Abstract
Objective
The aim was to assess the long-term effect of trimetazidine on myocardial perfusion, using gated single photon emission computerized tomography (SPECT).
Methods
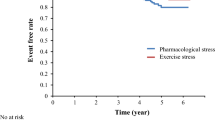
200 patients (aged 54.7 ² 12 years) with ischemic left ventricular dysfunction (LVD) and multivessel coronary artery disease were randomized to receive trimetazidine 20mg three times daily or a placebo for 24 months. At baseline and after 24 months of treatment, all patients underwent a symptom-limited cardiopulmonary exercise test concluded by the injection of 99mTc-MIBI (technetium-99m methoxy-isobutyl-isonitrile). Imaging of post-stress gated SPECT and resting gated SPECT were performed. Standard antianginal therapy was interrupted for 48 hours (nitrates for 6 hours) before the exercise tests and resumed immediately after testing.
Results
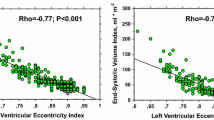
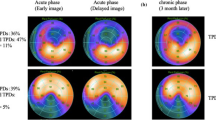
On initial evaluation, summed stress and rest scores (SSS and SRS, respectively), systolic wall thickness (SWT), and wall motion score index (WMI), heart rate, SBP, and rate pressure product were similar at rest and peak exercise in both groups. After 24 months, 91 % of patients in the trimetazidine group versus 22% in the placebo group showed a significant decrease of the frequency of anginal episodes per week (3.9 vs 5.7, p < 0.01). Weekly nitroglycerin (glyceryl trinitrate) tablet consumption was significantly lower with trimetazidine than with placebo at endpoint (2.3 ² 0.8 vs 6.1 ² 1.6, p < 0.01). This was supported by perfusion SPECT data. Compared with baseline values, SSS and SRS were significantly reduced with trimetazidine (from 19.8 ² 7.7 to 11.2 ² 6.1, p < 0.00001 and from 12.4 ² 8.7 to 5.8 ² 3.3, p < 0.00001, respectively). There was a nonsignificant decrease from baseline values in both SRS and SSS with placebo group (from 11.9 ² 8.3 to 11.2 ² 7.4 and 18.1²6.3 to 17.9 ² 9.2, respectively).
Duration of peak exercise increased significantly from baseline values with trimetazidine (from 4.6 to 5.8 minutes, p < 0.01) but not with placebo (from 5.4 to 5.8 minutes). Accordingly, mean maximum work at peak exercise improved by 1.2 metabolic equivalents with trimetazidine. This was proved by gated SPECT with an increase in SWT score of 89.5% (p < 0.00001) and in ejection fraction of 23% with trimetazidine (p < 0.001) without significant changes in hemodynamic parameters.
Conclusion
Trimetazidine improves ischemic attacks in patients with ischemic cardiomyopathy, clinically and objectively as seen in gated SPECT myocardial perfusion. The improvement in myocardial function with trimetazidine was not accompanied by hemodynamic changes.








Similar content being viewed by others
References
Birnbaum Y, Criger DA, Wagner GS, et al. Prediction of the extent and severity of left ventricular dysfunction in anterior acute myocardial infarction by the admission electrocardiogram. Am Heart J 2001; 141(6): 915–24.
Pfeffer MA, McMurray JJ, Velazquez EJ, et al. Valsartan, captopril, or both in myocardial infarction complicated by heart failure, left ventricular dysfunction, or both. N Engl J Med 2003; 349(20): 1893–906.
DiBianco R. Update on therapy for heart failure. Am J Med 2003; 115(6): 480–8.
McKee SP, Leslie SJ, LeMaitre JP, et al. Management of chronic heart failure due to systolic left ventricular dysfunction by cardiologist and non-cardiologist physicians. Eur J Heart Fail 2003; 5(4): 549–55.
McClellan KJ, Plosker GL. Trimetazidine: a review of its use in stable angina pectoris and other coronary conditions. Drugs 1999; 58: 143–57.
Marzilli M, Klein W. Efficacy and tolerability of trimetazidine in stable angina: a metaanalysis of randomized, double-blind, controlled trials. Coron Artery Dis 2003; 14: 171–9.
Cross HR. Trimetazidine for stable angina pectoris. Expert Opin Pharmacother 2001; 2(5): 857–75.
Lu C, Dabrowski P, Fragasso G, et al. Effects of trimetazidine on ischemic left ventricular dysfunction in patients with coronary artery disease. Am J Cardiol 1998; 82(7): 898–901.
Marzilli M. Cardioprotective effects of trimetazidine: a review. Curr Med Res Opin 2003; 19(7): 661–72.
