Abstract
Proton pump inhibitors (PPIs) are widely prescribed for the treatment of gastric acid-related disorders and the eradication of Helicobacter pylori. In addition, they are routinely prescribed for the prevention of gastrointestinal bleeding in patients receiving a dual antiplatelet therapy consisting of clopidogrel and aspirin (acetylsalicylic acid) after myocardial infarction or percutaneous coronary intervention and stenting. Because PPIs are given to these patients for long periods, there is a concern about the potential for clinically significant drug-drug interactions (DDIs) with concomitantly administered medications. Because PPIs give rise to profound and long-lasting elevation of intragastric pH, it is not surprising that they interfere with the absorption of concurrent medications. Drug solubility may be substantially reduced at neutral pH compared with acidic conditions. In this context, PPIs have been shown to reduce the bioavailability of many clinically relevant drugs (e.g. ketoconazole, atazanavir) by 50% or more compared with the control values.
Soon after the introduction of omeprazole (a prototype PPI) into the market, it was reported that omeprazole was associated with 30% and 10% reductions in systemic clearance of diazepam and phenytoin, respectively. In vitro studies demonstrating the inhibitory effects of omeprazole on the metabolism of these drugs with human liver microsomes gave a mechanistic explanation for the DDIs. Numerous subsequent studies have been performed to investigate the DDI potential of PPIs associated with the metabolic inhibition of cytochrome P450 (CYP) enzyme activities; however, most such attempts have failed to find clinically relevant results.
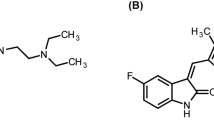
Nevertheless, recent large-scale clinical trials have raised concerns about possible DDIs between PPIs and an antiplatelet drug, clopidogrel. It has been suggested that coadministration of PPIs with a dual antiplatelet therapy consisting of clopidogrel and aspirin may attenuate the anti-aggregation effects of those medications and augment the risk of cardiovascular ischaemic events. There is a possibility that PPIs may elicit detrimental effects by inhibiting CYP2C19-dominated metabolism of clopidogrel to its active metabolite. Further studies are urgently required to clarify themechanism of this DDI and to explore new aspects of theDDI potential of PPIs.








Similar content being viewed by others
References
Shin JM, Sachs G. Pharmacology of proton pump inhibitors. Curr Gastroenterol Rep 2008 Dec; 10(6): 528–34
Shi S, Klotz U. Proton pump inhibitors: an update of their clinical use and pharmacokinetics. Eur J Clin Pharmacol 2008 Oct; 64(10): 935–51
Sugimoto M, Furuta T, Shirai N, et al. Treatment strategy to eradicate Helicobacter pylori infection: impact of pharmacogenomics-based acid inhibition regimen and alternative antibiotics. Expert Opin Pharmacother 2007 Nov; 8(16): 2701–17
Gugler R, Jensen JC. Omeprazole inhibits oxidative drug metabolism: studies with diazepam and phenytoin in vivo and 7-ethoxycoumarin in vitro. Gastroenterology 1985 Dec; 89(6): 1235–41
Blume H, Donath F, Warnke A, et al. Pharmacokinetic drug interaction profiles of proton pump inhibitors. Drug Saf 2006; 29(9): 769–84
Unge P, Andersson T. Drug interactions with proton pump inhibitors. Drug Saf 1997 Mar; 16(3): 171–9
Ho PM, Maddox TM, Wang L, et al. Risk of adverse outcomes associated with concomitant use of clopidogrel and proton pump inhibitors following acute coronary syndrome. JAMA 2009 Mar 4; 301(9): 937–44
Juurlink DN, Gomes T, Ko DT, et al. A population-based study of the drug interaction between proton pump inhibitors and clopidogrel. CMAJ 2009 Mar 31; 180(7): 713–8
Joerger M, Huitema AD, van den Bongard HJ, et al. Determinants of the elimination of methotrexate and 7-hydroxy-methotrexate following high-dose infusional therapy to cancer patients. Br J Clin Pharmacol 2006 Jul; 62(1): 71–80
Suzuki K, Doki K, Homma M, et al. Co-administration of proton pump inhibitors delays elimination of plasma methotrexate in high-dose metho-trexate therapy. Br J Clin Pharmacol 2009 Jan; 67(1): 44–9
Lahner E, Annibale B, Delle Fave G. Systematic review: impaired drug absorption related to the co-administration of antisecretory therapy. Aliment Pharmacol Ther 2009 Jun 15; 29(12): 1219–29
Spénard J, Aumais C, Massicotte J, et al. Influence of omeprazole on bioavailability of bismuth following administration of a triple capsule of bismuth biskalcitrate, metronidazole, and tetracycline. J Clin Pharmacol 2004 Jun; 44(6): 640–5
Treiber G, Walker S, Klotz U.Omeprazole-induced increaseinthe absorption of bismuth from tripotassium dicitrato bismuthate. Clin Pharmacol Ther 1994 May; 55(5): 486–91
Treiber G, Walker S, Klotz U. Omeprazole, amoxicillin and bismuth for peptic ulcer healing and Helicobacter pylori eradication. Arznei-mittelforschung 1997 Jan; 47(1): 47–50
Oosterhuis B, Jonkman JH, Andersson T, et al. Minor effect of multiple dose omeprazole on the pharmacokinetics of digoxin after a single oral dose. Br J Clin Pharmacol 1991 Nov; 32(5): 569–72
Hartmanna M, Huber R, Bliesath H, et al. Lack of interaction between pantoprazole and digoxinat therapeutic doses inman. Int J Clin Pharmacol Ther 1995 Sep; 33(9): 481–5
Le GH, Schaefer MG, Plowman BK, et al. Assessment of potential digoxinrabeprazole interaction after formulary conversion of proton-pump inhibitors. Am J Health Syst Pharm 2003 Jul 1; 60(13): 1343–5
