Abstract
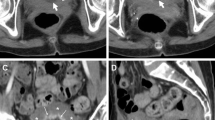
Involvement of the urinary tract and genital organs is not uncommon in patients affected with Crohn’s disease (CD). Occurring in both sexes, uro-gynecological complications are often clinically unsuspected because of the dominant intestinal or systemic symptoms. Knowledge of their manifestations and cross-sectional imaging appearances is necessary to recognize and report them, since correct medical or surgical treatment choice with appropriate specialist consultation allows to prevent further complications. Besides uncomplicated urinary tract infections that usually do not require imaging, urolithiasis and pyelonephritis represent the most commonly encountered urinary disorders: although very useful, use of computed tomography (CT) should be avoided whenever possible, to limit lifetime radiation exposure. Hydronephrosis due to ureteral inflammatory entrapment and enterovesical fistulization may result from penetrating CD, and require precise imaging assessment with contrast-enhanced CT to ensure correct surgical planning. Representing the majority of genital complication, ano- and rectovaginal fistulas and abscesses frequently complicate perianal inflammatory CD and are comprehensively investigated with high-resolution perianal MRI acquired with phased-array coils, high-resolution T2-weighted sequences and intravenous contrast. Finally, rare gynecological manifestations including internal genital fistulas, vulvar and male genital involvement are discussed.









Similar content being viewed by others
References
Rimola J, Rodriguez S, Cabanas ML, et al. (2011) MRI of Crohn’s disease: from imaging to pathology. Abdom Imaging. doi:10.1007/s00261-011-9797-7.
Van Assche G, Dignass A, Reinisch W, et al. (2010) The second European evidence-based consensus on the diagnosis and management of Crohn’s disease: special situations. J Crohns Colitis 4:63–101
Maccioni F, Colaiacomo MC, Stasolla A, et al. (2002) Value of MRI performed with phased-array coil in the diagnosis and pre-operative classification of perianal and anal fistulas. Radiol Med 104:58–67
Halligan S, Stoker J (2006) Imaging of fistula in ano. Radiology 239:18–33
Szurowska E, Wypych J, Izycka-Swieszewska E (2007) Perianal fistulas in Crohn’s disease: MRI diagnosis and surgical planning: MRI in fistulazing perianal Crohn’s disease. Abdom Imaging 32:705–718
Torkzad MR, Karlbom U (2010) MRI for assessment of anal fistula. Insights Imaging 1:62–71
Ruffolo C, Angriman I, Scarpa M, et al. (2006) Urologic complications in Crohn’s disease: suspicion criteria. Hepatogastroenterology 53:357–360
Ben-Ami H, Ginesin Y, Behar DM, et al. (2002) Diagnosis and treatment of urinary tract complications in Crohn’s disease: an experience over 15 years. Can J Gastroenterol 16:225–229
De La Poza G, Lopez-Sanroman A, Taxonera C, et al. (2011) Genital fistulas in female Crohn’s disease patients. Clinical characteristics and response to therapy. J Crohns Colitis. doi:10.1016/j.crohns.2011.08.015.
