Abstract
Synopsis
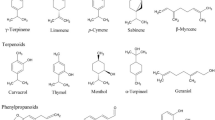
Serenoa repens (Permixon®)1 has been available for several years for the treatment of men with benign prostatic hyperplasia (BPH). The drug is the n-hexane lipidosterolic extract of the dwarf American palm (also known as Serenoa repens ) and is a complex mixture of various compounds. A number of pharmacodynamic effects have been demonstrated with the lipidosterolic extract of Serenoa repens (LSESR), suggesting multiple mechanisms of action including in vitro inhibition of both type 1 and type 2 isoenzymes of 5α-reductase and interference with binding of dihydrotestosterone to cytosolic androgen receptors in prostate cells.
In controlled clinical trials in men with BPH, oral administration of Serenoa repens 160mg twice daily for 1 to 3 months was generally superior to placebo in improving subjective symptoms, such as dysuria, as well as objective parameters. The frequency of nocturia was reduced by 33 to 74%, while urinary frequency during the day decreased by 11 to 43% and peak urinary flow rate increased by 26 to 50% with Serenoa repens. Corresponding values for placebo were 13 to 39%, 1 to 29% and 2 to 35%. The only large comparative trial conducted to date, in which >1000 men with moderate BPH were randomised to receive Serenoa repens 160mg twice daily or finasteride 5mg once daily for 6 months, demonstrated similar efficacy between the two drugs. No statistically significant difference was demonstrated between treatment groups for improvement in patient self-rated quality-of-life scores and the primary end-point of objective symptom score; International Prostate Symptom Score improved by 37% with Serenoa repens compared with 39% with finasteride. In much smaller comparative trials, few significant differences were demonstrated between Serenoa repens and α1-receptor antagonists, and larger randomised trials of adequate duration are required to better compare the clinical efficacy of these drugs. The most frequently reported adverse events in clinical trials with Serenoa repens have been minor gastrointestinal problems (e.g. nausea and abdominal pain).
In conclusion, Serenoa repens is well tolerated and has greater efficacy than placebo and similar efficacy to finasteride in improving symptoms in men with BPH. Although there is a need for further comparative studies, particularly with α1-receptor antagonists, available data indicate that Serenoa repens is a useful alternative to α1-receptor antagonists and finasteride in the treatment of men with BPH.
Pharmacodynamic Properties
The precise mechanism of action of Serenoa repens has not been fully elucidated; however, important in vitro effects of the lipidosterolic extract of Serenoa repens (LSESR) include inhibition of 5α-reductase, the enzyme responsible for conversion of testosterone to dihydrotestosterone (DHT), and inhibition of binding of DHT to androgen receptors in the cytosolic component of prostate cells. Two 5α-reductase isoenzymes, type 1 and 2, appear to be expressed by cultured human prostate cells. Although there is some controversy whether the type 1 isoenzyme is expressed, it is generally agreed that the type 2 isoenzyme predominates. LSESR has been shown to inhibit both isoenzymes in a eukaryotic expression system, whereas finasteride primarily inhibits 5α-reductase type 2. LSESR also inhibited binding of the ligand [ H]methyltrienolone to androgen receptors in the cytosolic component of rat prostate cells and inhibited binding of [ H]DHT to its receptor in human foreskin fibroblasts.
Data from other in vitro studies and in vivo trials conducted in various animal models suggest additional mechanisms by which the drug may exert its effects. These include inhibition of prolactin- and growth factor-induced prostatic cell proliferation, an antioedematous effect and interference with mediators of inflammation.
Studies in men with benign prostatic hyperplasia (BPH) receiving Serenoa repens 320 mg/day for 3 months also suggest an antiestrogenic effect of the drug, and a comparative trial demonstrated reductions in prostatic tissue levels of DHT similar to those observed with finasteride 5 mg/day.
