Abstract
Introduction and hypothesis
Defecatory dysfunction is a relatively common and challenging problem among women and one that practicing pelvic reconstructive surgeons and gynecologists deal with frequently. A subset of defecatory dysfunction includes obstructed defecation, which can have multiple causes, one of which is descending perineum syndrome (DPS).
Methods
A literature search was performed to identify the pathophysiology, diagnosis, and management of DPS.
Results
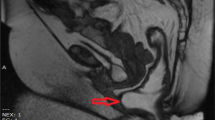
Although DPS has been described in the literature for many decades, it is still uncommonly diagnosed and difficult to manage. A high index of suspicion combined with physical examination consistent with excess perineal descent, patient symptom assessment, and imaging in the form of defecography are required for the diagnosis to be accurately made. Primary management options of DPS include conservative measures consisting of bowel regimens and biofeedback. Although various surgical approaches have been described in limited case series, no compelling evidence can be demonstrated at this point to support surgical intervention.
Conclusions
Knowledge of DPS is essential for the practicing pelvic reconstructive surgeon to make a timely diagnosis, avoid harmful treatments, and initiate therapy early on.








Similar content being viewed by others
References
Porter NH (1962) A physiological study of the pelvic floor in rectal prolapse. Ann R Coll Surg Engl 31:379–404
Parks AG, Porter NH, Hardcastle J (1966) The syndrome of the descending perineum. Proc R Soc Med 59:477–482
Hardcastle JD (1969) The descending perineum syndrome. Practitioner 203:612–619
Shorvon PJ, McHugh S, Diamant NE, Somers S, Stevenson GW (1989) Defecography in normal volunteers: results and implications. Gut 30:1737–1749
Mahieu P, Pringot J, Bodart P (1984) Defecography. I. Description of a new procedure and results in normal patients. Gastrointest Radiol 9:247–251
Ekberg O, Nylander G, Fork FT (1985) Defecography. Radiology 155:45–48
Bartram CI, Turnbull GK, Lennard-Jones JE (1988) Evacuation proctography: an investigation of rectal expulsion in 20 subjects without defecatory disturbance. Gastrointest Radiol 13:72–80
Faccioli N, Comai A, Mainardi P, Perandini S, Moore F, Pozzi-Mucelli R (2010) Defecography: a practical approach. Diagn Interv Radiol 16:209–216
Harewood GC, Coulie B, Camilleri M, Rath-Harvey D, Pemberton JH (1999) Descending perineum syndrome: audit of clinical and laboratory features and outcome of pelvic floor retraining. Am J Gastroenterol 94:126–130
Choi JS, Wexner SD, Nam YS, Mavrantonis C, Salum MR, Yamaguchi T, Weiss EG, Nogueras JJ, Yu CF (2000) Intraobserver and interobserver measurements of the anorectal angle and perineal descent in defecography. Dis Colon Rectum 43:1121–1126
Jorge JM, Ger GC, Gonzalez L, Wexner SD (1994) Patient position during cinedefecography. Influence on perineal descent and other measurements. Dis Colon Rectum 37:927–931
Landmann RG, Wexner SD (2008) Paradoxical puborectalis contraction and increased perineal descent. Clin Colon Rectal Surg 21:138–145
Armañanzas L, Arroyo A, Ruiz-Tovar J, López A, Santos J, Moya P, Gómez MA, Candela F, Calpena R (2015) Chronic idiopathic anal pain. Results of a diagnostic-therapeutic protocol in a colorectal referral unit. Cir Esp 93:34–38
Pucciani F, Boni D, Perna F, Bassotti G, Bellini M (2005) Descending perineum syndrome: are abdominal hysterectomy and bowel habits linked? Dis Colon Rectum 48:2094–2099
Pemberton JH (1990) Anorectal and pelvic floor disorders: putting physiology into practice. J Gastroenterol Hepatol 5:127–143
Henry MM, Parks AG, Swash M (1982) The pelvic floor musculature in the descending perineum syndrome. Br J Surg 69:470–472