Kiley CA, Cragin DJ, Roth BJ. Omeprazole-associated digoxin toxicity. South Med J 2007 Apr; 100(4): 400–2
Stuht H, Lode H, Koeppe P, et al. Interaction study of lomefloxacin and ciprofloxacin with omeprazole and comparative pharmacokinetics. Antimicrob Agents Chemother 1995 May; 39(5): 1045–9
Washington C, Hou E, Hughes N, et al. Effect of omeprazole on bioavailability of an oral extended-release formulation of ciprofloxacin. Am J Health Syst Pharm 2006 Apr 1; 63(7): 653–6
Allen A, Vousden M, Lewis A. Effect of omeprazole on the pharmacokinetics of oral gemifloxacin in healthy volunteers. Chemotherapy 1999 Nov-Dec; 45(6): 496–503
Gustavson LE, Kaiser JF, Edmonds AL, et al. Effect of omeprazole on concentrations of clarithromycin in plasma and gastric tissue at steady state. Antimicrob Agents Chemother 1995 Sep; 39(9): 2078–83
Ortiz RA, Calafatti SA, Moraes LA, et al. Effect of Helicobacter pylori infection and acid blockade by lansoprazole on clarithromycin bioavailability. Braz J Med Biol Res 2007 Mar; 40(3): 383–9
Kees F, Holstege A, Ittner KP, et al. Pharmacokinetic interaction between proton pump inhibitors and roxithromycin in volunteers. Aliment Pharmacol Ther 2000 Apr; 14(4): 407–12
Poli A, Moreno RA, Ribeiro W, et al. Influence of gastric acid secretion blockade and food intake on the bioavailability of a potassium diclofenac suspension in healthy male volunteers. Int J Clin Pharmacol Ther 1996 Feb; 34(2): 76–9
Andersson T, Bredberg E, Lagerstrom PO, et al. Lack of drug-drug interaction between three different non-steroidal anti-inflammatory drugs and omeprazole. Eur J Clin Pharmacol 1998 Jul; 54(5): 399–404
Bliesath H, Huber R, Steinijans VW, et al. Lack of pharmacokinetic interaction between pantoprazoleand diclofenac. Int J Clin Pharmacol Ther 1996 Apr; 34(4): 152–6
Tomilo DL, Smith PF, Ogundele AB, et al. Inhibition of atazanavir oral absorption by lansoprazole gastric acid suppression in healthy volunteers. Pharmacotherapy 2006 Mar; 26(3): 341–6
Klein CE, Chiu YL, Cai Y, et al. Effects of acid-reducing agents on the pharmacokinetics of lopinavir/ritonavir and ritonavir-boosted atazanavir. J Clin Pharmacol 2008 May; 48(5): 553–62
Sekar VJ, Lefebvre E, De Paepe E, et al. Pharmacokinetic interaction between darunavir boosted with ritonavir and omeprazole or ranitidine in human immunodeficiency virus-negative healthy volunteers. Antimicrob Agents Chemother 2007 Mar; 51(3): 958–61
Shelton MJ, Ford SL, Borland J, et al. Coadministration of esomeprazole with fosamprenavir has no impact on steady-state plasma amprenavir pharmacokinetics. J Acquir Immune Defic Syndr 2006 May; 42(1): 61–7
Tappouni HL, Rublein JC, Donovan BJ, et al. Effect of omeprazole on the plasma concentrations of indinavir when administered alone and in combination with ritonavir. Am J Health Syst Pharm 2008 Mar 1; 65(5): 422–8
Fang AF, Damle BD, LaBadie RR, et al. Significant decrease in nelfinavir systemic exposure after omeprazole coadministration in healthy subjects. Pharmacotherapy 2008 Jan; 28(1): 42–50
Iwamoto M, Wenning LA, Nguyen BY, et al. Effects of omeprazole on plasma levels of raltegravir. Clin Infect Dis 2009 Feb; 48(4): 489–92
Winston A, Back D, Fletcher C, et al. Effect of omeprazole on the pharm-acokinetics of saquinavir-500 mg formulation with ritonavir in healthy male and female volunteers. AIDS 2006 Jun 26; 20(10): 1401–6
Singh K, Dickinson L, Chaikan A, et al. Pharmacokinetics and safety of saquinavir/ritonavir and omeprazole in HIV-infected subjects. Clin Pharmacol Ther 2008 Jun; 83(6): 867–72
Zimmermann T, Yeates RA, Riedel KD, et al. The influence of gastric pH on the pharmacokinetics of fluconazole: the effect of omeprazole. Int J Clin Pharmacol Ther 1994 Sep; 32(9): 491–6
Jaruratanasirikul S, Sriwiriyajan S. Effect of omeprazole on the pharmacokinetics of itraconazole. Eur J Clin Pharmacol 1998 Apr; 54(2): 159–61
Johnson MD, Hamilton CD, Drew RH, et al. A randomized comparative study to determine the effect of omeprazole on the peak serum concentration of itraconazole oral solution. J Antimicrob Chemother 2003 Feb; 51(2): 453–7
Aciphex® (rabeprazole sodium) delayed-release tablets: US prescribing information. Woodcliff Lake (NJ): Eizai Inc., 2009 Jan [online]. Available from URL: http://www.aciphex.com/PDF/aciphexpi.pdf [Accessed 2010 Jun 16]
Krishna G, Moton A, Ma L, et al. Pharmacokinetics and absorption of posaconazole oral suspension under various gastric conditions in healthy volunteers. Antimicrob Agents Chemother 2009 Mar; 53(3): 958–66
Pommerien W, Braun M, Idstrom JP, et al. Pharmacokinetic and pharmacodynamic interactions between omeprazole and amoxycillin in Helicobacter pylori-positive healthy subjects. Aliment Pharmacol Ther 1996 Jun; 10(3): 295–301
Wittayalertpanya S, Wannachai N, Thongnopnua P, et al. Effect of omeprazole on gastric mucosa and serum levels of amoxicillin in patients with non-ulcer dyspepsia. J Med Assoc Thai 2000 Jun; 83(6): 611–8
Madaras-Kelly K, Michas P, George M, et al. A randomized crossover study investigating the influence of ranitidine or omeprazole on the pharmacokinetics of cephalexin monohydrate. J Clin Pharmacol 2004 Dec; 44(12): 1391–7
Zhang YF, Chen XY, Dai XJ, et al. Influence of omeprazole on pharmacokinetics of domperidone given as free base and maleate salt in healthy Chinese patients. Acta Pharmacol Sin 2007 Aug; 28(8): 1243–6
Calafatti SA, Ortiz RA, Deguer M, et al. Effect of acid secretion blockade by omeprazole on the relative bioavailability of orally administered furazolidone in healthy volunteers. Br J Clin Pharmacol 2001 Aug; 52(2): 205–9