Pharmacokinetic Properties
Limited pharmacokinetic data are available for Serenoa repens, primarily because the drug is a complex mixture of several compounds. In healthy young men, mean peak plasma drug concentration (second component; retention time 26.4 minutes on high performance liquid chromatography assay) was 2.6 mg/L and time to achieve peak concentration was 1.5 hours after oral administration of Serenoa repens 320mg. Elimination half-life was 1.9 hours and mean value of area under the concentration versus time curve was 8.2 mg/L • h. Tissue distribution studies in the rat indicate that the drug achieved higher concentrations in the prostate gland than the liver or genitourinary tissues other than the prostate.
Therapeutic Efficacy
The effects of Serenoa repens 160mg twice daily on urinary frequency and peak urinary flow rate were superior to placebo in 3 of 4 larger (i.e. >50 patients) controlled clinical trials lasting 1 to 3 months in men with BPH. Serenoa repens was associated with reductions in urinary frequency at night ranging from 33 to 74% (13 to 39% with placebo) and urinary frequency during the day ranging from 11 to 43% (1 to 29% with placebo); peak urinary flow rate was increased by 26 to 50% (2 to 35% with placebo) in placebo-controlled trials. Some studies evaluated additional parameters and demonstrated that Serenoa repens was more effective than placebo in improving dysuria (difficult or painful urination), reducing postmicturition residual urinary volume and improving subjective symptoms of BPH according to patient and physician global assessment.
Clinical efficacy of Serenoa repens 160mg twice daily was compared with that of finasteride 5mg once daily for 6 months in a large randomised double-blind study. The study was conducted in 9 European countries and is the largest international trial comparing 2 drugs in the treatment of men with BPH. Intention-to-treat analysis included 1069 men with moderate BPH and demonstrated similar results between treatment groups. At the end of the treatment period, symptoms [as assessed using the well-accepted International Prostate Symptom Score (I-PSS)] were reduced by 37% among Serenoa repens recipients compared with 39% among finasteride recipients, and the difference between treatment groups was not statistically significant. A marked improvement in patient self-rated quality-of-life scores was noted with both Serenoa repens and finasteride (69 vs 73%; no statistically significant difference between groups). Results of a separate questionnaire demonstrated that Serenoa repens produced a modest improvement in sexual function score, whereas a deterioration was reported with finasteride, and the difference between treatment groups achieved statistical significance. Both drugs improved peak urinary flow rates and reduced prostate volume, although changes were significantly greater with finasteride. However, the proportion of patients with a 30% or 3 ml/sec increase in peak urinary flow rate was similar between treatment groups. Unlike finasteride, Serenoa repens did not significantly affect serum prostate specific antigen (PSA) levels.
In two smaller comparative trials, Serenoa repens 160mg twice daily and α1-receptor antagonists improved overall symptoms, reduced urinary frequency and postmicturition residual urine volume and increased urinary flow rate. In general, clinical efficacy tended to favour the α1-receptor antagonists (alfuzosin 2.5mg 3 times daily and prazosin titrated to 2mg every 12 hours); however, few significant differences were observed between treatment groups. Moreover, studies included relatively small numbers of patients and one of the trials was only 3 weeks in duration.
Tolerability
In general, Serenoa repens is well tolerated, with only 2% of patients spontaneously reporting adverse events in a large noncomparative trial of 500 men with BPH receiving the drug for 3 months. Similar results were noted in smaller placebo-controlled trials, and discontinuation of Serenoa repens because of poor tolerability occurred only rarely. The most common adverse events in clinical trials have been minor gastrointestinal complaints, such as nausea and abdominal pain. In a large comparative trial with finasteride, Serenoa repens tended to be associated with a higher incidence of hypertension, headache, urinary retention and back pain, whereas gastrointestinal complaints, impotence, dysuria and decreased libido tended to be more frequently reported among men receiving finasteride. Clinically significant changes in laboratory parameters did not occur with Serenoa repens in clinical trials.
