Abstract
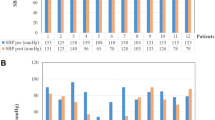
Postprandial hypotension (PPH) is a major clinical problem in patients with autonomic failure such as that observed in multiple system atrophy (MSA). The pathophysiology of PPH remains unclear, although autonomic dysfunction and gastrointestinal vasoactive peptides have been suspected to participate in its pathogenesis. We measured blood pressure and plasma levels of glucose, insulin, noradrenaline, neurotensin, glucagon-like peptide (GLP)-1 and GLP-2 before and after meal ingestion in 24 patients with MSA to reveal the roles of the autonomic nervous system and gastrointestinal vasoactive peptides in PPH. We performed a second meal-ingestion test by administering acarbose to evaluate the effects of acarbose (an α-glucosidase inhibitor) on PPH and vasoactive peptides in 14 patients with MSA and PPH. We also evaluated blood pressure responses to the head-up tilt test and heart rate variability in all the patients. Severities of PPH and orthostatic hypotension were significantly correlated. Patients with PPH had significantly worse orthostatic hypotension and lower heart rate variability than those without PPH. Postprandial GLP-1 secretion was higher in patients with PPH than in those without PPH. No significant differences were observed in the postprandial increases in plasma levels of glucose, insulin, noradrenaline, neurotensin or GLP-2. Acarbose significantly attenuated postprandial hypotension and tended to decrease GLP-2 secretion. Our results indicate that autonomic failure is involved in the pathogenesis of PPH and confirm that acarbose has a preventive effect against PPH in patients with MSA. Decreased postprandial secretion of GLP-2, which increases intestinal blood pooling, may attenuate PPH in patients with MSA.

Similar content being viewed by others
References
Gilman S, Wenning GK, Low PA, Brooks DJ, Mathias CJ, Trojanowski JQ, Wood NW, Colosimo C, Durr A, Fowler CJ, Kaufmann H, Klockgether T, Lees A, Poewe W, Quinn N, Revesz T, Robertson D, Sandroni P, Seppi K, Vidailhet M (2008) Second consensus statement on the diagnosis of multiple system atrophy. Neurology 71:670–676
Mathias CJ, Holly E, Armstrong E, Shareef M, Bannister R (1991) The influence of food on postural hypotension in three groups with chronic autonomic failure-clinical and therapeutic implications. Journal of Neurology, Neurosurgery and Psychiatry 54:726–730
Thomaides T, Bleasdale-Barr K, Chaudhuri KR, Pavitt D, Marsden CD, Mathias CJ (1993) Cardiovascular and hormonal responses to liquid food challenge in idiopathic Parkinson’s disease, multiple system atrophy, and pure autonomic failure. Neurology 43:900–904
Micieli G, Martignoni E, Cavallini A, Sandrini G, Nappi G (1987) Postprandial and orthostatic hypotension in Parkinson’s disease. Neurology 37:386–393
Sasaki E, Kitaoka H, Ohsawa N (1992) Postprandial hypotension in patients with non-insulin-dependent diabetes mellitus. Diabetes Research and Clinical Practice 18:113–121
Jansen RW, Lipsitz LA (1995) Postprandial hypotension: epidemiology, pathophysiology, and clinical management. Annals of Internal Medicine 122:286–295
Lipsitz LA, Ryan SM, Parker JA, Freeman R, Wei JY, Goldberger AL (1993) Hemodynamic and autonomic nervous system responses to mixed meal ingestion in healthy young and old subjects and dysautonomic patients with postprandial hypotension. Circulation 87:391–400
Mathias CJ, da Costa DF, Fosbraey P, Bannister R, Wood SM, Bloom SR, Christensen NJ (1989) Cardiovascular, biochemical and hormonal changes during food-induced hypotension in chronic autonomic failure. Journal of the Neurological Sciences 94:255–269
Teramoto S, Akishita M, Fukuchi Y, Toba K, Ouchi Y (1997) Assessment of autonomic nervous function in elderly subjects with or without postprandial hypotension. Hypertension Research 20:257–261
Kooner JS, Raimbach S, Watson L, Bannister R, Peart S, Mathias CJ (1989) Relationship between splanchnic vasodilation and postprandial hypotension in patients with primary autonomic failure. Journal of Hypertension. Supplement 7:S40–S41
Puvi-Rajasingham S, Smith GD, Akinola A, Mathias CJ (1998) Hypotensive and regional haemodynamic effects of exercise, fasted and after food, in human sympathetic denervation. Clin Sci (Lond) 94:49–55
Takamori M, Hirayama M, Kobayashi R, Ito H, Mabuchi N, Nakamura T, Hori N, Koike Y, Sobue G (2007) Altered venous capacitance as a cause of postprandial hypotension in multiple system atrophy. Clinical Autonomic Research 17:20–25