Egorin MJ, Shah DD, Christner SM, et al. Effect of a proton pump inhibitor on imatinib pharmacokinetics. Br J Clin Pharmacol 2009 Sep; 68(3): 370–4
Kofler S, Deutsch MA, Bigdeli AK, et al. Proton pump inhibitor co-medication reduces mycophenolate acid drug exposure in heart transplant recipients. J Heart Lung Transplant 2009 Jun; 28(6): 605–11
Rupprecht K, Schmidt C, Raspe A, et al. Bioavailability of mycophenolate mofetil and enteric-coated mycophenolate sodium is differentially affected by pantoprazole in healthy volunteers. J Clin Pharmacol 2009 Oct; 49(10): 1196–201
Hussain FN, Ajjan RA, Moustafa M, et al. Mesalazine release from a pH dependent formulation: effects of omeprazole and lactulose co-administration. Br J Clin Pharmacol 1998 Aug; 46(2): 173–5
Dmochowski R, Chen A, Sathyan G, et al. Effect of the proton pump inhibitor omeprazole on the pharmacokinetics of extended-release formulations of oxybutynin and tolterodine. J Clin Pharmacol 2005 Aug; 45(8): 961–8
Palaparthy R, Pradhan RS, Chan J, et al. Effect of omeprazole on the pharmacokinetics of paricalcitol in healthy subjects. Biopharm Drug Dispos 2007 Mar; 28(2): 65–71
Chin TW, Loeb M, Fong IW. Effects of an acidic beverage (Coca-Cola) on absorption of ketoconazole. Antimicrob Agents Chemother 1995 Aug; 39(8): 1671–5
Prilosec® (omeprazole): US prescribing information. Wilmington (DE): AstraZeneca LP, 2010 [online]. Available from URL: http://www1.astrazeneca-us.com/pi/Prilosec.pdf [Accessed 2010 Jun 16]
Carlson JA, Mann HJ, Canafax DM. Effect of pH on disintegration and dissolution of ketoconazole tablets. Am J Hosp Pharm 1983 Aug; 40(8): 1334–6
Beique L, Giguere P, la Porte C, et al. Interactions between protease inhibitors and acid-reducing agents: a systematic review. HIV Med 2007 Sep; 8(6): 335–45
Atazanavir sulfate (Reyataz® capsules): interview form [in Japanese]. Tokyo: Bristol-Myers Squibb, 2005
Reyataz® (atazanavir sulfate) capsules: US prescribing information. Princeton (NJ): Bristol-Myers Squibb, 2010 Apr [online]. Available from URL: http://packageinserts.bms.com/pi/pi_reyataz.pdf [Accessed 2010 Jun 16]
Furtek KJ, Crum NF, Olson PE, et al. Proton pump inhibitor therapy in atazanavir-treated patients: contraindicated? J Acquir Immune Defic Syndr 2006 Mar; 41(3): 394–6
Sahloff EG, Duggan JM. Clinical outcomes associated with concomitant use of atazanavir and proton pump inhibitors. Ann Pharmacother 2006 Oct; 40(10): 1731–6
Nwokolo CU, Lewin JF, Hudson M, et al. Transmucosal penetration of bismuth particles in the human stomach. Gastroenterology 1992 Jan; 102(1): 163–7
Hassan-Alin M, Andersson T, Niazi M, et al. Studies on drug interactions between esomeprazole, amoxicillin and clarithromycin in healthy subjects. Int J Clin Pharmacol Ther 2006 Mar; 44(3): 119–27
Sanchez Navarro A. New formulations of amoxicillin/clavulanic acid: a pharmacokinetic and pharmacodynamic review. Clin Pharmacokinet 2005; 44(11): 1097–115
Cohen AF, Kroon R, Schoemaker R, et al. Influence of gastric acidity on the bioavailability of digoxin. Ann Intern Med 1991 Oct 1; 115(7): 540–5
Tanigawara Y, Okamura N, Hirai M, et al. Transport of digoxin by human P-glycoprotein expressed in a porcine kidney epithelial cell line (LLC-PK1). J Pharmacol Exp Ther 1992 Nov; 263(2): 840–5
Soons PA, van den Berg G, Danhof M, et al. Influence of single- and multiple-dose omeprazole treatment on nifedipine pharmacokinetics and effects in healthy subjects. Eur J Clin Pharmacol 1992; 42(3): 319–24
Bliesath H, Huber R, Steinijans VW, et al. Pantoprazole does not interact with nifedipine in man under steady-state conditions. Int J Clin Pharmacol Ther 1996 Feb; 34(2): 51–5
Meyer UA. Metabolic interactions of the proton-pump inhibitors lansoprazole, omeprazole and pantoprazole with other drugs. Eur J Gastroenterol Hepatol 1996 Oct; 8 Suppl. 1: S21–5
Klotz U. Clinical impact of CYP2C19 polymorphism on the action of proton pump inhibitors: a review of a special problem. Int J Clin Pharmacol Ther 2006; 44: 297–302
Wilkinson GR. Drug metabolism and variability among patients in drug response. N Engl J Med 2005; 352: 2211–21
Li XQ, Andersson TB, Ahlstrom M, et al. Comparison of inhibitory effects of the proton pump-inhibiting drugs omeprazole, esomeprazole, lansoprazole, pantoprazole, and rabeprazole on human cytochrome P450 activities. Drug Metab Dispos 2004 Aug; 32(8): 821–7
Center for Drug Evaluation and Research and Center for Biologics Evaluation and Research, US FDA. Guidance for industry. Drug metabolism/drug interaction studies in the drug development process: studies in vitro. Rock-ville (MD): US FDA, 1997 Apr [online]. Available from URL: http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/ucm072104.pdf [Accessed 2010 Jun 16]
Brown HS, Ito K, Galetin A, et al. Prediction of invivo drug-drug interactions from in vitro data: impact of incorporating parallel pathways of drug elimination and inhibitor absorption rate constant. Br J Clin Pharmacol 2005 Nov; 60(5): 508–18
Yu KS, Yim DS, Cho JY, et al. Effect of omeprazole on the pharmacokinetics of moclobemide according to the genetic polymorphism of CYP2C19. Clin Pharmacol Ther 2001 Apr; 69(4): 266–73
Andersson T, Cederberg C, Edvardsson G, et al. Effect of omeprazole treatment on diazepam plasma levels in slow versus normal rapid metabolizers of omeprazole. Clin Pharmacol Ther 1990 Jan; 47(1): 79–85