Dosage and Administration
For the treatment of men with BPH the recommended dosage of Serenoa repens is 160mg twice daily by oral administration. The drug should be taken with morning and evening meals to minimise possible gastrointestinal disturbances.
Similar content being viewed by others
References
Benard P, Cousse H, Chevalier G. Distribution study of radioactivity in rats after oral administration of lipidosterolic extract of Serenoa repens (Permixon®) supplemented with [1-14C] lauric acid, [1-14C] oleic acid or [4-14C] beta-sitosterol. Eur J Drug Metab Pharmacokinet. In press
Fitzpatrick JM, Lynch TH. Phytotherapeutic agents in the management of symptomatic benign prostatic hyperplasia. Urol Clin North Am 1995; 22(2): 407–12
Neuzil E, Cousse H. The Saw palmetto Serenoa repens: botanical and chemical aspects. Bull Soc Pharm Bordeaux 1993; 132: 121–41
Raynaud J-P. Permixonα1® an overview of its pharmacological activities as regards medical treatment of benign prostatic hypertrophy (BPH). In: Dimopoulos CA, Di Silverio F, editors. BPH: From molecular biology to patient relief. Proceedings of the satellite symposium held during the 4th Mediterranean Congress of Urology; 1995 Sep 6-10; Rhodes. Bologna: Monduzzi Editore, 1996: 57-69
Isaacs JT, Brendler CB, Walsh PC. Changes in the metabolism of dihydrotestosterone in the hyperplastic human prostate. J Clin Endocrinol Metab 1983; 56: 139–46
Imperato-McGinley G, Gautier T, Zirinsky K, et al. Prostate visualisation studies in male homozygous and heterozygous for 5α-reductase deficiency. J Clin Endocrinol Metab 1992; 75: 1022–6
Bruchovsky N. Comparison of the metabolites found in rat prostate following the in vivo administration of 7 natural andro-gens. Endocrinology 1971; 89: 1212–8
Sitteree PK, Wilson JD. Dihydrotestosterone of prostatic hypertrophy. I. The formation and content of dihydrotestosterone in the hypertrophic state of man. J Clin Invest 1970; 49: 1737–45
Walsh PC, Hutchins GM, Ewing LL. Tissue content of dihydrotestosterone in human prostatic hyperplasia is not supranormal. J Clin Invest 1983; 72: 1772–7
Délos S, Iehlé C, Martin PM, et al. Inhibition of the activity of ‘basic’ 5 α-reductase (type 1) detected in DU 145 cells and expressed in insect cells. J Steroid Biochem Mol Biol 1994 Mar; 48: 347–52
Iehlé C, Délos S, Guirou O, et al. Human prostatic steroid 5α-reductase isoforms — a comparative study of selective inhibitors. J Steroid Biochem Mol Biol 1995; 54: 273–9
Strauch G, Perles P, Vergult G, et al. Comparison of finasteride (Proscar®) and Serenoa repens (Permixon®) in the inhibition of 5-alpha reductase in healthy male volunteers. Eur Urol 1994; 26: 247–52
Briley M, Carilla E, Roger A, et al. A new treatment of prostatic hyperplasia, Permixon® has antiandrogen effects at two complementary levels. New Trends Androlog Sci 1985; 1(1): 24–6
Carilla E, Briley M, Fauran F, et al. Binding of Permixon, a new treatment for prostatic benign hyperplasia, to the cytosolic androgen receptor in the rat prostate. J Steroid Biochem 1984 Jan; 20: 521–3
Carilla E, Roger A, Briley M, et al. The lipido-sterolic extract of Serenoa repens B: new treatment of prostatic hyperplasia, with anti-androgen effects at two complementary levels. Excerpta Medica 1986: 216-23
Sultan C, Terraza A, Devillier C, et al. Inhibition of androgen metabolism and binding by a liposterolic extract of “Serenoa Repens B” in human foreskin fibroblasts. J Steroid Biochem 1984; 20(1): 515–9
Sultan C, Terraza A, Carilla E, et al. Anti-androgenic effects of Permixon: in vitro studies. New trends in BPH etiopathogen-esis. Proceedings of the International Workshop in Urology; 1987 Jul 22-25; Cannes, Rome; Acta Medica, 1988: 239-246.