Bartolo DC, Read NW, Jarratt JA, Read MG, Donnelly TC, Johnson AG (1983) Differences in anal sphincter function and clinical presentation in patients with pelvic floor descent. Gastroenterology 85:68–75
Read NW, Bartolo DC, Read MG, Hall J, Haynes WG, Johnson AG (1983) Differences in anorectal manometry between patients with haemorrhoids and patients with descending perineum syndrome: implications for management. Br J Surg 70:656–659
Womack NR, Morrison JF, Williams NS (1986) The role of pelvic floor denervation in the aetiology of idiopathic faecal incontinence. Br J Surg 73:404–407
Palit S, Lunniss PJ, Scott SM (2012) The physiology of human defecation. Dig Dis Sci 57:1445–1464
Ambrose S, Keighley MR (1985) Outpatient measurement of perineal descent. Ann R Coll Surg Engl 67:306–308
Chang J, Chung SS (2012) An analysis of factors associated with increased perineal descent in women. J Korean Soc Coloproctol 28:195–200
Baek HN, Hwang YH, Jung YH (2010) Clinical significance of perineal descent in pelvic outlet obstruction diagnosed by using defecography. J Korean Soc Coloproctol 26:395–401
Sunderland S (1978) Nerves and nerve injuries. Churchill Livingstone, New York, pp 62–66
Henry MM, Parks AG, Swash M (1980) The anal reflex in idiopathic faecal incontinence: an electrophysiological study. Br J Surg 67:781–783
Wall EJ, Massie JB, Kwan MK, Rydevik BL, Myers RR, Garfin SR (1992) Experimental stretch neuropathy. Changes in nerve conduction under tension. J Bone Joint Surg (Br) 74:126–129
Ho YH, Goh HS (1995) The neurophysiological significance of perineal descent. Int J Colorectal Dis 10:107–111
Kiff ES, Barnes PR, Swash M (1984) Evidence of pudendal neuropathy in patients with perineal descent and chronic straining at stool. Gut 25:1279–1282
Jorge JM, Wexner SD, Ehrenpreis ED, Nogueras JJ, Jagelman DG (1993) Does perineal descent correlate with pudendal neuropathy? Dis Colon Rectum 36:475–483
Vaccaro CA, Wexner SD, Teoh TA, Choi SK, Cheong DM, Salanga VD (1995) Pudendal neuropathy is not related to physiologic pelvic outlet obstruction. Dis Colon Rectum 38:630–634
Oettle GJ, Roe AM, Bartolo DC, Mortensen NJ (1985) What is the best way of measuring perineal descent? A comparison of radiographic and clinical methods. Br J Surg 72:999–1001
Mellgren A, Bremmer S, Johansson C, Dolk A, Udén R, Ahlbäck SO, Holmström B (1994) Defecography. Results of investigations in 2,816 patients. Dis Colon Rectum 37:1133–1141
Varma MG, Hart SL, Brown JS, Creasman JM, Van Den Eeden SK, Thom DH (2008) Obstructive defecation in middle-aged women. Dig Dis Sci 53:2702–2709
Yang A, Mostwin JL, Rosenshein NB, Zerhouni EA (1991) Pelvic floor descent in women: dynamic evaluation with fast MR imaging and cinematic display. Radiology 179:25–33
Lamb GM, de Jode MG, Gould SW, Spouse E, Birnie K, Darzi A, Gedroyc WM (2000) Upright dynamic MR defaecating proctography in an open configuration MR system. Br J Radiol 73:152–155
Mortele KJ, Fairhurst J (2007) Dynamic MR defecography of the posterior compartment: indications, techniques and MRI features. Eur J Radiol 61:462–472
Goei R, Kemerink G (1990) Radiation dose in defecography. Radiology 176:137–139
Bertschinger KM, Hetzer FH, Roos JE, Treiber K, Marincek B, Hilfiker PR (2002) Dynamic MR imaging of the pelvic floor performed with patient sitting in an open-magnet unit versus with patient supine in a closed-magnet unit. Radiology 223:501–508
Foti PV, Farina R, Riva G, Coronella M, Fisichella E, Palmucci S, Racalbuto A, Politi G, Ettorre GC (2013) Pelvic floor imaging: comparison between magnetic resonance imaging and conventional defecography in studying outlet obstruction syndrome. Radiol Med 118:23–39
Vanbeckevoort D, Van Hoe L, Oyen R, Ponette E, De Ridder D, Deprest J (1999) Pelvic floor descent in females: comparative study of colpocystodefecography and dynamic fast MR imaging. J Magn Reson Imaging 9:373–377