Gram LF, Guentert TW, Grange S, et al. Moclobemide, a substrate of CYP2C19 and an inhibitor of CYP2C19, CYP2D6, and CYP1A2: a panel study. Clin Pharmacol Ther 1995 Jun; 57(6): 670–7
Vossen M, Sevestre M, Niederalt C, et al. Dynamically simulating the inter- action of midazolam and the CYP3A4 inhibitor itraconazole using individual coupled whole-body physiologically-based pharmacokinetic (WB-PBPK) models. Theor Biol Med Model 2007 Mar 26; 4: 13
Almond LM, Yang J, Jamei M, et al. Towards a quantitative framework for the prediction of DDIs arising from cytochrome P450 induction. Curr Drug Metab 2009 May; 10(4): 420–32
Willmann S, Hohn K, Edginton A, et al. Development of a physiology-based whole-body population model for assessing the influence of individual variability on the pharmacokinetics of drugs. J Pharmacokinet Pharmacodyn 2007 Jun; 34(3): 401–31
Diaz D, Fabre I, Daujat M, et al. Omeprazole is an aryl hydrocarbon-like inducer of human hepatic cytochrome P450. Gastroenterology 1990 Sep; 99(3): 737–47
Ma Q, Lu AY. CYP1A induction and human risk assessment: an evolving tale of in vitro and in vivo studies. Drug Metab Dispos 2007 Jul; 35(7): 1009–16
Rost KL, Brosicke H, Heinemeyer G, et al. Specific and dose-dependent enzyme inductionbyomeprazoleinhuman beings. Hepatology 1994 Nov; 20(5): 1204–12
Rost KL, Brosicke H, Brockmoller J, et al. Increase of cytochrome P450IA2 activity by omeprazole: evidence by the 13C-[N-3-methyl]-caffeine breath test in poor and extensive metabolizers of S-mephenytoin. Clin Pharmacol Ther 1992 Aug; 52(2): 170–80
Sarich T, Kalhorn T, Magee S, et al. The effect of omeprazole pretreatment on acetaminophen metabolism in rapid and slow metabolizers of S-mepheny-toin. Clin Pharmacol Ther 1997 Jul; 62(1): 21–8
Andersson T, Bergstrand R, Cederberg C, et al. Omeprazole treatment does not affect the metabolism of caffeine. Gastroenterology 1991 Oct; 101(4): 943–7
Xiaodong S, Gatti G, Bartoli A, et al. Omeprazole does not enhance the metabolism of phenacetin, a marker of CYP1A2 activity, in healthy volunteers. Ther Drug Monit 1994 Jun; 16(3): 248–50
Rizzo N, Padoin C, Palombo S, et al. Omeprazole and lansoprazole are not inducers of cytochrome P4501A2 under conventional therapeutic conditions. Eur J Clin Pharmacol 1996; 49(6): 491–5
Hartmann M, Zech K, Bliesath H, et al. Pantoprazole lacks induction of CYP1A2 activity in man. Int J Clin Pharmacol Ther 1999 Apr; 37(4): 159–64
Beorlegui B, Aldaz A, Ortega A, et al. Potential interaction between metho-trexate and omeprazole. Ann Pharmacother 2000 Sep; 34(9): 1024–7
Bauters TG, Verlooy J, Robays H, et al. Interaction between methotrexate and omeprazole in an adolescent with leukemia: a case report. Pharm World Sci 2008 Aug; 30(4): 316–8
Bhatt DL, Scheiman J, Abraham NS, et al. ACCF/ACG/AHA 2008 expert consensus document on reducing the gastrointestinal risks of antiplatelet therapy and NSAID use: a report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents. J Am Coll Cardiol 2008 Oct 28; 52(18): 1502–17
Yusuf S, Zhao F, Mehta SR, et al., Clopidogrel inUnstable Angina to Prevent Recurrent Events Trial Investigators. Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation [published erratum appears in N Engl J Med 2001 Nov 15; 345 (20): 1506]. N Engl J Med 2001 Aug 16; 345(7): 494–502
Peters RJ, Mehta SR, Fox KA, et al. Effects of aspirin dose when used alone or in combination with clopidogrel in patients with acute coronary syndromes: observations from the Clopidogrel in Unstable Angina to Prevent Recurrent Events (CURE) study. Circulation 2003 Oct 7; 108(14): 1682–7
Evanchan J, Donnally MR, Binkley P, et al. Recurrence of acute myocardial infarction inpatients discharged on clopidogrel and a proton pump inhibitor after stent placement for acute myocardial infarction. Clin Cardiol 2010 Mar; 33(3): 168–71
Gaglia Jr MA, Torguson R, Hanna N, et al. Relation of proton pump inhibitor use after percutaneous coronary intervention with drug-eluting stents to outcomes. Am J Cardiol 2010 Mar; 105(6): 833–8
Stockl KM, Le L, Zakharyan A, et al. Risk of rehospitalization for patients using clopidogrel with a proton pump inhibitor. Arch Intern Med 2010 Apr; 170(8): 704–10
Kwok CS, Loke YK. Meta-analysis: the effects of proton pump inhibitors on cardiovascular events and mortality in patients receiving clopidogrel. Aliment Pharmacol Ther 2010 Apr; 31(8): 810–23
O’Donoghue ML, Braunwald E, Antman EM, et al. Pharmacodynamic effect and clinical efficacy of clopidogrel and prasugrel with or without a proton-pump inhibitor: an analysis of two randomized trials. Lancet 2009 Sep 19; 374(9694): 989–97
Rassen JA, Choudhry NK, Avorn J, et al. Cardiovascular outcomes and mortality in patients using clopidogrel with proton pump inhibitors after percutaneous coronary intervention or acute coronary syndrome. Circulation 2009 Dec; 120(23): 2322–9
Ray WA, Murray KT, Griffin MR, et al. Outcomes with concurrent use of clopidogrel and proton-pump inhibitors: a cohort study. Ann Intern Med 2010 Mar; 152(6): 337–45
Zairis MN, Tsiaousis GZ, Patsourakos NG, et al. The impact of treatment with omeprazole on the effectiveness of clopidogrel drug therapy during the first year after successful coronary stenting. Can J Cardiol 2010 Feb; 26 (2): e54–7
US FDA. Information for healthcare professionals: update to the labeling of clopidogrel bisulfate (marketed as Plavix) to alert healthcare professionals about a drug interaction with omeprazole (marketed as Prilosec and Prilosec OTC). Rockville (MD): US FDA, 2009 Nov 17 [online]. Available from URL: http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/DrugSafetyInformationforHeathcareProfessionals/ucm190787.htm [Accessed 2010 Jun 16]