Feller ER, Ribaudo S, Jackson ND (2001) Gynecologic aspects of Crohn’s disease. Am Fam Physician 64:1725–1728
Sato S, Sasaki I, Naito H, et al. (1999) Management of urinary complications in Crohn’s disease. Surg Today 29:713–717
Andersson H, Bosaeus I, Fasth S, et al. (1987) Cholelithiasis and urolithiasis in Crohn’s disease. Scand J Gastroenterol 22:253–256
Eisner BH, McQuaid JW, Hyams E, et al. (2011) Nephrolithiasis: what surgeons need to know. AJR Am J Roentgenol 196:1274–1278
Kroeker KI, Lam S, Birchall I, et al. (2011) Patients with IBD are exposed to high levels of ionizing radiation through CT scan diagnostic imaging: a five-year study. J Clin Gastroenterol 45:34–39
Craig WD, Wagner BJ, Travis MD (2008) Pyelonephritis: radiologic–pathologic review. Radiographics 28:255–277
Stunell H, Buckley O, Feeney J, et al. (2007) Imaging of acute pyelonephritis in the adult. Eur Radiol 17:1820–1828
Martina MC, Campanino PP, Caraffo F, et al. (2010) Dynamic magnetic resonance imaging in acute pyelonephritis. Radiol Med 115:287–300
Ueno Y, Tanaka S, Kanao H, et al. (2006) A case of Crohn’s disease with hydronephrosis caused by ureteropelvic junction obstruction. Eur J Gastroenterol Hepatol 18:1015–1018
Ben-Ami H, Lavy A, Behar DM, et al. (2000) Left hydronephrosis caused by Crohn disease successfully treated conservatively. Am J Med Sci 320:286–287
Siminovitch JM, Fazio VW (1980) Ureteral obstruction secondary to Crohn’s disease: a need for ureterolysis? Am J Surg 139:95–98
Kruglik GD, Neiman HL, Sparberg M, et al. (1977) Urological complications of regional enteritis. Gastrointest Radiol 1:375–378
Solem CA, Loftus EV Jr, Tremaine WJ, et al. (2002) Fistulas to the urinary system in Crohn’s disease: clinical features and outcomes. Am J Gastroenterol 97:2300–2305
Wong-You-Cheong JJ, Woodward PJ, Manning MA, et al. (2006) From the archives of the AFIP: inflammatory and nonneoplastic bladder masses: radiologic–pathologic correlation. Radiographics 26:1847–1868
Yamamoto T, Keighley MR (2000) Enterovesical fistulas complicating Crohn’s disease: clinicopathological features and management. Int J Colorectal Dis 15:211–215 (discussion 216–217)
McNamara MJ, Fazio VW, Lavery IC, et al. (1990) Surgical treatment of enterovesical fistulas in Crohn’s disease. Dis Colon Rectum 33:271–276
Sou S, Yao T, Matsui T, et al. (1999) Preoperative detection of occult enterovesical fistulas in patients with Crohn’s disease: efficacy of oral or rectal administration of indocyanine green solution. Dis Colon Rectum 42:266–270
Kingsland CR, Alderman B (1991) Crohn’s disease of the vulva. J R Soc Med 84:236–237
Andreani SM, Ratnasingham K, Dang HH, et al. (2010) Crohn’s disease of the vulva. Int J Surg 8:2–5
Maconi G, Ardizzone S, Greco S, et al. (2007) Transperineal ultrasound in the detection of perianal and rectovaginal fistulae in Crohn’s disease. Am J Gastroenterol 102:2214–2219
Maun D, Vine A, Slater G (2006) Ileosalpingeal fistula: an unusual complication of Crohn’s disease. Mt Sinai J Med 73:1115–1116
Pai D, Dillman JR, Mahani MG, et al. (2011) MRI of vulvar Crohn disease. Pediatr Radiol 41:537–541
Leu S, Sun PK, Collyer J, et al. (2009) Clinical spectrum of vulva metastatic Crohn’s disease. Dig Dis Sci 54:1565–1571
Madnani NA, Desai D, Gandhi N, et al. (2011) Isolated Crohn’s disease of the vulva. Indian J Dermatol Venereol Leprol 77:342–344
Reyes M, Borum M (2009) Severe case of genital and perianal cutaneous Crohn’s disease. Inflamm Bowel Dis 15:1125–1126
Yamaguchi M, Kujiraoka Y, Saida Y, et al. (2001) Prostatic abscess in young males: a rare complication of Crohn’s disease. Abdom Imaging 26:423–424
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tonolini, M., Villa, C., Campari, A. et al. Common and unusual urogenital Crohn’s disease complications: spectrum of cross-sectional imaging findings. Abdom Imaging 38, 32–41 (2013). https://doi.org/10.1007/s00261-012-9876-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-012-9876-4