Abstract
Introduction
0.05 % betamethasone valerate cream is generally used as an alternative to circumcision for the treatment of phimosis in boys. The aim of this study is to determine whether the half-strength formula (0.025 %) of betamethasone is as effective as 0.05 % betamethasone.
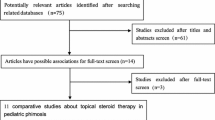
Method
All boys with phimosis seen at our institution between 2010 and 2012, whose parents complained that their children had problems of micturition, i.e., crying and ballooning, and sought for some instructions or treatments, were instructed to apply betamethasone valerate cream. Two strengths, 0.05 and 0.025 %, were randomly applied to each patient twice a day for 2 months. The patients whose parents were not willing to the conservative treatment underwent circumcision.
Results
Of the 47 patients, 23 boys with an average age of 16.65 ± 4.052 months (range 11–24 months) were given 0.025 % betamethasone cream, whereas the remaining 24 boys in control group with an average age of 18.42 ± 5.030 months (range 10–24 months) were instructed to apply with 0.05 % betamethasone valerate cream. Using unpaired t test, the age in both groups were comparable (p = 0.1932). There was a decrease in phimosis grade by the end of the therapeutic course in both groups. Further analysis using Mann–Whitney test revealed that the phimosis grade in the half-strength group (0.025 % strength) was significantly lower to the phimosis grade in the control (0.05 % betamethasone) group (p = 0.0003). There was no diversion from steroid application to circumcision or any side effects in the both groups.
Conclusions
0.025 % betamethasone valerate cream produced a clinical improvement. However, the half-strength formula was not effective as the conventional formula of 0.05 % betamethasone valerate cream.


Similar content being viewed by others
References
Jørgensen ET, Svensson A (1993) The treatment of phimosis in boys, with a potent topical steroid (clobetasol propionate 0.05 %) cream. Acta Derm Venereol 73:55–56
Kikiros CS, Beasley SW, Woodward AA (1993) The response of phimosis to local steroid application. Pediatr Surg Int 8:329–332
Lindhagen T (1996) Topical clobetasol propionate compared with placebo in the treatment of unretractable foreskin. Eur J Surg 162:969–972
Golubovic Z, Milanovic D, Vukadinovic V, Rakic I, Perovic S (1996) The conservative treatment of phimosis in boys. Br J Urol 78:786–788
Lund L, Wai KH, Mui LM, Yeung CK (2000) Effect of topical steroid on non-retractile prepubertal foreskin by a prospective, randomized, double-blind study. Scand J Urol Nephrol 34:267–269
Gairdner D (1949) The fate of the foreskin, a study of circumcision. Br Med J 2:1433–1437
Wright JE (1994) The treatment of childhood phimosis with topical steroid. Aust N Z J Surg 64:327–328
Palmer LS, Palmer JS (2008) The efficacy of topical betamethasone for treating phimosis: a comparison of two treatment regimens. Urology 72:68–71
Monsour MA, Rabinovitch HH, Dean GE (1999) Medical management of phimosis in children: our experience with topical steroids. J Urol 162:1162–1164
Orsola A, Caffaratti J, Garat JM (2000) Conservative treatment of phimosis in children using a topical steroid. Urology 56:307–310
Elmore JM, Baker LA, Snodgrass WT (2002) Topical steroid therapy as an alternative to circumcision for phimosis in boys younger than 3 years. J Urol 168:1746–1747
Marques TC, Sampaio FJ, Favorito LA (2005) Treatment of phimosis with topical steroids and foreskin anatomy. Int Braz J Urol 31:370–374
Zampieri N, Corroppolo M, Camoglio FS, Giacomello L, Ottolenghi A (2005) Phimosis: stretching methods with or without application of topical steroids? J Pediatr 147:705–706
Berdeu D, Sauze L, Ha-Vinh P, Blum-Boisgard C (2001) Cost-effectiveness analysis of treatments for phimosis: a comparison of surgical and medicinal approaches and their economic effect. BJU Int 87:239–244
Van Howe RS (1998) Cost-effective treatment of phimosis. Pediatrics 102:E43
Yilmaz E, Batislam E, Basar MM, Basar H (2003) Psychological trauma of circumcision in the phallic period could be avoided by using topical steroids. Int J Urol 10:651–656
Hutcheson JC (2004) Male neonatal circumcision: indications, controversies and complications. Urol Clin North Am 31:461–467 (viii)
Hammarström S, Hamberg M, Duell EA, Stawiski MA, Anderson TF, Voorhees JJ (1977) Glucocorticoid in inflammatory proliferative skin disease reduces arachidonic and hydroxyeicosatetraenoic acids. Science 197:994–996
Gavan N, Maibach H (1997) Effect of topical corticosteroids on the activity of superoxide dismutase in human skin in vitro. Skin Pharmacol 10:309–313
Nuutinen P, Riekki R, Parikka M, Salo T, Autio P, Risteli J, Oikarinen A (2003) Modulation of collagen synthesis and mRNA by continuous and intermittent use of topical hydrocortisone in human skin. Br J Dermatol 148:39–45
Haapasaari KM, Risteli J, Karvonen J, Oikarinen A (1997) Effect of hydrocortisone, methylprednisolone aceponate and momethasone furoate on collagen synthesis in human skin in vivo. Skin Pharmacol 10:261–264
Korting HC, Unholzer A, Schäfer-Korting M, Tausch I, Gassmueller J, Nietsch KH (2002) Different skin thinning potential of equipotent medium-strength glucocorticoids. Skin Pharmacol Appl Skin Physiol 15:85–91
Delforno C, Holt PJ, Marks R (1978) Corticosteroid effect on epidermal cell size. Br J Dermatol 98:619–623
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sookpotarom, P., Asawutmangkul, C., Srinithiwat, B. et al. Is half strength of 0.05 % betamethasone valerate cream still effective in the treatment of phimosis in young children?. Pediatr Surg Int 29, 393–396 (2013). https://doi.org/10.1007/s00383-012-3253-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-012-3253-9