European Medicines Agency. Public statement on possible interaction between clopidogrel and proton pump inhibitors [document reference EMEA/328956/2009]. London: European Medicines Agency, 2009 May 29 [online]. Available from URL: http://www.ema.europa.eu/humandocs/PDFs/EPAR/Plavix/32895609en.pdf [Accessed 2010 Jun 16]
Geisler T, Schaeffeler E, Dippon J, et al. CYP2C19 and nongenetic factors predict poor responsiveness to clopidogrel loading dose after coronary stent implantation. Pharmacogenomics 2008 Sep; 9(9): 1251–9
Gilard M, Arnaud B, Cornily JC, et al. Influence of omeprazole on the antiplatelet action of clopidogrel associated with aspirin: the randomized, double-blind OCLA (Omeprazole Clopidogrel Aspirin) study. J Am Coll Cardiol 2008 Jan 22; 51(3): 256–60
Cuisset T, Frere C, Quilici J, et al. Comparison of omeprazole and panto- prazole influence on a high 150-mg clopidogrel maintenance dose the PACA (Proton Pump Inhibitors And Clopidogrel Association) prospective randomized study. J Am Coll Cardiol 2009 Sep 22; 54(13): 1149–53
Siller-Matula JM, Spiel AO, Lang IM, et al. Effects of pantoprazole and esomeprazole on platelet inhibitionby clopidogrel. Am Heart J 2009 Jan; 157(1): 148.e1–5
Kim KA, Park PW, Hong SJ, et al. The effect of CYP2C19 polymorphism on the pharmacokinetics and pharmacodynamics of clopidogrel: a possible mechanism for clopidogrel resistance.Clin Pharmacol Ther 2008 Aug; 84(2): 236–42
Mega JL, Close SL, Wiviott SD, et al. Cytochrome p-450 polymorphisms and response to clopidogrel. N Engl J Med 2009 Jan 22; 360(4): 354–62
Shuldiner AR, O’Connell JR, Bilden KP, et al. Association of cytochrome P450 2C19 genotype with the antiplatelet effect and clinical efficacy of clopidogrel therapy. JAMA 2009 Aug 26; 302(8): 849–57
Simon T, Verstuyft C, Mary-Krause M, et al. Genetic determinants of response to clopidogrel and cardiovascular events. N Engl J Med 2009 Jan 22; 360(4): 363–75
Savi P, Pereillo JM, Uzabiaga MF, et al. Identification and biological activity of the active metabolite of clopidogrel. Thromb Haemost 2000 Nov; 84(5): 891–6
Caplain H, Donat F, Gaud C, et al. Pharmacokinetics of clopidogrel. Semin Thromb Hemost 1999; 25 Suppl. 2: 25–8
Lins R, Broekhuysen J, Necciari J, et al. Pharmacokinetic profile of 14C- labeled clopidogrel. Semin Thromb Hemost 1999; 25 Suppl. 2: 29–33
Clarke TA, Waskell LA. The metabolism of clopidogrelis catalyzed byhuman cytochrome P450 3A and is inhibited by atorvastatin. Drug Metab Dispos 2003 Jan; 31(1): 53–9
Farid NA, Payne CD, Small DS, et al. Cytochrome P450 3A inhibition by ketoconazole affects prasugrel and clopidogrel pharmacokinetics and pharmacodynamics differently. Clin Pharmacol Ther 2007 May; 81(5): 735–41
Umemura K, Furuta T, Kondo K. The common gene variants of CYP2C19 affect pharmacokinetics and pharmacodynamics in an active metabolite of clopidogrel in healthy subjects. J Thromb Haemost 2008 Aug; 6(8): 1439–41
Brandt JT, Close SL, Iturria SJ, et al. Common polymorphisms of CYP2C19 and CYP2C9 affect the pharmacokinetic and pharmacodynamic response to clopidogrel but not prasugrel. J Thromb Haemost 2007 Dec; 5(12): 2429–36
Ko JW, Sukhova N, Thacker D, et al. Evaluation of omeprazole and lanso- prazole asinhibitors of cytochrome P450 isoforms. Drug Metab Dispos 1997 Jul; 25(7): 853–62
Goddard AF, Jessa MJ, Barrett DA, et al. Effect of omeprazole on the distribution of metronidazole, amoxicillin, and clarithromycin in human gastric juice. Gastroenterology 1996 Aug; 111(2): 358–67
Grayson ML, Eliopoulos GM, Ferraro MJ, et al. Effect of varying pH on the susceptibility of Campylobacter pylori to antimicrobial agents. Eur J Clin Microbiol Infect Dis 1989 Oct; 8(10): 888–9
Andersson T, Miners JO, Veronese ME, et al. Identification of human liver cytochrome P450 isoforms mediating omeprazole metabolism. Br J Clin Pharmacol 1993 Dec; 36(6): 521–30
Andersson T, Andren K, Cederberg C, et al. Effect of omeprazole and ci- metidine on plasma diazepam levels. Eur J Clin Pharmacol 1990; 39(1): 51–4
Ishizaki T, Chiba K, Manabe K, et al. Comparison of the interaction potential of a new proton pump inhibitor, E3810, versus omeprazole with diazepam in extensive and poor metabolizers of S-mephenytoin 4′ -hydroxylation. Clin Pharmacol Ther 1995 Aug; 58(2): 155–64
Caraco Y, Tateishi T, Wood AJ. Interethnic difference in omeprazoleś inhibition of diazepam metabolism. Clin Pharmacol Ther 1995 Jul; 58(1): 62–72
Scholler-Gyure M, Kakuda TN, De Smedt G, et al. A pharmacokinetic study of etravirine (TMC125) co-administered with ranitidine and omeprazole in HIV-negative volunteers. Br J Clin Pharmacol 2008 Oct; 66(4): 508–16
Funck-Brentano C, Becquemont L, Lenevu A, et al. Inhibition by omeprazole of proguanil metabolism: mechanism of the interaction in vitro and prediction of in vivo results from theinvitro experiments.J Pharmacol Exp Ther 1997 Feb; 280(2): 730–8
Wood N, Tan K, Purkins L, et al. Effect of omeprazole on the steady-state pharmacokinetics of voriconazole. Br J Clin Pharmacol 2003 Dec; 56 Suppl. 1: 56–61
de Hoon JN, Thijssen HH, Beysens AJ, et al. No effect of short-term ome- prazole intake on acenocoumarol pharmacokinetics and pharmaco-dynamics. Br J Clin Pharmacol 1997 Oct; 44(4): 399–401
Henry DA, Somerville KW, Kitchingman G, et al. Omeprazole: effects on oxidative drug metabolism. Br J Clin Pharmacol 1984 Aug; 18(2): 195–200