Farnsworth WE. PermixonR: antagonist of prolactin (PRL) action on the prostate [abstract no. 749]. 73rd Annual Meeting of the Endocrine Society, Washington, USA.
Vacher P, Prevarskaya N, Skryma R, et al. The lipidosterolic extract from Serenoa repens interferes with prolactin receptor signal transduction. J Biomed Sci 1995; 2: 357–65
Paubert-Braquet M, Cousse H, Raynaud JP, et al. Effect of the lipidic Serenoa repens extract (PermixonR) on the ionophore A23187-stimulated production of leukotriene B4 (LTB4) from human polymorphonuclear neutrophils. Prostaglandins Leukotrienes and Medicine. In press
Ragab A, Ragab-Thomas JMF, Delhon A, et al. Effects of Per-mixonR (Sereprostat® in Spain) on phospholipase A2 activity and on arachidonic acid metabolism in cultured prostatic cells. New trends in BPH etiopathogenesis 1987: 293-6
Crastes de Paulet A, Damon M, Le Doucen C, et al. Anti-inflammatory and antiagregant activities of a lipido-sterolic extract from Serenoa repens on human neutrophiles and on human platelets models. Pierre Fabre Médicaments. (Data on file)
Paubert Braquet M, Janssen DH, Servent N, et al. Permixon® [lipido sterolic extract of Serenoa repens (LSESr)] inhibits b-FGF- and EGF-induced proliferation of human prostate or-ganotypic cell lines [abstract]. Pharmacol Res 1995; 31 Suppl.: 69
Di Silverio F, Sciarr A, D’Eramo G, et al. Response of tissue androgen and epidermal growth factor concentrations to the long-term administration of Serenoa repens (PermixonR), finasteride and flutamide to BPH patients. Eur Urol 1996; 30 Suppl. 2: 96
Tarayre JP, Delhon A, Lauressergues H, et al. Anti-edematous action of a hexane extract of the stone fruit of Serenoa repens Bartr [in French]. Ann Pharm Fr 1983; 41: 559–70
Di Silverio F, D’Eramo G, Lubrano C, et al. Evidence that Serenoa repens extract displays an antiestrogenic activity in prostatic tissue of benign prostatic hypertrophy. Eur Urol 1992; 21: 309–14
Rhodes L, Primka RL, Berman C, et al. Comparison of finasteride (Proscar®), a 5-α reductase inhibitor, and various commercial plant extracts in in vitro and in vivo 5-α reductase inhibition. Prostate 1993; 22(1): 43–51
Andersson S, Russell DW. Structural and biochemical properties of cloned and expressed human and rat steroid 5α-reduc-tases. Proc Natl Acad Sci USA 1990; 87: 3640–4
Jenkins EP, Andersson S, Imperato-McGinley G, et al. Genetic and pharmacological evidence for more than one human steroid 5α-reductase. J Clin Invest 1992; 89: 293–300
Andersson S, Berman DM, Jenkins EP, et al. Deletion of steroid 5α-reductase 2 gene in male pseudohermaphroditism. Nature 1991; 354: 159–61
Bonnet P, Reiter E, Bruyninx M, et al. Benign prostatic hyperplasia in normal prostate aging: differences in types I and II 5 alpha reductase and steroid hormone receptor messenger ribonucleic acid (mRNA) levels but not in insulin like growth factor mRNA levels. J Clin Endocrinol Metab 1993; 77: 1203–8
Hirsch KS, Jones CD, Audia JE, et al. LY191704: a selective, nonsteroidal inhibitor of human steroid 5α-reductase type 1. Proc Natl Acad Sci USA 1993; 90: 5277–81
Iehlé C, Raynaud J-P, Martin P-M, et al. Steroid 5α-reductase type 1 is expressed in the human pathological prostate [abstract]. J Urol 1996 May; 155(5) Suppl.: 808
Rennie PS, Bruchovsky N, McLaughlan MG, et al. Kinetic analysis of 5α-reductase isoenzymes in benign prostatic hyperplasia (BPH). J Steroid Biochem 1983; 19: 169–73
Ross M, Chapman K, Habib FK. The expression of type 1 and type 2 5-alpha reductase mRNA in BPH and prostate cancer and in short term primary cultures of prostate epithelial and stromal cells [abstract]. British Prostate Group: Future Perspectives in Prostatic Disease; 1996; 19-20 Mar; The University of York, UK, p 22.