Kelvin FM, Maglinte DD, Hale DS, Benson JT (2000) Female pelvic organ prolapse: a comparison of triphasic dynamic MR imaging and triphasic fluoroscopic cystocolpoproctography. AJR Am J Roentgenol 174:81–88
Healy JC, Halligan S, Reznek RH, Watson S, Bartram CI, Phillips R, Armstrong P (1997) Dynamic MR imaging compared with evacuation proctography when evaluating anorectal configuration and pelvic floor movement. Am J Roentgenol 169:775–779
Schoenenberger AW, Debatin JF, Guldenschuh I, Hany TF, Steiner P, Krestin GP (1998) Dynamic MR defecography with a superconducting, open-configuration MR system. Radiology 206:641–646
Flusberg M, Sahni VA, Erturk SM, Mortele KJ (2011) Dynamic MR defecography: assessment of the usefulness of the defecation phase. Am J Roentgenol 196:394–399
Solopova AE, Hetzer FH, Marincek B, Weishaupt D (2008) MR defecography: prospective comparison of two rectal enema compositions. Am J Roentgenol 190:118–124
Andromanakos N, Skandalakis P, Troupis T, Filippou D (2006) Constipation of anorectal outlet obstruction: pathophysiology, evaluation and management. J Gastroenterol Hepatol 21:638–646
El-Nashar SA, Occhino JA, Trabuco E, Gebhart J, Klingele C (2014) Descending perineum syndrome: a fresh look at an interesting and complex pelvic floor disorder. J Minim Invasive Gynecol 21:S16–S17
Bartolo DC, Roe AM, Virjee J, Mortensen NJ, Locke-Edmunds JC (1988) An analysis of rectal morphology in obstructed defaecation. Int J Colorectal Dis 3:17–22
Khaikin M, Wexner SD (2006) Treatment strategies in obstructed defecation and fecal incontinence. World J Gastroenterol 12:3168–3173
Schey R, Cromwell J, Rao SS (2012) Medical and surgical management of pelvic floor disorders affecting defecation. Am J Gastroenterol 107:1624–1633
Guillemot F, Bouche B, Gower-Rousseau C, Chartier M, Wolschies E, Lamblin MD, Harbonnier E, Cortot A (1995) Biofeedback for the treatment of fecal incontinence. Long-term clinical results. Dis Colon Rectum 38:393–397
Dailianas A, Skandalis N, Rimikis MN, Koutsomanis D, Kardasi M, Archimandritis A (2000) Pelvic floor study in patients with obstructive defecation: influence of biofeedback. J Clin Gastroenterol 30:176–180
Beco J, Antolak S (2010) Posterior perineal support during defecation, descending perineum syndrome, pudendal neuropathy and anal fissures. Tech Coloproctol 14:193–194
Cundiff GW, Harris RL, Coates K, Low VH, Bump RC, Addison WA (1997) Abdominal sacral colpoperineopexy: a new approach for correction of posterior compartment defects and perineal descent associated with vaginal vault prolapse. Am J Obstet Gynecol 177:1345–1353
Link RE, Su LM, Bhayani SB, Wright EJ (2004) Laparoscopic sacral colpoperineopexy for treatment of perineal body descent and vaginal vault prolapse. Urology 64:145–147
Alves-Ferreira PC, Gurland B, Zutshi M, Hull T (2012) Perineal descent does not imply a more severe clinical disorder. Colorectal Dis 14:1372–1379
Beco J (2008) Interest of retro-anal levator plate myorrhaphy in selected cases of descending perineum syndrome with positive anti-sagging test. BMC Surg 8:1–13
Boccasanta P, Venturi M, Salamina G, Cesana BM, Bernasconi F, Roviaro G (2004) New trends in the surgical treatment of outlet obstruction: clinical and functional results of two novel transanal stapled techniques from a randomised controlled trial. Int J Colorectal Dis 19:359–369
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Rights and permissions
About this article
Cite this article
Chaudhry, Z., Tarnay, C. Descending perineum syndrome: a review of the presentation, diagnosis, and management. Int Urogynecol J 27, 1149–1156 (2016). https://doi.org/10.1007/s00192-015-2889-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-015-2889-0