Quinn DI, Nemunaitis J, Fuloria J, et al. Effect of the cytochrome P450 2C19 inhibitor omeprazole on the pharmacokinetics and safety profile of borte-zomib in patients with advanced solid tumours, non-Hodgkin’s lymphoma or multiple myeloma. Clin Pharmacokinet 2009; 48(3): 199–209
Dixit RK, Chawla AV, Kumar N, et al. Effect of omeprazole on the pharmacokinetics of sustained-release carbamazepine in healthy male volunteers. Methods Find Exp Clin Pharmacol 2001 Jan-Feb; 23(1): 37–9
Suri A, Bramer SL. Effect of omeprazole on the metabolism of cilostazol. Clin Pharmacokinet 1999; 37 Suppl. 2: 53–9
Arranz R, Yanez E, Franceschi JL, et al. More about omeprazole-cyclo- sporine interaction. Am J Gastroenterol 1993 Jan; 88(1): 154–5
Castellote E, Bonet J, Lauzurica R, et al. Does interaction between omepra- zole and cyclosporin exist? [letter] Nephron 1993; 65(3): 478
Blohme I, Idstrom JP, Andersson T. A study of the interaction between omeprazole and cyclosporine in renal transplant patients. Br J Clin Pharmacol 1993 Feb; 35(2): 156–60
Schouler L, Dumas F, Couzigou P, et al. Omeprazole-cyclosporin interaction [letter]. Am J Gastroenterol 1991 Aug; 86(8): 1097
Rocha A, Coelho EB, Sampaio SA, et al. Omeprazole preferentially inhibits the metabolism of (+)-(S)-citalopram in healthy volunteers. Br J Clin Pharmacol In press
Portolés A, Calvo A, Terleira A, et al. Lack of pharmacokinetic interaction between omeprazole or lansoprazole and ivabradine in healthy volunteers: an open-label, randomized, crossover, pharmacokinetic interaction clinical trial. J Clin Pharmacol 2006 Oct; 46(10): 1195–203
Noble DW, Bannister J, Lamont M, et al. The effect oforal omeprazole onthe disposition of lignocaine. Anaesthesia 1994 Jun; 49(6): 497–500
Andersson T, Lundborg P, Regardh CG. Lack of effect of omeprazole treatment on steady-state plasma levels of metoprolol. Eur J Clin Pharmacol 1991; 40(1): 61–5
David FL, Da Silva CM, Mendes FD, et al. Acid suppression by omeprazole does not affect orally administered metronidazole bioavailability and metabolism in healthy male volunteers. Aliment Pharmacol Ther 1998 Apr; 12(4): 349–54
Prichard PJ, Walt RP, Kitchingman GK, et al. Oral phenytoin pharmacokinetics during omeprazole therapy. Br J Clin Pharmacol 1987 Oct; 24(4): 543–5
Bachmann KA, Sullivan TJ, Jauregui L, et al. Absence of an inhibitory effect of omeprazole and nizatidine on phenytoin disposition, a marker of CYP2C activity. Br J Clin Pharmacol 1993 Oct; 36(4): 380–2
Andersson T, Lagerstrom PO, Unge P. A study of the interaction between omeprazole and phenytoin in epileptic patients. Ther Drug Monit 1990 Jul; 12(4): 329–33
Cavanaugh JH, Karol MD. Lack of pharmacokinetic interaction after administration of lansoprazole or omeprazole with prednisone. J Clin Pharmacol 1996 Nov; 36(11): 1064–71
Henry D, Brent P, Whyte I, et al. Propranolol steady-state pharmacokinetics are unaltered by omeprazole. Eur J Clin Pharmacol 1987; 33(4): 369–73
Ching MS, Elliott SL, Stead CK, et al. Quinidine single dose pharmacokinetics and pharmacodynamics are unaltered by omeprazole. Aliment Pharmacol Ther 1991 Oct; 5(5): 523–31
Lemahieu WP, Maes BD, Verbeke K, et al. Impact of gastric acid suppressants on cytochrome P450 3A4 and P-glycoprotein: consequences for FK506 assimilation. Kidney Int 2005 Mar; 67(3): 1152–60
Moreau C, Debray D, Loriot MA, et al. Interaction between tacrolimus and omeprazole in a pediatric liver transplant recipient. Transplantation 2006 Feb 15; 81(3): 487–8
Takahashi K, Yano I, Fukuhara Y, et al. Distinct effects of omeprazole and rabeprazole on the tacrolimus blood concentration in a kidney transplant recipient. Drug Metab Pharmacokinet 2007 Dec; 22(6): 441–4
Oosterhuis B, Jonkman JH, Andersson T, et al. No influence of single intravenous doses of omeprazole on theophylline elimination kinetics. J Clin Pharmacol 1992 May; 32(5): 470–5
Taburet AM, Geneve J, Bocquentin M, et al. Theophylline steady state pharmacokinetics is not altered by omeprazole. Eur J Clin Pharmacol 1992; 42(3): 343–5
Dilger K, Zheng Z, Klotz U. Lack of drug interaction between omeprazole, lansoprazole, pantoprazole and theophylline. Br J Clin Pharmacol 1999 Sep; 48(3): 438–44
Uno T, Sugimoto K, Sugawara K, et al. The role of cytochrome P2C19 in R-warfarin pharmacokinetics and its interaction with omeprazole. Ther Drug Monit 2008 Jun; 30(3): 276–81
Unge P, Svedberg LE, Nordgren A, et al. A study of the interaction of omeprazole and warfarin in anticoagulated patients. Br J Clin Pharmacol 1992 Dec; 34(6): 509–12
Sutfin T, Balmer K, Bostrom H, et al. Stereoselective interaction of omeprazole with warfarin in healthy men. Ther Drug Monit 1989; 11(2): 176–84
Giancarlo GM, Venkatakrishnan K, Granda BW, et al. Relative contributions of CYP2C9 and 2C19 to phenytoin 4-hydroxylation in vitro: inhibition by sulfaphenazole, omeprazole, and ticlopidine. Eur J Clin Pharmacol 2001 Apr; 57(1): 31–6
Kerr BM, Thummel KE, Wurden CJ, et al. Human liver carbamazepine metabolism: role of CYP3A4 and CYP2C8 in 10,11-epoxide formation. Biochem Pharmacol 1994 Jun 1; 47(11): 1969–79
Guengerich FP, Martin MV, Beaune PH, et al. Characterization of rat and human liver microsomal cytochrome P-450 forms involved in nifedipine oxidation, prototype for genetic polymorphism in oxidative drug metabolism. J Biol Chem 1986 Apr 15; 261(11): 5051–60
Dettmar PW, Hampson FC, Jain A, et al. Administration of analginate based gastric reflux suppressant on the bioavailabilityof omeprazole. Indian JMed Res 2006 Apr; 123(4): 517–24