Levine AC, Wang J-P, Ren M, et al. Immunohistochemical localization of steroid 5α-reductase 2 in the human male fetal reproductive tract and adult prostate. J Clin Endocrinol Metab 1996; 81(1): 384–9
Habib F, Grant E. BPH and current biochemical trends. In press
Silver I, Wiley EL, Davis DL, et al. Expression and regulation of steroid 5α-reductase 2 in prostate disease. J Urol 1994; 152: 433–7
Silver I, Wiley EL, Thigpen AE, et al. Cell type specific expression of 5α-reductase 2. J Urol 1994; 152: 438–42
Thigpen AE, Silver RI, Guileyardo JM, et al. Tissue distribution and ontogeny of steroid 5α-reductase isozyme expression. J Clin Invest 1993; 92: 903–10
Tsai SY, Tsai M-J, O’Malley BW. The steroid receptor super-family: transactivators of gene expression. In: Parker MG, editor. Nuclear hormone receptors. London: Academic Press, 1991: 103–24
Ravenna L, Di Silverio F, Russo M, et al. Effects of the lipido-sterolic extract of Serenoa repens (Permixon®) on human pro-static cell lines. Prostate. In press
Robinette CL. Sex-hormone-induced inflammation and fibro-muscular proliferation in the rat lateral prostate. Prostate 1988; 12: 271–86
Theyer G, Kramer G, Assmann I, et al. Phenotypic characterization of infiltrating leukocytes in benign prostatic hyper-plasia. Lab Invest 1992; 66: 96–107
Paubert-Braquet M, Richardson FO, Servent-Saez N, et al. Effect of Serenoa repens extract (Permixon®) on estradiol/tes-tosterone-induced experimental prostate enlargement in the rat. Pharmacol Res. In press
Stenger A, Tarayre J-P, Carilla E, et al. Pharmacologic and biochemical study of the hexane extract of Serenoa repens B (PA 109). La Gazette Médicale de France 1982; 89(17): 2041–8
De Bernardi di Valserra M, Tripodi AS, Contos S, et al. Serenoa repens capsules: a bioequivalence study. Acta Toxicol Ther 1994; 15(1): 21–39
Oesterling JE. Benign prostatic hyperplasia. Medical and minimally invasive treatment options. N Engl J Med 1995; 332(2): 99–109
Geller J, Kirschenbaum A, Lepor H, et al. Therapeutic controversies: clinical treatment of benign prostatic hyperplasia. J Clin Endocrinol Metab 1995; 80(3): 745–8
Andersen JT. α1-Blockers vs 5α-reductase inhibitors in benign prostatic hyperplasia: a comparative review. Drugs Aging 1995; 6(5): 388–96
Berry SJ, Coffey DS, Walsh PC, et al. The development of human benign prostatic hyperplasia with age. J Urol 1984; 132: 474–9
Clinton JJ. Benign prostatic hyperplasia (BPH) — diagnosis and treatment. JAMA 1994 Apr 20; 271: 1151
Lepor H, Nitti VW. Treatment of benign prostatic hyperplasia. Reply [letter]. Lancet 1996 May 4; 347: 1270
Authie D, Cauquil J. A multicenter study of the efficacy of Permixon in daily practice [in French]. C R Ther Pharmacol Clin 1987; 5(56): 3–13
Ebbinghaus KD. Efficacy of Permixon® in the treatment of benign prostatic hyperplasia [in German]. Journal Für Urologie und Urogynäkologie 1995; 2: 17–21
