar YB, Puri HC, Hawker CC, et al. (1979) Parathyroid autotransplantation in renal osteodystrophy. Am J Dis Child 133(9):901–905
Moazam F, Orak JK, Fennell RS III, et al. (1984) Total parathyroidectomy and autotransplantation for tertiary hyperparathyroidism in children with chronic renal failure. J Pediatr Surg 19(4):389–393
Martinez L, Alonso A, Meseguer MC, et al. (1997) [Surgical treatment of tertiary hyperparathyroidism in childhood]. Cir Pediatr 10(1):13–17
Ross AJ III (1991) Parathyroid surgery in children. Prog Pediatr Surg 26:48–59
Jofre R, Lopez Gomez JM, Menarguez J, et al. (2003) Parathyroidectomy: whom and when? Kidney Int Suppl 85:S97–100
Zahiri K, Hachim K, Fatihi EM, et al. (2002) Calcium needs in hemodialyzed-parathyroidectomized patients. Ann Med Intern (Paris) 153(7):433–439
Davenport A, Stearns MP (2007) Administration of pamidronate helps prevent immediate postparathyroidectomy hungry bone syndrome. Nephrology (Carlton) 12(4):386–390
Oh J, Wunsch R, Turzer M, et al. (2002) Advanced coronary and carotid arteriopathy in young adults with childhood-onset chronic renal failure. Circulation 106(1):100–105
Salusky IB, Foley J, Nelson P, et al. (1991) Aluminum accumulation during treatment with aluminum hydroxide and dialysis in children and young adults with chronic renal disease. N Engl J Med 324(8):527–531
Civilibal M, Caliskan S, Oflaz H, et al. (2007) Traditional and “new” cardiovascular risk markers and factors in pediatric dialysis patients. Pediatr Nephrol 22:1021-1029
Civilibal M, Caliskan S, Adaletli I, et al. (2006) Coronary artery calcifications in children with end-stage renal disease. Pediatr Nephrol 21(10):1426–1433
Querfeld U (2004) The clinical significance of vascular calcification in young patients with end-stage renal disease. Pediatr Nephrol 19(5):478–484
Author information
Authors and Affiliations
Corresponding author
Additional information
K. Schlosser and C. P. Schmitt contributed equally to this work.
Rights and permissions
About this article
Cite this article
Schlosser, K., Schmitt, C.P., Bartholomaeus, J.E. et al. Parathyroidectomy for Renal Hyperparathyroidism in Children and Adolescents. World J Surg 32, 801–806 (2008). https://doi.org/10.1007/s00268-007-9318-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-007-9318-6