Takahata T, Yasui-Furukori N, Yoshiya G, et al. Fexofenadine does not affect omeprazole pharmacokinetics: both are putative P-glycoprotein substrates. Basic Clin Pharmacol Toxicol 2004 May; 94(5): 252–6
Howden CW, Reid JL. The effect of antacids and metoclopramide on omeprazole absorption and disposition. Br J Clin Pharmacol 1988 Jun; 25(6): 779–81
Iwao K, Saitoh H, Takeda K, et al. Decreased plasma levels of omeprazole after coadministration with magnesium-aluminium hydroxide dry suspension granules [in Japanese]. Yakugaku Zasshi 1999 Mar; 119(3): 221–8
Svensson US, Ashton M, Trinh NH, et al. Artemisinin induces omeprazole metabolism in human beings. Clin Pharmacol Ther 1998 Aug; 64(2): 160–7
Calabresi L, Pazzucconi F, Ferrara S, et al. Pharmacokinetic interactions between omeprazole/pantoprazole and clarithromycin in healthy volunteers. Pharmacol Res 2004 May; 49(5): 493–9
Chen BL, Chen Y, Tu JH, et al. Clopidogrel inhibits CYP2C19-dependent hydroxylation of omeprazole related to CYP2C19 genetic polymorphisms. J Clin Pharmacol 2009 May; 49(5): 574–81
Kang BC, Yang CQ, Cho HK, et al. Influence of fluconazole on the pharm- acokinetics of omeprazole in healthy volunteers. Biopharm Drug Dispos 2002 Mar; 23(2): 77–81
Yasui-Furukori N, Takahata T, Nakagami T, et al. Different inhibitory effect of fluvoxamine on omeprazole metabolism between CYP2C19 genotypes. Br J Clin Pharmacol 2004 Apr; 57(4): 487–94
Yin OQ, Tomlinson B, Waye MM, et al. Pharmacogenetics and herb-drug interactions: experience with Ginkgo biloba and omeprazole. Pharmaco-genetics 2004 Dec; 14(12): 841–50
Bottiger Y, Tybring G, Gotharson E, et al. Inhibition of the sulfoxidation of omeprazole by ketoconazole in poor and extensive metabolizers of S-me-phenytoin. Clin Pharmacol Ther 1997 Oct; 62(4): 384–91
Cho JY, Yu KS, Jang IJ, et al. Omeprazole hydroxylation is inhibited by a single dose of moclobemide in homozygotic EM genotype for CYP2C19. Br J Clin Pharmacol 2002 Apr; 53(4): 393–7
Leucuta A, Vlase L, Farcau D, et al. A pharmacokinetic interaction study between omeprazole and the H2-receptor antagonist ranitidine. Drug Metabol Drug Interact 2004; 20(4): 273–81
Wang LS, Zhou G, Zhu B, et al. St John’s wort induces both cytochrome P450 3A4-catalyzed sulfoxidation and 2C19-dependent hydroxylation of omeprazole. Clin Pharmacol Ther 2004 Mar; 75(3): 191–7
Fan L, Wang G, Wang LS, et al. Herbal medicine yin zhi huang induces CYP3A4-mediated sulfoxidation and CYP2C19-dependent hydroxylation of omeprazole. Acta Pharmacol Sin 2007 Oct; 28(10): 1685–92
Andersson T, Weidolf L. Stereoselective disposition of proton pump inhibitors. Clin Drug Investig 2008; 28(5): 263–79
Schwab M, Klotz U, Hofmann U, et al. Esomeprazole-induced healing of gastroesophageal reflux disease is unrelated to the genotype of CYP2C19: evidence from clinical and pharmacokinetic data. Clin Pharmacol Ther 2005 Dec; 78(6): 627–34
St Peter JV, Awni WM, Granneman GR, et al. The effects of lansoprazole on the disposition of antipyrine and indocyanine green in normal human subjects. Am J Ther 1995 Aug; 2(8): 561–8
Lefebvre RA, Flouvat B, Karolac-Tamisier S, et al. Influence of lansoprazole treatment on diazepam plasma concentrations. Clin Pharmacol Ther 1992 Nov; 52(5): 458–63
Sanaka M, Kuyama Y, Mineshita S, et al. Pharmacokinetic interaction between acetaminophen and lansoprazole. J Clin Gastroenterol 1999 Jul; 29(1): 56–8
Karol MD, Locke CS, Cavanaugh JH. Lack of pharmacokinetic interaction between lansoprazole and intravenously administered phenytoin. J Clin Pharmacol 1999 Dec; 39(12): 1283–9
Small DS, Farid NA, Payne CD, et al. Effects of the proton pump inhibitor lansoprazole on the pharmacokinetics and pharmacodynamics of prasugrel and clopidogrel. J Clin Pharmacol 2008 Apr; 48(4): 475–84
Karol MD, Locke CS, Cavanaugh JH. Lack of interaction between lansoprazole and propranolol, a pharmacokinetic and safety assessment. J Clin Pharmacol 2000 Mar; 40(3): 301–8
Itagaki F, Homma M, Yuzawa K, et al. Effect of lansoprazole and rabeprazole on tacrolimus pharmacokinetics in healthy volunteers with CYP2C19 mutations. J Pharm Pharmacol 2004 Aug; 56(8): 1055–9
Itagaki F, Homma M, Yuzawa K, et al. Drug interaction of tacrolimus and proton pump inhibitors in renal transplant recipients with CYP2C19 gene mutation. Transplant Proc 2002 Nov; 34(7): 2777–8
Takahashi K, Motohashi H, Yonezawa A, et al. Lansoprazole-tacrolimus interaction in Japanese transplant recipient with CYP2C19 polymorphism. Ann Pharmacother 2004 May; 38(5): 791–4
Hosohata K, Masuda S, Ogura Y, et al. Interaction between tacrolimus and lansoprazole, but not rabeprazole in living-donor liver transplant patients with defects of CYP2C19 and CYP3A5. Drug Metab Pharmacokinet 2008; 23(2): 134–8
Kokufu T, Ihara N, Sugioka N, et al. Effects of lansoprazole on pharmaco- kinetics and metabolism of theophylline. Eur J Clin Pharmacol 1995; 48(5): 391–5
Granneman GR, Karol MD, Locke CS, et al. Pharmacokinetic interaction between lansoprazole and theophylline. Ther Drug Monit 1995 Oct; 17(5): 460–4
Pan WJ, Goldwater DR, Zhang Y, et al. Lack of a pharmacokinetic interaction between lansoprazole or pantoprazole and theophylline. Aliment Pharmacol Ther 2000 Mar; 14(3): 345–52
Vakily M, Lee RD, Wu J, et al. Drug interaction studies with dexlansoprazole modified release (TAK-390MR), a proton pump inhibitor with a dual delayed-release formulation: results of four randomized, double-blind, crossover, placebo-controlled, single-centre studies. Clin Drug Investig 2009; 29(1): 35–50