Barreto HP, de Vivero C, Castro LEC, et al. Advances in the medical management of benign prostatic hyperplasia [in Spanish]. Tribuna Medica 1995; 91(4): 197–205
Hanus M, Matouskova M. Alternative treatment of benign prostatic hypertrophy by Permixon (Capistan) [in Czech]. Rozhl Chir 1993 Feb; 72: 75–9
Mancuso G, Guillot F, Migaleddu V, et al. Serenoa repens in treatment of benign prostate hypertrophy [in Italian]. Urologia 1986; 53(5): 709–14
Martorana G, Giberti C, Pizzorno R, et al. Treatment of prostate adenoma with Serenoa repens extract [in Italian]. Urologia 1986; 53(3): 366–9
Olle-Carreras J. Our experience with a hexane extract of Serenoa repens in the treatment of benign prostatic hypertrophy [in Spanish]. Arch Esp Urol 1987 Jun; 40: 310–3
Orfei S, Grumelli B, Galetti G. Clinical and flowmetric study of Permixon in aged patients [in Italian]. Urologia 1988; 55(4): 373–81
Paoletti PP, Francalanci R, Tenti S, et al. Medical treatment of prostate hypertrophy: trial with the therapeutic use of Serenoa repens [Italian]. Urologia 1986; 53(2): 182–7
Pescatore D, Calvi P, Michelotti P. Urodynamic evaluation of management of prostatic adenoma with Serenoa repens extract [in Italian]. Urologia 1986; 53(6): 894–7
Pisani E. National experience on therapeutic use of Serenoa repens. New Trends Androlog Sci 1985; 1(1): 110–2
Tenaglia R, DśEramo G, Bertolozzi L, et al. Mechanism of action of Serenoa repens: considerations and conclusions. New Trends Androlog Sci 1985; 1(1): 132–4
Vespasiani G, Cesaroni M, Parziani S, et al. Treatment of benign prostatic hypertrophy with Serenoa repens [in Italian]. Urologia 1987; 54(2): 145–9
Dathe G, Schmid H. Phytotherapy of benign prostate hyperplasia with Serenoa repens extract (Permixon registered ) [in German]. Urologe Ausg B 1991; 31(5): 220–3
Boccafoschi C, Annoscia S. Comparison of Serenoa repens extract and placebo in controlled clinical trial in patients with prostatic adenomatosis [in Italian]. Urologia 1983; 50(6): 1–14
Champault G, Patel JC, Bonnard AM. A double-blind trial of an extract of the plant Serenoa repens in benign prostatic hyperplasia. Br J Clin Pharmacol 1984 Sep; 18: 461–2
Cukier, Ducassou, Le Guillou, et al. Serenoa repens extract vs. placebo. C R Ther Pharmacol Clin 1985; 4(25): 15–21
Descotes JL, Rambeaud JJ, Deschaseaux P, et al. Placebo-controlled evaluation of the efficacy and tolerability of Permixon® in benign prostatic hyperplasia after exclusion of placebo responders. Clin Drug Invest 1995 May; 9: 291–7
Emili E, Lo Cigno M, Petrone U. Clinical results on a new drug in the treatment of benign prostatic hyperplasia (Permixon) [in Italian]. Urologia 1983; 50(5): 1042–9
Reece Smith H, Memon A, Smart CJ, et al. The value of Permixon in benign prostatic hypertrophy. Br J Urol 1986 Feb; 58: 36–40
Tasca A, Barulli M, Cavazzana A, et al. Treatment of obstruction in prostatic adenoma using an extract of Serenoa repens. Double-blind clinical test v. placebo [in Italian]. Minerva Urol Nefrol 1985; 37(1): 87–91