Jansen RW, Peeters TL, Van Lier HJ, Hoefnagels WH (1990) The effect of oral glucose, protein, fat and water loading on blood pressure and the gastrointestinal peptides VIP and somatostatin in hypertensive elderly subjects. European Journal of Clinical Investigation 20:192–198
Brubaker PL, Minireview Drucker DJ (2004) Glucagon-like peptides regulate cell proliferation and apoptosis in the pancreas, gut, and central nervous system. Endocrinology 145:2653–2659
Green BD, Hand KV, Dougan JE, McDonnell BM, Cassidy RS, Grieve DJ (2008) GLP-1 and related peptides cause concentration-dependent relaxation of rat aorta through a pathway involving KATP and cAMP. Archives of Biochemistry and Biophysics 478:136–142
Bremholm L, Hornum M, Henriksen BM, Larsen S, Holst JJ (2009) Glucagon-like peptide-2 increases mesenteric blood flow in humans. Scandinavian Journal of Gastroenterology 44:314–319
Deniz M, Bozkurt A, Kurtel H (2007) Mediators of glucagon-like peptide 2-induced blood flow: responses in different vascular sites. Regulatory Peptides 142:7–15
Stephens J, Stoll B, Cottrell J, Chang X, Helmrath M, Burrin DG (2006) Glucagon-like peptide-2 acutely increases proximal small intestinal blood flow in TPN-fed neonatal piglets. American Journal of Physiology: Regulatory, Integrative and Comparative Physiology 290:R283–R289
Maruta T, Komai K, Takamori M, Yamada M (2006) Voglibose inhibits postprandial hypotension in neurologic disorders and elderly people. Neurology 66:1432–1434
Hammer RA, Matsumoto BK, Blei AT, Pearl G, Ingram H (1988) Local effect of neurotensin on canine ileal blood flow, and its release by luminal lipid. Scandinavian Journal of Gastroenterology 23:445–449
Shibao C, Gamboa A, Diedrich A, Dossett C, Choi L, Farley G, Biaggioni I (2007) Acarbose, an alpha-glucosidase inhibitor, attenuates postprandial hypotension in autonomic failure. Hypertension 50:54–56
Sasaki E, Goda K, Nagata K, Kitaoka H, Ohsawa N, Hanafusa T (2001) Acarbose improved severe postprandial hypotension in a patient with diabetes mellitus. Journal of Diabetes and Its Complications 15:158–161
Freeman R, Wieling W, Axelrod FB, Benditt DG, Benarroch E, Biaggioni I, Cheshire WP, Chelimsky T, Cortelli P, Gibbons CH, Goldstein DS, Hainsworth R, Hilz MJ, Jacob G, Kaufmann H, Jordan J, Lipsitz LA, Levine BD, Low PA, Mathias C, Raj SR, Robertson D, Sandroni P, Schatz I, Schondorff R, Stewart JM, van Dijk JG (2011) Consensus statement on the definition of orthostatic hypotension, neurally mediated syncope and the postural tachycardia syndrome. Clinical Autonomic Research 21:69–72
Jansen RW, Penterman BJ, van Lier HJ, Hoefnagels WH (1987) Blood pressure reduction after oral glucose loading and its relation to age, blood pressure and insulin. American J Cardiol 60:1087–1091
Baggio LL, Drucker DJ (2004) Clinical endocrinology and metabolism. Glucagon-like peptide-1 and glucagon-like peptide-2. Best Pract Res Clin Endocrinol Metab 18:531–554
Ferris CF, George JK, Eastwood G, Potegal M, Carraway RE (1991) Plasma levels of human neurotensin: methodological and physiological considerations. Peptides 12:215–220
Rudholm T, Wallin B, Theodorsson E, Naslund E, Hellstrom PM (2009) Release of regulatory gut peptides somatostatin, neurotensin and vasoactive intestinal peptide by acid and hyperosmolal solutions in the intestine in conscious rats. Regulatory Peptides 152:8–12
Hornby PJ, Moore BA (2011) The therapeutic potential of targeting the glucagon-like peptide-2 receptor in gastrointestinal disease. Expert Opin Ther Targets 15:637–664
Dube PE, Brubaker PL (2007) Frontiers in glucagon-like peptide-2: multiple actions, multiple mediators. Am J Physiol Endocrinol Metab 293:E460–E465
Golpon HA, Puechner A, Welte T, Wichert PV, Feddersen CO (2001) Vasorelaxant effect of glucagon-like peptide-(7–36)amide and amylin on the pulmonary circulation of the rat. Regulatory Peptides 102:81–86
Yu M, Moreno C, Hoagland KM, Dahly A, Ditter K, Mistry M, Roman RJ (2003) Antihypertensive effect of glucagon-like peptide 1 in Dahl salt-sensitive rats. Journal of Hypertension 21:1125–1135
Barragan JM, Rodriguez RE, Blazquez E (1994) Changes in arterial blood pressure and heart rate induced by glucagon-like peptide-1-(7–36) amide in rats. Am J Physiol Renal Physiol 266:E459–E466
Yamamoto H, Lee CE, Marcus JN, Williams TD, Overton JM, Lopez ME, Hollenberg AN, Baggio L, Saper CB, Drucker DJ, Elmquist JK (2002) Glucagon-like peptide-1 receptor stimulation increases blood pressure and heart rate and activates autonomic regulatory neurons. J Clin Invest 110:43–52
