Abstract
Background
Postoperative mortality is frequently used in hospital comparisons as marker for quality of care. Differences in mortality between hospitals may be explained by varying complication rates. A possible modifying factor may be the ability to let patients with a serious complication survive, referred to as failure to rescue (FTR). The purpose of this study was to evaluate how hospital performance on postoperative mortality is related to severe complications or to FTR and to explore the value of FTR in quality improvement programs.
Methods
All patients operated for colorectal cancer from 2009 to 2011, registered in the Dutch Surgical Colorectal Audit, were included. Logistic regression models were used to obtain adjusted mortality, complication, and FTR rates. Hospitals were grouped into 5 quintiles according to adjusted mortality. Outcomes were compared between quintiles.
Results
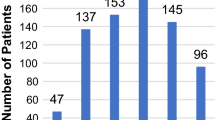
A total of 24,667 patients were included. Severe complications ranged from 19 % in the lowest to 25 % in the highest mortality quintile (odds ratio 1.5, 95 % confidence interval 1.37–1.67). Risk-adjusted FTR rates showed a marked difference between the quintiles, ranging from 9 % to 26 % (odds ratio 3.0, 95 % confidence interval 2.29–3.98). There was significant variability in FTR rates. Seven hospitals had significantly lower FTR rates than average.
Conclusions
High-mortality hospitals had slightly higher rates of severe complications than low-mortality hospitals. However, FTR was three times higher in high-mortality hospitals than in low-mortality hospitals. In quality improvement projects, feedback to hospitals of FTR rates, along with complication rates, may illustrate shortcomings (prevention or management of complications) per hospital, which may be an important step in reducing mortality.


Similar content being viewed by others
References
Almoudaris AM, Burns EM, Bottle A, et al. Single measures of performance do not reflect overall institutional quality in colorectal cancer surgery. Gut. 2013;62:523–9.
Zheng H, Zhang W, Ayanian JZ, et al. Profiling hospitals by survival of patients with colorectal cancer. Health Serv Res. 2011;46:729–46.
Kolfschoten NE, Marang van de Mheen PJ, Gooiker GA, et al. Variation in case-mix between hospitals treating colorectal cancer patients in the Netherlands. Eur J Surg Oncol. 2011;37:956–63.
Silber JH, Rosenbaum PR, Schwarz JS, et al. Evaluation of the complication rate as a measure of quality of care in coronary artery bypass graft surgery. JAMA. 1995;274:317–23.
Ghaferi AA, Birkmeyer JD, Dimick JB. Variation in hospital mortality associated with inpatient surgery. N Engl J Med. 2009;361:1368–75.
Ghaferi AA, Birkmeyer JD, Dimick JB. Hospital volume and failure to rescue with high-risk surgery. Med Care. 2011;49:1076–81.
Ghaferi AA, Birkmeyer JD, Dimick JD. Complications, failure to rescue, and mortality with major inpatient surgery in medicare patients. Ann Surg. 2009;250:1029–34.
Almoudaris AM, Burns EM, Mamidanna R, et al. Value of failure to rescue as a marker of the standard of care following reoperation for complications after colorectal resection. Br J Surg. 2011;98:1775–83.
Longo WE, Vorgo KS, Johnson FE, et al. Risk factors for morbidity and mortality after colectomy for colon cancer. Dis Colon Rectum. 2000;43:83–91.
Horwitz LI, Cuny JF, Cerese J, et al. Failure to Rescue, Validation of an algorithm using administrative data. Med Care. 2007;45:283–7.
Moriarty JP, Finnie DM, Johnson MG, et al. Do pre-existing complications affect the failure to rescue quality measures? Qual Saf Health Care. 2010;19:65–8.
Dutch Surgical Colorectal Audit. Annual report, 2009. http://www.clinicalaudit.nl.
Dutch Surgical Colorectal Audit. Annual report, 2010. http://www.clinicalaudit.nl.
Dutch Institute for Clinical Auditing. Annual reports, 2011. http://www.clinicalaudit.nl.
Gooiker GA, Dekker JWT, Bastiaannet E, et al. Risk factors for excess mortality in the first year after curative surgery for colorectal cancer. Ann Surg Oncol. 2012;19:2428–34.
Visser BC, Keegan H, Martin, et al. Death after colectomy: it’s later than we think. Arch Surg. 2009;144:1021–7.
Dekker JW, van den Broek CB, Bastiaannet E, et al. Importance of the first postoperative year in the prognosis of elderly colorectal cancer patients. Ann Surg Oncol. 2011;18:1533–9.
Lang TA, Hodge M, Olson V, et al. Nurse–patient ratios. J Nurs adm. 2004;34:326–37.
Ghaferi AA, Osborne NH, Birkmeyer JD, et al. Hospital characteristics associated with failure to rescue from complications after pancreatectomy. J Am Coll Surg. 2010;211:325–30.
den Dulk M, Noter SL, Hendriks ER, et al. Improved diagnosis and treatment of anastomotic leakage after colorectal surgery. Eur J Surg Oncol. 2009;35:420–6.
Acknowledgment
The authors would like to thank all surgeons, registrars, physician assistants and administrative nurses that registered all the patients in the DSCA, as well as the Dutch Surgical Colorectal Audit group.
Conflict of interest
The authors declare no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study is conducted for the Dutch Surgical Colorectal Audit Group. The study group members are listed in Appendix.
Appendix
Appendix
Study group members
The collaborators of the Dutch Surgical Colorectal Audit Group are W. A. Bemelman, D. Boerma, O. R. C. Busch, R. M. van Dam, J. W. Dekker, E. H. Eddes, E. van der Harst, M. L. E. A. Jansen-Landheer, Th. M. Karsten, J. H. J. M. van Krieken, W. G. T. Kuijpers, V. E. Lemmens, E. R. Manusama, W. J. H. J. Meijerink, H. J. T. Rutten, and C. J. H. van de Velde.
Rights and permissions
About this article
Cite this article
Henneman, D., Snijders, H.S., Fiocco, M. et al. Hospital Variation in Failure to Rescue after Colorectal Cancer Surgery: Results of the Dutch Surgical Colorectal Audit. Ann Surg Oncol 20, 2117–2123 (2013). https://doi.org/10.1245/s10434-013-2896-7
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-013-2896-7