Carraro J-C, Raynaud J-P, Koch G, et al. Comparison of phytotherapy (Permixon®) with finasteride in the treatment of benign prostate hyperplasia: a randomized international study of 1098 patients. Prostate. In press
Grasso M, Montesano A, Buonaguidi A, et al. Comparative effects of alfuzosin versus Serenoa repens in the treatment of symptomatic benign prostatic hyperplasia. Arch Esp Urol 1995 Jan-Feb; 48: 97–103
Adriazola Semino M, Lozano Ortega JL, Garcia Cobo E, et al. Symptomatic treatment of benign hypertrophy of the prostate. Comparative study of prazosin and Serenoa repens [in Spanish], Arch Esp Urol 1992 Apr; 45: 211–3
Mandressi S, Tarallo U, Maggioni A, et al. Medical treatment of benign prostatic hyperplasia: efficacy of the extract of Serenoa repens (Permixon®) compared to that of the extract of Pygeum africanum and a placebo [in Italian]. Urologia 1983; 50(4): 752–8
Pannunzio E, D’Ascenzo R, Giardinetti F, et al. Serenoa repens vs. gestonorone caproate in treatment of benign prostatic hypertrophy [in Italian]. Urologia 1986; 53(5): 696–705
Peters DH, Sorkin EM. Finasteride: a review of its potential in the treatment of benign prostatic hyperplasia. Drugs 1993; 46(1): 177–208
Anon. Benign prostatic hyperplasia: diagnosis and treatment: guideline overview. J Natl Med Assoc 1994 Jul; 86: 489-549
McCarthy M. BPH guidelines. Lancet 1994 Feb 19; 343: 473
Eri LM, Tveter KJ. α-Blockade in the treatment of symptomatic benign prostatic hyperplasia. J Urol 1995; 154: 923–34
Madsen FA, Bruskewitz RC. Benign prostatic hyperplasia: pathophysiology and pharmacological treatment. Curr Opin Nephrol Hypertension 1995; 4: 455–9
Lepor H, Williford WO, Barry MJ, et al. The efficacy of ter-azosin, finasteride, or both in benign prostatic hyperplasia. N Engl J Med 1996; 335(8): 533–9
Walsh PC. Treatment of benign prostatic hyperplasia [editorial]. N Engl J Med 1996; 335(8): 586–7
Author information
Authors and Affiliations
Additional information
Various sections of the manuscript reviewed by: A.C. Buck, Department of Urology, Glasgow Royal Infirmary, Glasgow, Scotland; M. Grasso, Department of Urology, Scientific Institute H San Raffaele, Milan, Italy; F.K. Habib, Department of Surgery, University of Edinburgh, Western General Hospital, Edinburgh, Scotland; A.C. Levine, Division of Endocrinology and Metabolism, Department of Medicine, Mount Sinai Medical Center, New York, New York, USA; A.D. Mooradian, Department of Endocrinology and Metabolism, St. Louis University Health Sciences Center, St. Louis, Missouri, USA; G.P. Murphy, Pacific Northwest Cancer Foundation, Seattle, Washington, USA; P. Vacher, Laboratoire de Neurophysiologie, Université de Bordeaux, Bordeaux, France.
Rights and permissions
About this article
Cite this article
Plosker, G.L., Brogden, R.N. Serenoa repens (Permixon®). Drugs & Aging 9, 379–395 (1996). https://doi.org/10.2165/00002512-199609050-00008
Published:
Issue Date:
DOI: https://doi.org/10.2165/00002512-199609050-00008