Verges B, Bonnard C, Renard E (2011) Beyond glucose lowering: glucagon-like peptide-1 receptor agonists, body weight and the cardiovascular system. Diabetes Metab J 37:477–488
Claustre J, Brechet S, Plaisancie P, Chayvialle JA, Cuber JC (1999) Stimulatory effect of beta-adrenergic agonists on ileal L cell secretion and modulation by alpha-adrenergic activation. Journal of Endocrinology 162:271–278
Carraway R, Leeman SE (1973) The isolation of a new hypotensive peptide, neurotensin, from bovine hypothalami. J Biol Chem 248:6854–6861
Goedert M, Emson PC (1983) The regional distribution of neurotensin-like immunoreactivity in central and peripheral tissues of the cat. Brain Research 272:291–297
Kalafatakis K, Triantafyllou K (2011) Contribution of neurotensin in the immune and neuroendocrine modulation of normal and abnormal enteric function. Regulatory Peptides 170:7–17
Ferris CF, Hammer RA, Leeman SE (1981) Elevation of plasma neurotensin during lipid perfusion of rat small intestine. Peptides 2(Suppl 2):263–266
Armstrong MJ, Parker MC, Ferris CF, Leeman SE (1986) Neurotensin stimulates [3H]oleic acid translocation across rat small intestine. American Journal of Physiology 251:G823–G829
Robinson BJ, Stowell LI, Purdie GL, Palmer KT, Johnson RH (1992) Autonomic responses to carbohydrate ingestion and head-up tilt in elderly subjects with orthostatic hypotension. Clinical Autonomic Research 2:309–316
Smith GDP, Von Der Thusen J, Mathias CJ (1998) Comparison of the blood pressure response to food ingestion in two clinical subgroups of multiple system atrophy. Parkinsonism Relat Disord 4:113–117
Imai C, Muratani H, Kimura Y, Kanzato N, Takishita S, Fukiyama K (1998) Effects of meal ingestion and active standing on blood pressure in patients > or = 60 years of age. American Journal of Cardiology 81:1310–1314
Task Force of The European Society of Cardiology and The North American Society of Pacing and Electrophysiology (1996) Heart rate variability. Standards of measurement, physiological interpretation, and clinical use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. European Heart Journal 17:354–381
Baba S (1994) International trends in drug treatment. Diabetes: focus on α-glucosidase inhibitors, Churchill Livingstone Japan K.K., Tokyo, pp 20–34
Bischoff H (1995) The mechanism of alpha-glucosidase inhibition in the management of diabetes. Clinical and Investigative Medicine 18:303–311
Gentilcore D, Bryant B, Wishart JM, Morris HA, Horowitz M, Jones KL (2005) Acarbose attenuates the hypotensive response to sucrose and slows gastric emptying in the elderly. American Journal of Medicine 118:1289
Jian ZJ, Zhou BY (2008) Efficacy and safety of acarbose in the treatment of elderly patients with postprandial hypotension. Chin Med J (Engl) 121:2054–2059
Hucking K, Kostic Z, Pox C, Ritzel R, Holst JJ, Schmiegel W, Nauck MA (2005) alpha-Glucosidase inhibition (acarbose) fails to enhance secretion of glucagon-like peptide 1 (7–36 amide) and to delay gastric emptying in Type 2 diabetic patients. Diabetic Medicine 22:470–476
Gentilcore D, Vanis L, Wishart JM, Rayner CK, Horowitz M, Jones KL (2011) The alpha (alpha)-glucosidase inhibitor, acarbose, attenuates the blood pressure and splanchnic blood flow responses to intraduodenal sucrose in older adults. Journals of Gerontology. Series A, Biological Sciences and Medical Sciences 66:917–924
Lee A, Patrick P, Wishart J, Horowitz M, Morley JE (2002) The effects of miglitol on glucagon-like peptide-1 secretion and appetite sensations in obese type 2 diabetics. Diabetes, Obesity & Metabolism 4:329–333
Ranganath L, Norris F, Morgan L, Wright J, Marks V (1998) Delayed gastric emptying occurs following acarbose administration and is a further mechanism for its anti-hyperglycaemic effect. Diabetic Medicine 15:120–124
Sjölund K, Sandén G, Håkanson R, Sundler F (1983) Endocrine cells in human intestine: an immunocytochemical study. Gastroenterology 85:1120–1130
Acknowledgement
We would like to express gratitude to Dr. Yasunori Sato who provided valuable statistical analysis advice.
Conflicts of interest
None.
Ethical standard
This study has been approved by the appropriate ethics committee and has therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fukushima, T., Asahina, M., Fujinuma, Y. et al. Role of intestinal peptides and the autonomic nervous system in postprandial hypotension in patients with multiple system atrophy. J Neurol 260, 475–483 (2013). https://doi.org/10.1007/s00415-012-6660-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-012-6660-x