Desideri A, Celegon L. Metabolic management of ischemic heart disease: clinical data with trimetazidine. Am J Cardiol 1998; 82(5A): 50K–3K.
Kantor P, Lucien A, Kozak R, et al. The antianginal drug trimetazidine shifts cardiac energy metabolism from fatty acid oxidation to glucose oxidation by inhibiting mitochondrial long-chain 3-ketoacyl coenzyme A thiolase. Circ Res 2000; 86(5): 580–8.
Sellier P, Broustet J-P. Assessment of anti-ischemic and antianginal effect at trough plasma concentration and safety of trimetazidine MR 35mg in patients with stable angina pectoris: a multicenter, double-blind, placebo-controlled study. Am J Cardiovasc Drugs 2003; 3(5): 361–9.
Shlyakhto EV, Almazov VVA, Nifontov EM, et al. Antianginal effects of trimetazidine and left ventricular function improvement in patients with stable angina pectoris. Am J Cardiovasc Drugs 2002; 2(2): 119–24.
Kober G, Pennaforte S, Buck T, et al. Myocardial cytoprotection during percutaneous transluminal coronary angioplasty. Eur Heart J 1993; 14 Suppl. G: 6–11.
Birand A, Kudaiberdieva GZ, Batyraliev TA, et al. Effects of trimetazidine on heart rate variability and left ventricular systolic performance in patients with coronary artery disease after percutaneous transluminal angioplasty. Angiology 1997; 48(5): 413–22.
Polonski L, Dec I, Wojnar R, et al. Trimetazidine limits the effects of myocardial ischaemia during percutaneous coronary angioplasty. Curr Med Res Opin 2002; 18(7): 389–96.
Detry JM, Sellier P, Pennaforte S, et al. Trimetazidine: a new concept in the treatment of angina. Comparison with propranolol in patients with stable angina: Trimetazidine European Multicenter Study Group. Br J Clin Pharmacol 1994; 37(3): 279–88.
Szwed H, Sadowski Z, Elikowski W, et al. Trimpol II: combination treatment of stable effort angina using trimetazidine and metoprolol. Results of a randomised, double blind, multicentre study. Eur Heart J 2001; 22(2): 2267–74.
Dalla-Volta S, Maraglino G, Delia-Valentina P, et al. Comparison of trimetazidine with nifedipene in effort angina: a double-blind, crossover study. Cardiovasc Drugs Ther 1990; 4: 853–9.
Levy S. Combination therapy of trimetazidine with diltiazem in patients with coronary artery disease: Group of South of France Investigators. Am J Cardiol 1995; 76: 12B–6B.
Manchanda SC, Krishnaswani S. Combination treatment with trimetazidine and diltiazem in stable angina pectoris. Heart 1997; 78: 353–7.
Dahlberg ST, Leppo JA. Myocardial kinetics of radiolabeled perfusion agents: basis for perfusion imaging. J Nucl Cardiol 1994; 1(2 Pt 1): 189–97.
Germano G, Erel J, Lewin H, et al. Automatic quantitation of regional myocardial wall motion and thickening from gated technetium-99m sestamibi myocardial perfusion single-photon emission computed tomography. J Am Coll Cardiol 1997; 30(5): 1360–7.
Germano G, Kiat H, Kavanagh PB, et al. Automatic quantification of ejection fraction from gated myocardial perfusion SPECT. J Nucl Med 1995; 36(11): 2138–47.
Belardinelli R. Trimetazidine and the contractile response of dysfunctional myocardium in ischaemic cardiomyopathy. Rev Port Cardiol 2000; 19 Suppl. 5: V35–9.
Belardinelli R, Purcaro A. Effects of trimetazidine on the contractile response of chronically dysfunctional myocardium to low-dose dobutamine in ischaemic cardiomyopathy. Eur Heart J 2001; 22(23): 2164–70.
Ciavolella M, Greco C, Tavolaro R, et al. Acute oral trimetazidine administration increases resting technetium 99m sestamibi uptake in hibernating myocardium. J Nucl Cardiol 1998; 5(2): 128–33.
Acknowledgments
The authors acknowledge the assistance of Servier Medical, Egypt and the Nuclear Cardiology staff at the National Heart Institute, Cairo University, Egypt.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
El-Kady, T., El-Sabban, K., Gabaly, M. et al. Effects of Trimetazidine on Myocardial Perfusion and the Contractile Response of Chronically Dysfunctional Myocardium in Ischemic Cardiomyopathy. Am J Cardiovasc Drugs 5, 271–278 (2005). https://doi.org/10.2165/00129784-200505040-00006
Published:
Issue Date:
DOI: https://doi.org/10.2165/00129784-200505040-00006