Miura M, Inoue K, Kagaya H, et al. Influence of rabeprazole and lansopra-zole on the pharmacokinetics of tacrolimus in relation to CYP2C19, CYP3A5 and MDR1 polymorphisms in renal transplant recipients. Bio-pharm Drug Dispos 2007 May; 28(4): 167–75
Westphal JF. Macrolide-induced clinically relevant drug interactions with cytochrome P-450A (CYP) 3A4: an update focused on clarithromycin, azithromycin and dirithromycin. Br J Clin Pharmacol 2000 Oct; 50(4): 285–95
Yao C, Kunze KL, Trager WF, et al. Comparison of in vitro and in vivo inhibition potencies of fluvoxamine toward CYP2C19. Drug Metab Dispos 2003 May; 31(5): 565–71
Saito M, Yasui-Furukori N, Uno T, et al. Effects of clarithromycin on lansoprazole pharmacokinetics between CYP2C19 genotypes. Br J Clin Pharmacol 2005 Mar; 59(3): 302–9
Yasui-Furukori N, Saito M, Uno T, et al. Effects of fluvoxamine on lansoprazole pharmacokinetics in relation to CYP2C19 genotypes. J Clin Pharmacol 2004 Nov; 44(11): 1223–9
Miura M, Tada H, Yasui-Furukori N, et al. Effect of clarithromycin on the enantioselective disposition of lansoprazole in relation to CYP2C19 genotypes. Chirality 2005 Jun; 17(6): 338–44
Miura M, Tada H, Yasui-Furukori N, et al. Enantioselective disposition of lansoprazole in relation to CYP2C19 genotypes in the presence of fluvoxamine. Br J Clin Pharmacol 2005 Jul; 60(1): 61–8
Gugler R, Hartmann M, Rudi J, et al. Lack of pharmacokinetic interaction of pantoprazole with diazepam in man. Br J Clin Pharmacol 1996 Aug; 42(2): 249–52
Walter-Sack IE, Bliesath H, Stotzer F, et al. Lack of pharmacokinetic and pharmacodynamic interaction between pantoprazole and glibenclamide in humans. Clin Drug Investig 1998 Mar; 15(3): 253–60
De Mey C, Meineke I, Steinijans VW, et al. Pantoprazole lacks interaction with antipyrine in man, either by inhibition or induction. Int J Clin Pharmacol Ther 1994 Feb; 32(2): 98–106
Middle MV, Muller FO, Schall R, et al. No influence of pantoprazole on the pharmacokinetics of phenytoin. Int J Clin Pharmacol Ther 1995 May; 33(5): 304–7
Schulz HU, Hartmann M, Steinijans VW, et al. Lack of influence of pantoprazole on the disposition kinetics of theophylline in man. Int J Clin Pharmacol Ther Toxicol 1991 Sep; 29(9): 369–75
Shimizu M, Uno T, Yasui-Furukori N, et al. Effects of clarithromycin and verapamil on rabeprazole pharmacokinetics between CYP2C19 genotypes. Eur J Clin Pharmacol 2006 Aug; 62(8): 597–603
Uno T, Shimizu M, Yasui-Furukori N, et al. Different effects of fluvoxamine on rabeprazole pharmacokinetics in relation to CYP2C19 genotype status. Br J Clin Pharmacol 2006 Mar; 61(3): 309–14
Yasuda S, Higashi S, Murakami M, et al. Antacids have no influence on the pharmacokinetics of rabeprazole, a new proton pump inhibitor, in healthy volunteers. Int J Clin Pharmacol Ther 1999 May; 37(5): 249–53
Cheer SM, Prakash A, Faulds D, et al. Pantoprazole: an update of its pharmacological properties and therapeutic use in the management of acidrelated disorders. Drugs 2003; 63(1): 101–33
Huber R, Bliesath H, Hartmann M, et al. Pantoprazole does not interact with the pharmacokinetics of carbamazepine. Int J Clin Pharmacol Ther 1998 Oct; 36(10): 521–4
Ferron GM, Paul JC, Fruncillo RJ, etal. Lackof pharmacokinetic interaction between oral pantoprazole and cisapride in healthy adults. J Clin Pharmacol 1999 Sep; 39(9): 945–50
Lorf T, Ramadori G, Ringe B, et al. Pantoprazole does not affect cyclosporin A blood concentration in kidney-transplant patients. Eur J Clin Pharmacol 2000 Jan; 55(10): 733–5
Lorf T, Ramadori G, Ringe B, et al. The effect of pantoprazole on tacrolimus and cyclosporin A blood concentration in transplant recipients. Eur J Clin Pharmacol 2000 Aug; 56(5): 439–40
Koch HJ, Hartmann M, Bliesath H, et al. Pantoprazole has no influence on steady state pharmacokinetics and pharmacodynamics of metoprolol in healthy volunteers. Int J Clin Pharmacol Ther 1996 Oct; 34(10): 420–3
Ehrlich A, Fuder H, Hartmann M, et al. Lack of pharmacodynamic and pharmacokinetic interaction between pantoprazole and phenprocoumon in man. Eur J Clin Pharmacol 1996; 51(3-4): 277–81
Duursema L, Muller FO, Schall R, et al. Lack of effect of pantoprazole on the pharmacodynamics and pharmacokinetics of warfarin. Br J Clin Pharmacol 1995 Jun; 39(6): 700–3
Yasuda S, Horai Y, Tomono Y, et al. Comparison of the kinetic disposition and metabolism of E3810, a new proton pump inhibitor, and omeprazole in relation to S-mephenytoin 4′ -hydroxylation status. Clin Pharmacol Ther 1995 Aug; 58(2): 143–54
Huang SM, Strong JM, Zhang L, et al. New era in drug interaction evaluation: US Food and Drug Administration update on CYP enzymes, transporters, and the guidance process. J Clin Pharmacol 2008 Jun; 48(6): 662–70
Trenk D. Proton pump inhibitors for prevention of bleeding episodes in cardiac patients with dual antiplatelet therapy: between Scylla and Cha-rybdis? Int J Clin Pharmacol Ther 2009 Jan; 47(1): 1–10
Acknowledgements
No sources of funding were used to assist in the preparation of this review. The authors have no conflicts of interest that are directly relevant to the content of this review.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ogawa, R., Echizen, H. Drug-Drug Interaction Profiles of Proton Pump Inhibitors. Clin Pharmacokinet 49, 509–533 (2010). https://doi.org/10.2165/11531320-000000000-00000
Published:
Issue Date:
DOI: https://doi.org/10.2165/11531320-000000000-00000